7
Impacted Teeth and Resorption of the Roots of Adjacent Teeth
Prevalence
Aetiology, diagnosis and prevention
Treatment
Evidence-based answers to questions regarding canine-related incisor root resorption
Resorption in relation to vitality of the dental pulp
Invasive cervical root resorption
One of the essential characteristics of the deciduous dentition is that the roots of the teeth physiologically resorb with the development and progress of eruption of their permanent successors. This leads to a smooth transfer through the mixed dentition and on to the permanent dentition in the adolescent. In contrast, resorption of the roots of permanent teeth does not normally occur even when there are unerupted or crowded teeth in the close vicinity of these roots. Nevertheless, in relatively exceptional circumstances, pathological resorption of the roots of certain teeth can and does occur (Figure 7.1). The ‘aggressor’ teeth concerned are principally the maxillary canines and, to a much lesser extent, the mandibular third molars, which cause resorption of the roots of the maxillary lateral/central incisors and the mandibular second molars, respectively (Figure 7.2). Occasionally, too, one finds an aberrant mandibular second premolar developing low in the alveolus and with a strong distal tilt, with signs of resorption of the mesial root of the first molar (Figure 7.3). In each of these circumstances the crown of the impacted tooth is in close relation with the root of its neighbour – a situation not normally seen in other areas, where unerupted teeth are to be found at the level of the cervical area of the crowns of the adjacent teeth. Nevertheless, why resorption of the roots occurs routinely and physiologically in deciduous teeth and rarely and pathologically in these exceptional permanent teeth is not understood. Since resorption of the roots of permanent teeth has wide-ranging clinical implications, a discussion of the various aspects of this phenomenon is clearly warranted. The present chapter will deal mainly with the resorption of the roots of erupted permanent teeth by unerupted adjacent teeth in its most common location and where its clinical implications are also the most significant, namely the permanent canine/incisor area of the maxilla.
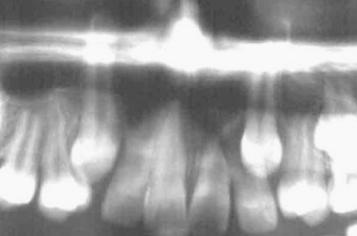
Fig. 7.1 An extreme case of resorption.
(Courtesy of Dr P. Svanholt.)
(a) Most of the root of the left central incisor has resorbed in response to the advancing unerupted canine in an 8.5-year-old female. On the right side, the central incisor shows considerable root resorption, which has arrested with the eruption of the right canine. The right lateral incisor is congenitally absent. (b) 16 months later the incisor is shed, following continued resorption. (c) The canine has erupted spontaneously in the position of the lost incisor. (d) Prosthodontic reshaping and restoration has made the canine more acceptable in its new role as an incisor.
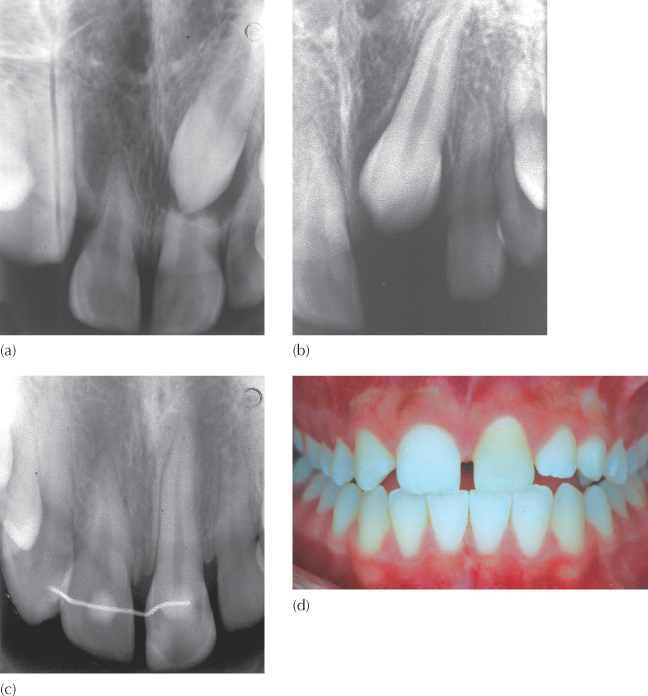
Fig. 7.2 Bilaterally impacted mandibular third molars associated with resorption of the roots of the adjacent second molars in an adult.
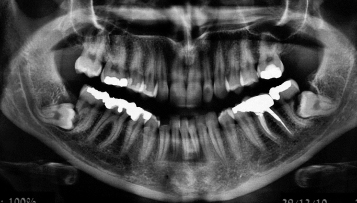
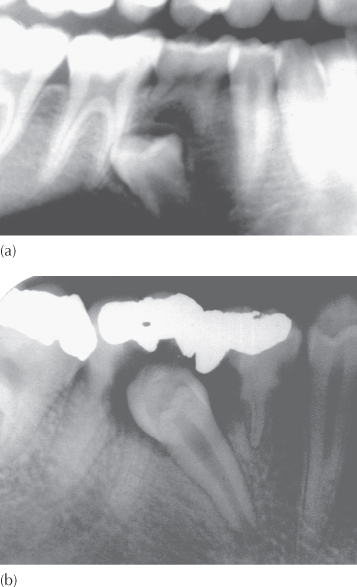
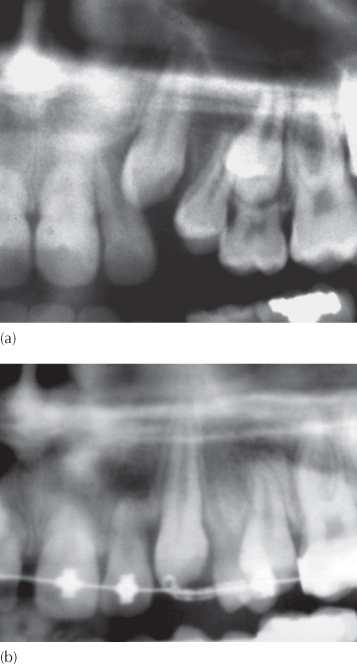
Fig. 7.3 (a) A section of the panoramic view of a female patient aged 12 years, showing a late-developing second premolar with a distal inclination. (b) A periapical view taken 2.5 years later. The second premolar has caused large-scale destruction of the first permanent molar.
Prevalence
Based on the use of plane film radiography, which was the standard of care in the late 1980s, early studies of the incidence of discernible root resorption of lateral and central incisors adjacent to an impacted maxillary canine revealed that 12% of the cases in the sample studied were affected [1–4]. While this finding in itself was alarming, the authors of the papers and others were at pains to point out that because of the limitations of plane film radiography, this figure was probably understating the extent of the problem [5–6]. It will be readily understood that an unerupted palatal canine is to be found closer to the palatal surface of the incisor roots than to any other surface of the root and, should there be root resorption of the incisor, it is logical to assume that it will be palatal surfaces that are most likely to be affected. By the same token, a buccal canine may cause similar damage to the labial surface of the root of the adjacent incisor. Furthermore, because the canine generally approaches the root of the incisor from above and along a path which is at an angle to the long axis of the resorbing incisor, the resorption process usually affects the incisor roots obliquely. However, the labial and palatal surfaces of the roots of the teeth are largely impossible to image using traditional plane film radiography. It is these palatal and labial root surfaces which, if affected by resorption, are least likely to be recognized in plane film radiography until the extent of the lesion is sufficiently well advanced for it to alter the mesio-distal profile of the root or the relative radiolucency of its projected shadow.
In line with technical progress in the development of diagnostic radiology, computerized tomography (CT) presented the window of opportunity that could overcome this bucco-lingual imaging ‘blind spot’, as discussed in Chapter 2. Accordingly, when a similar study of root resorption was undertaken by the same researchers [7], this time using spiral CT scanning in place of the earlier plane film radiography, it revealed signs of root resorption in almost half the cases affected by an aberrant/ectopic and unerupted maxillary canine. The actual figures in this study showed 38% of lateral incisors and 9% of central incisors affected to a greater or lesser extent, or 47% of affected individuals, in total. In a more recent study, in which the imaging modality used was cone beam three-dimensional volumetric CT, the figures were higher still, with 66.7% of adjacent lateral incisors and 11.1% of adjacent central incisors affected (Figure 7.4). All those cases which exhibited central incisor resorption also showed resorption of the lateral incisors and in all the cases in the study close proximity between the impacted tooth and the incisor root was found [8].
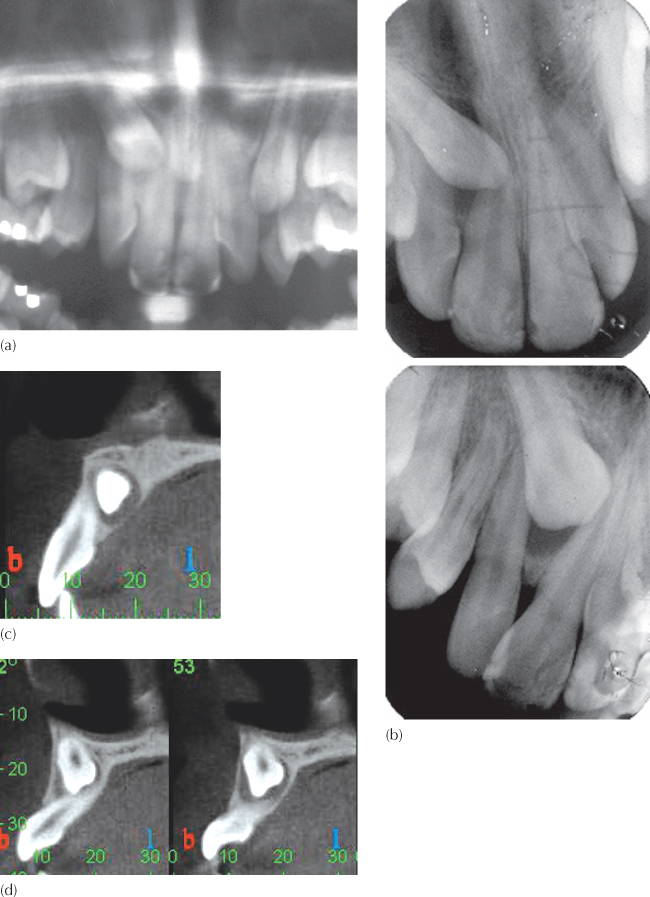
Fig. 7.4 A case for double misdiagnosis.
(Courtesy of Dr N. Dykstein.)
(a) A section of a panoramic view showing the right impacted canine superimposed on the lateral and central incisors. There is no apparent resorption of the incisor roots and the canine is palatal according to Chaushu’s method (see Chapter 2). (b) Two periapical views, with lateral tube shift intended for positional diagnosis, show the crown of the canine to be palatal to the central incisor root and no apparent root resorption. The canine is clearly palatally impacted. (c) From the CBCT images, a single paraxial cut of the canine and central incisor relation shows marked oblique and palatal resorption of the incisor root, and the canine can be confirmed to be on the palatal side of the central incisor. (d) From the CBCT images, two parallel paraxial (vertical antero-posterior) cuts, at an interval of 1.5 mm, of the canine and lateral incisor relation show marked oblique and labial resorption of the incisor root. The canine is on the labial side of the lateral incisor.
Of course, in a significant proportion of the impacted canine patients in whom root resorption has occurred, these canines will eventually erupt and the roots of the incisors may suffer little or no further resorption in the long term (see Figure 6.34i, j). The eruption may be generated by a spontaneous change in the orientation of the canine in relation to the affected incisor root, as has been shown in anecdotal case reports [9] or during orthodontic treatment to create space for the canine by an appliance-generated movement of adjacent teeth [10, 11] as described in Chapter 6 (see Figure 6.19) or by the prophylactic extraction of deciduous [5, 12, 13] or permanent teeth (see Figures 6.19, 6.20).
Aetiology, Diagnosis and Prevention
Over the years, clinicians have searched for clues, specific tell-tale features, which may indicate a high risk for incisor root resorption associated with an impacted canine. Obviously, the mobility of an incisor, in the absence of any signs of premature contact or symptoms of pain, would offer such an indication after the fact. However, the quest was for an associated anomaly or phenomenon in the dentition that could predict the occurrence of incisor root resorption before it occurred.
Two studies that have investigated sexual dimorphism as a factor in the prevalence of this phenomenon have found that it occurs 3–4 times more frequently in females than in males [3, 8]. In relation to those cases in which the resorption has been extensive, accounting for more than a third of the incisor roots, both published individual and multiple case reports in the orthodontic literature and the author’s clinical experience indicate that, in its severest form, the phenomenon may be almost completely limited to females [14]. However, caution should be exercised in this regard since no formal study has been made of these more advanced resorption cases in contrast to those that may be minimally affected or where the extent of the damage is clinically insignificant.
Suspicion regarding the presence of an enlarged dental follicle surrounding the impacted canine is another factor that has been investigated. Two studies have been performed by the same Swedish group and they found there to be no apparent cause-and-effect relation between an enlarged follicle and root resorption [3, 15]. Notwithstanding, other clinicians have expressed concern regarding a possible cause-and-effect relation between an enlarged follicle and root resorption [16, 17].
In light of the potential seriousness of the condition in the more extreme expression of its occurrence and its very much higher prevalence among females, this concern should be heeded, care taken and caution advised in the clinical context, despite the absence of confirmatory investigative studies. Good anecdotal examples of this may be seen in Figures 7.5, 6.15 and 6.36 and 7.10b, where unambiguous evidence of advanced root resorption of the incisor is seen adjacent to an impacted canine which is encompassed by an enlarged dental follicle. By and large, the overwhelming majority of cases where resorption has been confirmed show only a very mild and clinically insignificant degree of root loss, which at least partly explains why the condition requires the use of CT for the diagnosis to be determined definitively. However, it should also be remembered that all severely affected cases began the pathological process to this advanced state with very small initial resorption lesions which, had they been diagnosed earlier, may have markedly improved the prognosis.
Fig. 7.5 An enlarged follicle associated with severe resorption of the left lateral and central incisor teeth, in a 10-year-old female patient.
As we have pointed out in Chapter 6, a number of studies relating to the aetiology of palatal canine impaction have been published over the past 20 years, and these have established a firm link between palatally displaced maxillary canines and anomalous lateral incisors. However, when the prevalence of resorption of an incisor adjacent to a palatal canine was investigated, anomalous incisors appeared to be relatively immune to resorption. The phenomenon was found to be much more frequently associated with a normal-sized adjacent lateral incisor [6]. The conclusion drawn from this study was that the practitioner would be well advised to investigate the possible existence of resorption in any impacted canine patient who shows no lateral incisor anomaly. This is, therefore, a factor to be taken into consideration in deciding the strategy of the orthodontic treatment and the timing and sequencing of the individual tasks within the overall treatment plan.
Treatment
When the diagnosis of impacted canine-related resorption of the incisor root is made, a lack of positive action on the part of the orthodontist or surgeon carries with it the danger of further resorption of the root of the incisor, for which these two practitioners may justifiably be held responsible. Furthermore, for as long as the impacted tooth remains in close proximity to the resorbing root, its continued destructive nature remains undeterred by any initial orthodontic alignment and space-gaining procedures that may be under way. The resorption process seen in many of these cases is rapid and it has been shown conclusively that it will advance significantly during the preparatory orthodontic phase [14]. On the other hand, and as has been pointed out earlier, the creation of space in the arch by moving the adjacent teeth, one or more of which are themselves being actively resorbed, might be a factor that may change the course of the canine, causing it to move away from the area and spontaneously erupt (Figure 7.6).
Fig. 7.6 Root resorption, space opening and spontaneous eruption. (a) The left impacted canine has caused a marked oblique resorption, which has shortened the root in general and its distal side in particular. The central incisors have short rounded roots. (b) Following the orthodontic creation of space, the canine is seen to be erupting spontaneously.
Treatment Options
Three possible lines of treatment are available, and each has its advantages, disadvantages, unanswered questions and manner in which it influences the outcome.
Extract the Impacted Tooth
First principles in medicine dictate that, in order to successfully treat a disease, it is first necessary to remove the cause. In the present context, the cause of the resorption is the unerupted tooth, and its extraction carries with it the bonus of eliminating what may be a problematic impaction from the point of view of the provision of surgical access and the mechano-therapeutic difficulty. If this apparently logical line of treatment is followed, then a healthy canine will be extracted and the incisor with the resorbed root will be left in place. There is uncertainty as to whether the resorption process will continue and, in this compromised state, it may be reasonable to assume that the tooth has a reduced long-term prognosis. Given that it is unlikely that the incisor is in its ideal position and will thus need to be orthodontically moved into alignment, we need to know if the orthodontic treatment prescribed to achieve this will generate further resorption, potentially adversely affecting its prognosis still further. If an implant may be planned as the ultimate substitute for the extracted canine, considerable root movement of the resorbed lateral incisor will probably be mandatory in order to provide adequate space between the roots of the adjacent teeth. Alternatively, it may be wiser to attempt space closure. This would increase the length of time that orthodontic forces will need to be applied to this endangered tooth in its capacity as an anchor unit, and it may finally need to be splinted. Although it could be argued that perhaps a fixed cast bridge might reduce the amount of orthodontic movement to which the tooth will need to be subjected, it should not be forgotten that a resorbed lateral incisor will not make a good abutment. With a premolar in the canine position, the appearance may be compromised, and canine protection of the occlusion would not be present.
Leaving the deciduous canine in its place, in the hope of its enjoying long-term survival in the present situation, is a real possibility. Given the degree of displacement of the aberrant canine, it is quite likely that the root of the deciduous canine has remained untouched by the normal resorption process affecting deciduous teeth, and, in these cases, the tooth may last for many years before implant and/or prosthetic replacement is needed. However, if its position needs to be altered, to enable the placement of an appearance improving restoration, then perhaps the required orthodontic movement may trigger the physiological resorption that has not occurred.
Extract the Resorbed Tooth
Extracting the ‘victim’ tooth may appear unfair, but must be considered the pragmatic choice if it is to be assumed that it has a poor prognosis. By its extraction, the treatment of the impaction is much simplified. Whether the deciduous canine will also be lost in the overall long-term planning strategy or not, the permanent canine would be aligned in the lateral incisor site, with the accompanying poor appearance and lack of a canine-protected occlusion [18]. To address the appearance, some orthodontists, prosthodontists and ‘aesthetic’ dentists might prefer aligning the impacted canine in its normal place in the arch, performing a one-tooth implant to replace the lateral incisor and to achieve a more normal, uncompromised appearance [19, 20].
Non-Extraction
This is perhaps the most difficult and most heroic line of treatment, the more so since the literature offers little evidence for us to believe that the outcome can provide hope for a stable future. In the first place, without the expedient of extraction, the canine impaction is much more difficult to resolve since the tooth will need to be surgically exposed, attachment bonded and drawn away from the resorbing root in a separate orthodontic manoeuvre and before the more usual directional forces may be applied to bring it to its place in the arch. Second, the lateral incisor has a shortened root and will almost certainly require to be moved orthodontically. It may need to be splinted for the duration of its presumably reduced lifespan. Third, this incisor may become non-vital as a complication of the surgical exposure and may subsequently require root canal treatment. These factors appear likely to reduce its long-term prognosis still further. On the other side of the scale, it has been noted in the previous chapter that most palatally impacted canines and a minority section of the buccally ectopic canines are to be found in conditions of spacing and the mildest malocclusion, which may generally be considered to be non-extraction cases. Therefore, this approach potentially offers the prospect of the greatest gain for the patient and, if carefully managed, perhaps provides a way in which our worst fears will not be realized.
It has been proposed that there is a fourth alternative in this situation – a ‘masterly inactivity’ or ‘wait-and-see’ option. An anecdotal series of three cases has been reported in which severe resorption of incisor roots had been noted adjacent to impacted maxillary canines, in each case [9]. The patients were followed up clinically and radiographically for a long period on a half-yearly recall basis, without treatment of any sort being provided. The canines eventually erupted, although the progress of the spontaneous resolution of the impaction generated further root resorption. It is a sine qua non that additional damage to the roots of the adjacent incisors was fully anticipated at the outset in these three patients, although the full extent of its expression could not be predicted. It is therefore reasonable to assume that the significant risk that these teeth would be lost during this observation period was accepted as a conscious decision. The dilemma that faced the clinicians was whether more damage would have been inflicted iatrogenically had the impacted teeth been treated by the orthodontic/surgical modality.
It is germane to attempt to answer this question in relation to group 6 impacted canines in general. To do so, it becomes necessary to examine the anatomical, surgical and orthodontic contexts of the dilemma and discuss the several factors that need to be carefully evaluated.
The Anatomical Context
The first factor addresses the anatomical relationship between the impacted tooth, the resorbing tooth and their location in the alveolar process. In general, and having been the first to erupt some 3–4 years earlier, the adjacent incisor tooth is sited in mid-alveolus in the bucco-lingual plane. The impacted canine generally follows a high and mesially angulated path towards the root of the incisor. The approach of a palatal canine is on the distal or disto-palatal aspect of the root of the incisor, some way down the root from the apex (Figure 7.6a), while a buccal canine will be on the disto-labial side. Resorption occurs in the immediate area of the proximity of the two, and will only be discernible radiographically if it also affects the distal profile of the root of the incisor and is not hidden by the superimposition of the two teeth.
In the most extreme cases, which are the context of the present discussion, the canine does not ‘side-swipe’ the root of the incisor, but rather comes down from above its apex, obliquely resorbing most of the full width of the root as it progresses inferiorly into the area vacated by the resorbing root (Figure 7.1) The canine is also thus situated in mid-alveolus. In one scenario, further progress finds the incisor root being resorbed obliquely with the destruction proceeding coronally at an alarming rate, until the crown of the still unerupted canine reaches one side of the cemento-enamel junction (CEJ) of the incisor. At this point, no further resorption can take place, since the enamel of the tooth crown will not resorb but will act to deflect the progress of the canine to one side, where it may then erupt. The incisor does not then shed naturally, since the oblique resorptive process will have left a longish spicule of root which will hold the tooth in the alveolus, although the tooth may (but not necessarily) become a little mobile. The incisor crown is also likely to be displaced in the opposite direction to the canine’s new eruptive path due to the eruptive force of the latter acting obliquely on one side of the incisor’s CEJ.
The Surgical Context
If we are to try to change the course of what appears to be inevitable, it is logical to attempt to distance the canine from the resorption area as early as possible, which is immediately after the diagnosis has been established. In the orthodontic/surgical modality of treatment, this means that surgical access must be provided and an attachment bonded in order that orthodontic forces may be applied direct to the tooth to effectively draw it away from the immediate area by diverting it from its present path.
Because of the intimate relationship between the crown of the impacted tooth and the resorbing root apex of the incisor, accuracy of positional diagnosis is vital, if simultaneous collateral surgical damage to the root area of the incisor tooth is to be avoided. A wide flap is reflected, the crown of the impacted tooth is identified immediately beneath its thin bony covering and only the smallest opening is made in the bony crypt to expose that area of the crown of the impacted tooth most superficially accessible and most distant from the resorption site. No attempt should be made to seek out the root apex of the incisor, or even to gently probe the area (Figure 7.7).
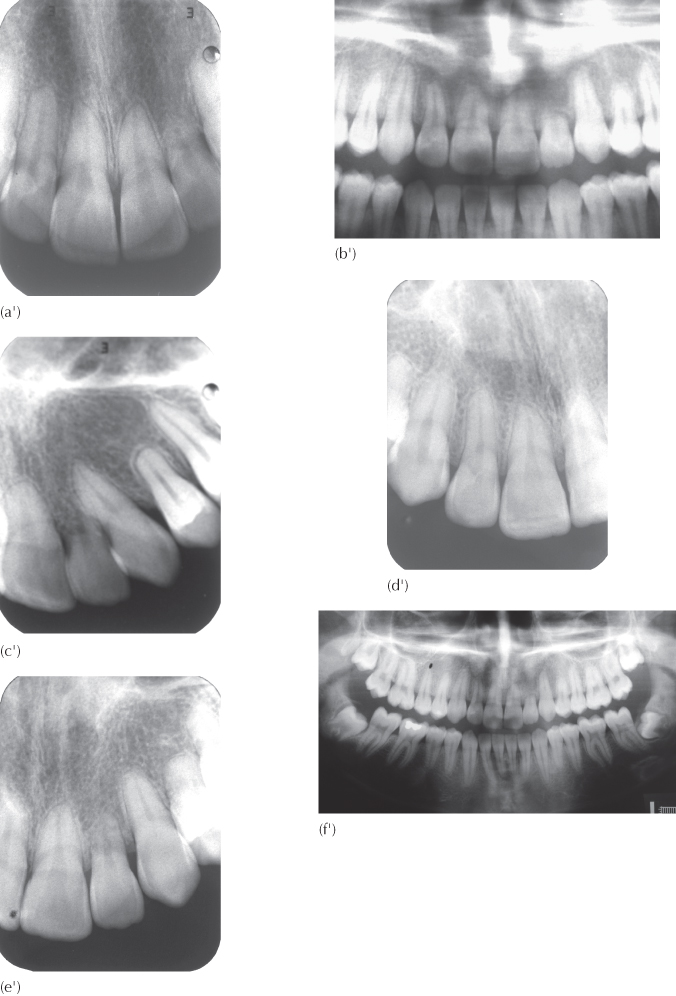
Fig. 7.7 This case was treated before the introduction of cone beam computerized tomography. (a–e) Initial clinical intra-oral views of the dentition. Note deciduous left maxillary canine in place and space loss in the left mandibular quadrant following early extraction of the deciduous second molar. (f) Section of the lateral cephalogram to show a single labially ectopic maxillary canine. (g) A section of the panoramic view shows the canine to superimpose on the lateral incisor root. It appears that most of the root of the lateral incisor has been resorbed. (h, i) The periapical views confirm labial impaction. (j) Surgical exposure is minimal to reveal only the disto-labial aspect of the tooth. The camera angle shows the canine to be in the same long axis of the incisor, obviously moving into the freshly resorbing area as it develops. (k) An eyelet is bonded to the disto-labial corner of the crown of the tooth. Its pigtail ligature is seen to hang loosely. Traction cannot be made direct to the archwire, for fear of resorbing more of the incisor root. (l, m) An open surgical exposure is strongly contraindicated here, since it would leave the sensitive apical area of the incisor exposed. Full flap closure is made to cover the entire exposed area, with the pigtail ligature taken through the oral mucosa, high up in the sulcus. In this situation, it cannot be taken through attached gingiva. The long loop of the light auxiliary labial archwire lies horizontally, in its passive state, ready for activation. (n, o) The loop is flexed upwards and engaged by the pigtail ligature, which ensnares it. This produces a light and highly controllable labial force to move the unseen canine. (p) At one month post-surgery, the tooth has exited the oral mucosa. (q) At two months post-surgery, the tooth has cleared the root of the lateral incisor and a distal direction of traction is applied, with a measured piece of cut tubing holding the space between incisor and premolar. The disto-labial position of the eyelet permits this movement without incurring unwanted rotation. (r, s) At three months post-surgery, the tooth has moved opposite its place in the arch and a regular bracket is substituted, in preparation for the finishing phase of treatment. (t) At five months post-surgery, finishing procedures are in progress. (u) Periapical radiograph checking for the status of root resorption indicates considerably more root than realized at the outset. The appearance is typical of an oblique resorption, in which the labial side of the tooth has been ‘shaved’ off, leaving a long spicule of palatal root. (v–z) The final clinical result. In view of the severity of the resorption process, meticulous attention to root uprighting and torqueing was considered inappropriate at the time. (a’–f’) Periapical and panoramic views of the immediate area, at the end of treatment. (g’–i’) Patient seen 7.6 years post-treatment. (j’, k’). Periapical and panoramic views of the dentition 7.6 years post-treatment, showing no change in the condition of the root of the resorbed lateral incisor. There is no hypermobility of the tooth and the removable retainer was discarded three years ago.

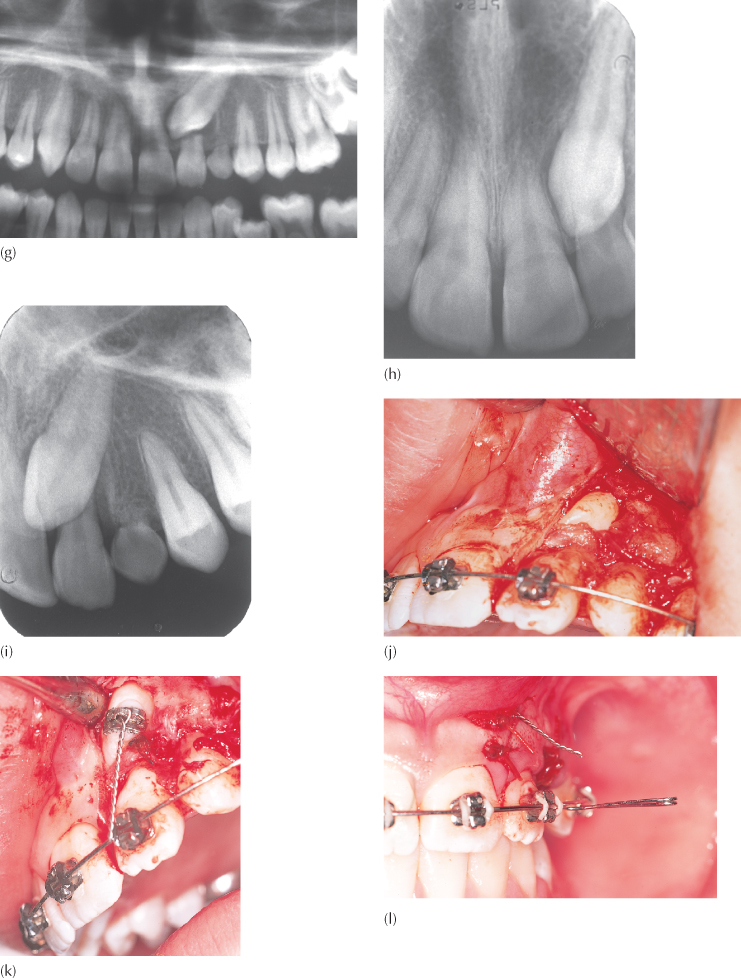


It will be appreciated that a good radiographic diagnostic technique, specifically CT views employing a cone beam volumetric machine, should be considered an essential diagnostic aid that will contribute enormously to determining the preferred exposure site as accurately as possible. From these, the direction in which the tooth must be moved away from the sensitive resorption area will be decided. This may be in a labial direction or in a palatal direction, depending on the labio-lingual location of the crown tip vis-à-vis the residual root end.
Exposure of the crown, clearance of the follicle and bone removal to the maximum width of the crown and down to the CEJ in this situation, as recommended by Kokich for the more accessible palatal canines [19], is strongly contraindicated in these cases, since it will surely inflict unnecessary trauma to the resorption area and lead to devitalization of the incisor.
In these highly sensitive situations it is recommended that the area of crown to be exposed should be on an aspect of the crown as far as possible from the site of resorption. It should be exposed minimally, with an opening only large enough for placement of the small eyelet, while permitting adequate haemostasis during the bonding procedure (Figure 7.7j, k).
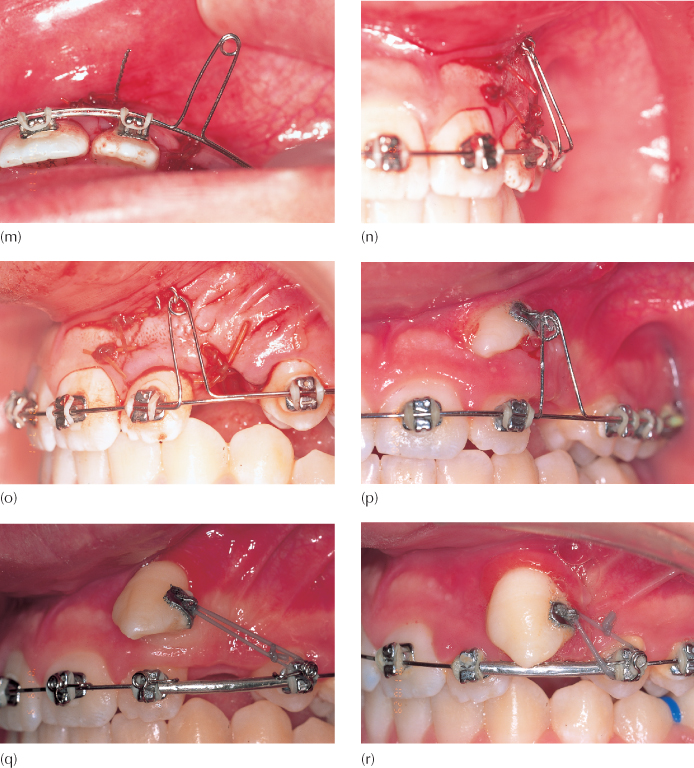
An eyelet attachment is then bonded to the tooth in the most accessible site available on the crown surface, and the twisted steel ligature is made to point in the direction that traction will be applied. The full flap is then sutured back to its former place, leaving only the ligature wire peeking through it, either at the sutured edge or, preferably, to piercing through the flap in the direction that traction has been determined. Primary closure is essential in these cases to protect the wound from damage or infection of the vital tissue at the root end of the lateral incisor. If, following the earlier resorption, the canine crown tip has crossed over to the labial side of the incisor roots, a labial resolution will be required (Figure 7.8). In this case, labial traction will be needed, and this will mean that a labial surgical approach will be preferred, with the attachment bonded in a convenient place on the crown and its ligature protruding through the flap, high in the labial sulcus. If the tooth is palatal, a palatal approach will be dictated, with the palatal aspect of the tooth being exposed and an attachment bonded there. Traction will need to be directed in the horizontal plane in a posterior horizontal direction.
Fig. 7.8 (a, b) Periapical views of the group 6 canine with associated severely resorbed central incisor. (c) A variant of the auxiliary labial arch to move a tooth buccally. The loop is drawn upwards and into the sulcus to ensnare the pigtail. (d) Four weeks later, the pigtail has elongated, indicating progress of the canine. (e) After several adjustments over a three-month period, the eyelet attachment of the canine becomes visible. (f, g) Clinical a/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


