Tooth Extraction and Site Preservation
Alveolar Bone Healing After Tooth Extraction
Scientific Validation for Site Preservation
Surgical Techniques for Minimally Invasive Tooth Extraction
Surgical Techniques for Site Preservation
Prosthetic Manipulation of Soft Tissues During Healing
Clinical Outcome Analysis of Alveolar Preservation Techniques
At the conclusion of this chapter, the reader will be able to:
 . Understand the basic physiology of extraction defect healing and the benefits of site preservation in altering that response.
. Understand the basic physiology of extraction defect healing and the benefits of site preservation in altering that response.
 . Describe the surgical techniques and biomaterials needed to perform atraumatic tooth removal and site preservation.
. Describe the surgical techniques and biomaterials needed to perform atraumatic tooth removal and site preservation.
 . Explain the extraction defect sounding classification system and the associated treatment algorithms.
. Explain the extraction defect sounding classification system and the associated treatment algorithms.
 . State the limitations of site preservation and the circumstances in which advanced surgical procedures are necessary.
. State the limitations of site preservation and the circumstances in which advanced surgical procedures are necessary.
Dental implants are quite often the treatment of choice for the replacement of lost or missing teeth. Implant treatment is extremely predictable for partially as well as completely edentulous clinical conditions, and long-term survival rates of 85% to 100% have been reported.1 The challenge today in implant dentistry is no longer just to achieve osseointegration, but also to attain balance and harmony between the implant restoration and the surrounding soft tissues (Figure 6-1). This is especially true in the esthetic zone.
The loss of a tooth commonly leads to hard and soft tissue alterations that challenge ideal implant placement, soft tissue esthetics, and long-term peri-implant tissue management. Tooth extraction is a traumatic surgical procedure that can result in immediate loss or fracture of alveolar bone. Soft and hard tissues are commonly traumatized during tooth extraction, compromising tissue esthetics. Damage to marginal bone may lead to recession of the marginal gingiva and coronal elongation of an implant restoration (Figure 6-2). Damage to the interproximal bone may lead to papilla shrinkage and the formation of interproximal “black triangles” (Figure 6-3) or force alteration of the restorative contact points, making restorations look bulky.
Physiologic wound healing after extraction is associated with morphologic alteration of the alveolar bone and soft tissue. Clot contraction in the socket leads to a reduction of alveolar bone width and height. An experimental study that evaluated morphologic changes in the alveolar process after tooth extraction showed an average loss of 2 mm of bone width. Soft tissue invagination in the socket leads to incomplete bone fill and reduction of alveolar bone height.2–4 The loss of crestal bone height ultimately leads to a vertical soft tissue deficit and a compromised esthetic result. In these situations the implant platform often must be placed more apically than is ideal for a proper emergence profile, which leads to the development of deeper peri-implant probing depths; this development compromises home care and long-term management of the peri-implant tissues and increases the risk of peri-implant disease.5 However, the loss of alveolar bone height and width can be minimized and very often prevented through the incorporation of site preservation procedures at the time of tooth extraction.
Alveolar Bone Healing after Tooth Extraction
The healing of an extraction socket after tooth removal has been well studied in both animals and humans.6 Studies in animals demonstrate that during the process of healing, a series of events occurs. It begins with the formation and maturation of a blood clot and proceeds to infiltration of fibroblasts to replace the coagulum and eventual establishment of a provisional matrix that allows for bone formation. In an experimental animal study, Araujo and Lindhe2 noted that resorption of the buccal and lingual plates occurred after tooth removal. This resorption occurred in two phases. In phase I the bundle bone was resorbed and replaced with woven bone, leading to a substantial vertical reduction of the crest. In the second phase, resorption occurred from the outer surfaces of both bone walls. This ultimately led to a loss of ridge width. In a follow-up study by the same authors,7 the effect of flap elevation on alveolar ridge dimension was examined. The authors concluded that flap elevation had very little or no effect on the alveolar process. These studies suggest that alveolar ridge resorption is a physiologic outcome directly caused by tooth removal.
In a study by Schenk and Hunziger,8 the alterations seen after tooth extraction were attributed to a decreased blood supply to the alveolus, which led to osteocyte cell death and necrosis of the surrounding tissue. In a further phase of healing, the necrotic bone may be gradually eliminated through surface resorption by osteoclasts in the periosteum. Additional factors related to these alveolar bone changes may be an adaptation to continued lack of function at the extraction site and tissue adjustment to meet genetically determined demands on ridge geometry in the absence of teeth. In a human study by Schropp et al.,9 bone and soft tissue dimensions were examined after tooth extraction. The authors found that the width of the alveolar ridge was reduced by 50% during the 1-year observation period. Most of these changes (approximately two thirds), occurred within the first 3 months after tooth extraction.
Scientific Validation for Site Preservation
In a 6-month randomized, controlled, blinded clinical and histologic study in humans, Iasella et al.10 examined 24 patients who underwent extraction and then implant placement.10 The aim of the study was to determine whether ridge preservation procedures would prevent postextraction resorption. Tetracycline-hydrated, freeze-dried bone allograft (FDBA) was placed in extraction sockets, and the grafts were covered with a collagen membrane. The authors concluded that ridge preservation improved ridge height and width dimensions compared with extraction alone. The mean width of preserved sites decreased by 0.8 mm, compared with a decrease of 2.7 mm in nonpreserved sites (a statistically significant finding). Most of the resorption was noted on the buccal aspects, and maxillary sites lost more width than did mandibular sites. Vertically, the preserved sites gained approximately 1 mm, compared with a loss of 1 mm in nonpreserved sites. A height difference of 2.2 mm was reported, which was statistically significant. However, the study also revealed a disadvantage of site preservation: the use of FDBA resulted in less bone by volume in the extraction defect, approximately 28% in the preserved sites compared with 54% in the nonpreserved sites. This was predominantly the result of the presence of residual graft particles.
In a 6-month split mouth study in the dog using bovine collagen (Bio-Oss), Araujo and Lindhe11 histologically noted better dimensional integrity of the alveolar process compared with nonpreserved sites. The authors found that the bovine collagen served as a scaffold for tissue modeling. However, as in the study by Iasella et al., the procedure did not enhance bone volume. Araujo and Lindhe11 concluded that placement of a biomaterial in an extraction socket may modify modeling and counteract marginal ridge contraction that naturally occurs after tooth removal.
In a histomorphometric evaluation of mineralized cancellous allograft (Puros) covered by a bioabsorbable collagen dressing in human extraction defects, Wang and Tsao12 noted favorable bone growth in the extraction defects.
These studies suggest that the benefits of site preservation procedures are not material specific. Multiple graft materials have been used successfully for site preservation. However, some materials may work better than others.13 The benefits of adding a graft material to a fresh extraction socket derive from an alteration in healing through the occupation of space by the graft material, which improves clot stability and reduces clot shrinkage and contraction.
Surgical Techniques for Minimally Invasive Tooth Extraction
Site preservation has been shown to significantly improve alveolar ridge height and width by minimizing physiologic alveolar shrinkage associated with tooth removal.14 However, the surgical procedure for removing a tooth can easily lead to a much more significant amount of tissue loss in a matter of minutes. Fracture of the alveolus, bone removal with the extracted tooth, and trauma to the soft tissues all are complications related to exodontia that can lead to significant hard and soft tissue deficits. This type of damage is also extremely difficult to repair predictably. Therefore, preventing such trauma and performing minimally invasive extractions are critical for sites that require minimal alveolar changes after tooth removal. Minimally traumatic tooth extraction should be considered the first step for successful site preservation. The following procedures are beneficial for all extraction sites but crucial in the esthetic zone15:
Esthetic Evaluation
Before removing a tooth, the dental practitioner should perform a soft tissue evaluation that focuses on esthetics and document the details. This is extremely important when dealing with extractions in the esthetic zone or any extraction in a patient who is esthetically demanding or particular. The evaluation should document the smile line (Figure 6-4) to determine the extent of gingival display; the gingival margin positions of the adjacent teeth, with notations of any asymmetries; and the condition of the interproximal papillae (Figure 6-5). The size, shape, and form of the papillae are important to recognize and document, because this can help preclude or minimize loss of interproximal papillae. Loss of the interproximal papillae often leads to the formation of interproximal spaces commonly referred to as “black triangles.” A thorough esthetic evaluation before tooth removal allows the practitioner to discuss expected healing outcomes accurately with the patient and to predict the alteration to the soft tissues.
Biotype Analysis
Recognition and documentation of the patient’s periodontal biotype are important for predicting hard and soft tissue healing; this also allows modification of the surgical procedure, when indicated, to enhance esthetics.16 An understanding of the biotype is extremely important for patient communication and expectations. In a clinical study, two basic tooth forms were observed and correlated with various soft tissue clinical parameters, leading to the description of two discrete periodontal biotypes (Figure 6-6).17
The thick, flat periodontium is associated with short, wide tooth forms. This biotype is characterized by short, flat interproximal papillae; a thick, fibrotic gingiva that is resistant to recession; wide zones of attached keratinized tissues; and thick underlying alveolar bone that is resistant to resorption.18 Wound healing is ideal in this type of periodontium, because bone resorption and soft tissue recession are minimal after surgical procedures, including extractions and dental implant surgery. Ideal implant soft tissue esthetics can be predictably achieved in patients with this biotype.
In contrast, the thin, scalloped periodontium is usually associated with long, narrow, triangular tooth forms. This biotype is characterized by long, pointy interproximal papillae; a thin, friable gingiva; minimal amounts of attached keratinized tissues; and thin underlying alveolar bone that is frequently dehisced or fenestrated.18 After surgical procedures, marginal and interproximal tissue recession in conjunction with alveolar resorption can be expected in patients with this biotype.16 A careful, minimally traumatic extraction technique performed with microsurgical instruments is necessary in these patients to help preserve the alveolar architecture.
Minimally Traumatic Exodontia
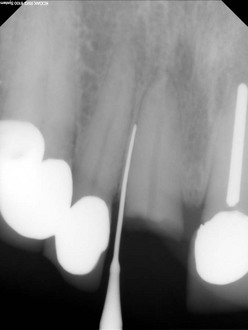
As continued apical pressure is exerted, the periotome is inserted into the periodontal ligament space along the root surfaces, severing the periodontal ligament directly below the alveolar crest. This process is continued until the periotome penetrates to a depth sufficient to initiate tooth mobility (Figure 6-7). Quite often a surgical mallet is used to facilitate the process. Once the tooth is sufficiently mobile, conventional extraction forceps can be used with rotational force to gently remove the tooth, without the need for further luxation and associated trauma. The use of a periotome is limited to the interproximal and palatal aspect of a tooth. To preserve the integrity of the buccal plate, the buccal tooth surface is avoided when a periotome is used; this helps maintain the integrity of the gingival margin, which is critical for an optimal esthetic result. The disadvantages of using a periotome include fatigue and an increase in the time needed to accomplish the extraction procedure.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses