7
Endodontics
In an endodontic emergency, diagnosis should include not only any endodontic considerations, but also periodontal and restorative considerations, along with a differential diagnosis for those instances when the pain may not be of an endodontic origin. Definitive treatment (ie, endodontic therapy versus extraction) is based on a thorough analysis of the long-term restorative and periodontal prognoses for the tooth.
Managing an endodontic emergency not only consists of treatment, but may, more appropriately, consist of referral, should the diagnosis be questionable. It is prudent to delay irreversible treatment when the diagnosis is unsure. In the case of a bona fide endodontic emergency, the rule of thumb is, the more that can be accomplished at the emergency visit (ie, pulpotomy versus analgesics, pulpectomy versus pulpotomy), the better the potential for pain relief. An emergency that is a result of periradicular inflammation or infection requires cleansing of the pulp canal. Antibiotic the ra pyshould be considered for patients who have signs and symptoms of infection, such as cellulitis, fever, or lymphadenitis.
Irreversible Pulpitis
Irreversible pulpitis occurs when prior insults to a tooth lead to focal areas of inflammation or necrosis within the pulp. Pain results not only from dentinal tubule fluid flow, but also from elevation in intrapulpal tissue pressure. Increased intrapulpal pressure lowers the threshold of pulpal nerves such that normally subthreshold stimuli can cause pain, more severe stimuli causes pain with slow or delayed recovery, or spontaneous pain can occur.
Diagnosis
Pulpal tests show a strong or severe response to thermal stimuli with delayed recovery. Long-standing inflammation may be evidenced by both a delayed response to hot stimuli and/or a delayed recovery. Electric pulp testing is positive, usually responding at a lower reading than normal teeth. Percussion and palpation sensitivity should be absent except when the periradicular tissue has been irritated as a result of occlusal trauma or the inflammation is long-standing. The pain may be described as mild to severe, continuous or intermittent, diffuse or localized. Referred pain to other head and neck structures or to other teeth is very common.
Clinically, check for evidence of decay, a faulty restoration (fractured or open margin), cuspal or coronal fracture, unprotected dentin, or evidence of trauma. Teeth with an extensive restorative history are likely candidates for developing irreversible symptoms.
Radiographically, look for decay, bone loss exposing root surfaces, or tooth fracture. A tooth that has been pulp capped should be tested for abnormal responses. The periradicular tissues should appear normal with the possible exceptions of a widened periodontal ligament (PDL) space (Fig 7-1) or condensing osteitis. Both signify the presence of low-grade infection in the pulp.
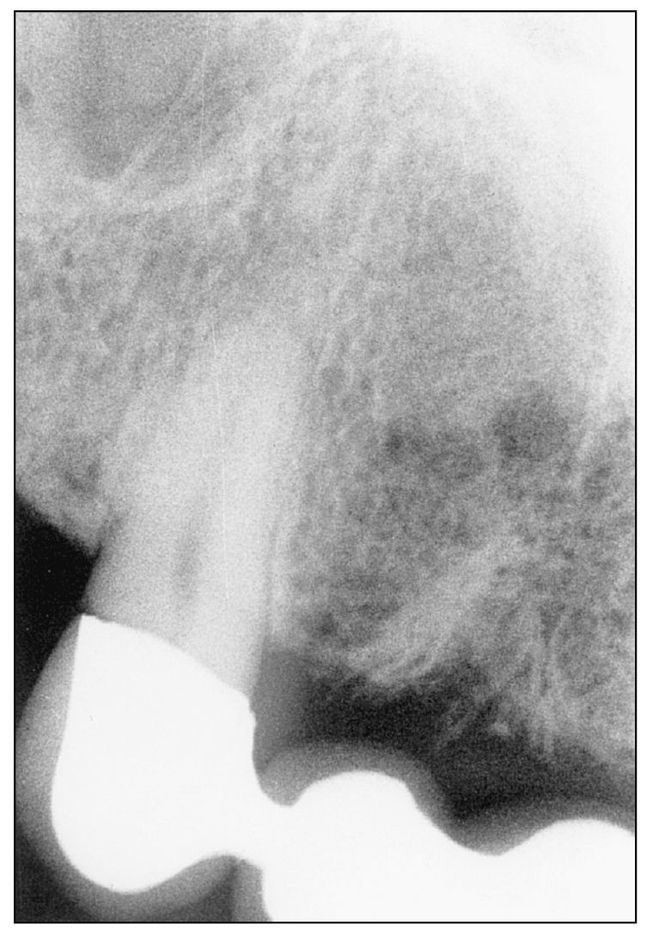
Fig 7-1a Normal PDL space.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


