6 The Practice of Dentistry
PRIVATE DENTAL PRACTICE
Traditionally dental care in the United States has been delivered by independent private practitioners. The American Dental Association (ADA) estimated that approximately 93% of all active dentists were in private practice in 1998.15 This proportion has remained remarkably stable over the years. Indeed, an essential feature of dental care delivery in the United States is the diversity of practice modes and their constant evolution within a private practice philosophy. Adaptability in a rapidly changing world is a major strength of private practice, an attribute that ensures that private practice will endure.
Private practice has a number of inherently desirable features. One advantage to both provider and patient is flexibility. Dental practitioners can provide care for as many hours per day and for as many days per year as they choose. When demand for care in a locality increases, private practitioners can respond if they wish by working longer hours, by increasing their productivity to meet it, by increasing their fees, or by all of these. There is a built-in economic incentive to be as efficient as possible in private practice, because it represents a big investment of private capital in facilities and equipment; the return on that investment is the practitioner’s profit. Choice of equipment, materials, and employees therefore is made carefully, and all can be chosen to suit the tastes of the individual dentist.
Private practice has often been equated with free choice of a dentist by the prospective patient and, conversely, with freedom of the dentist to treat or not to treat anyone seeking care. Whether these concepts were ever fully true is arguable, but it is certain that current circumstances put some limits on these freedoms. In many inner city or small rural communities, for example, there is often little choice of dentist because dentists are less likely to establish practices there. Because dentists in private practice are self-employed business people, they tend to establish their practices in localities where they can be reasonably sure of adequate demand for their services; these localities are typically higher-income suburban areas. There is a clear association between the availability of dentists and the per capita income of an area.7,8,14 Fig. 6-1 shows this association at the level of the states. Usually there are relatively more dentists in states with higher per capita incomes. This same phenomenon also is likely to apply to smaller geographic units such as counties, cities, and other natural market areas.
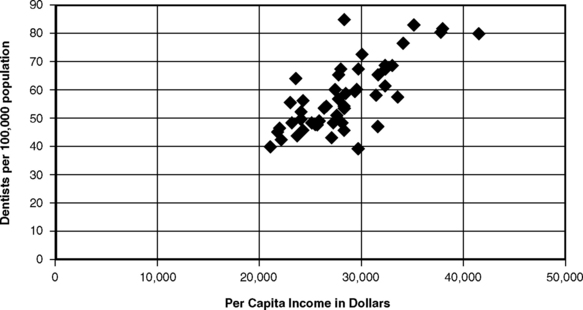
Fig. 6-1 The association between mean per capita income and the dentist/population ratio for individual states in the United States, 2000.65,67
Even within communities that are well stocked with dentists, some groups are not readily treated in private practice (see Chapter 9). Treatment of the preschool child with behavioral difficulties, for example, requires a degree of time, patience, experience, and training that can make such treatment uneconomical for many general practitioners to provide, and pediatric dental specialists are not always available. Many elderly people cannot afford the care that they need, and many have difficulty traveling because of physical infirmities. In addition, there are people who are chronically ill, mentally retarded, or physically challenged, or who have illnesses that require them to receive dental treatment in a hospital. Private practices that are optimally designed for ambulatory, highly compliant patients are often not well suited to care for such persons.
Low-income individuals often have a double problem: care is less available near where they live, and when it can be found it is relatively expensive. It is hardly surprising that people in low socioeconomic areas are often thought “not to value dental care.” That belief is not necessarily true; rather, the circumstances of their lives do not always permit the disadvantaged the luxury of “valuing dental care” the way that dentists would like.30 Given this situation, “free choice” can be most accurately described as a middle-class value that may mean little in other socioeconomic contexts.
Free choice also cuts the other way: dentists have some freedom to reject patients (although not solely on the basis of race, ethnicity, or human immunodeficiency virus status; see Chapters 3 and 10). Some practitioners may believe that they are treating as many patients as they can manage and therefore will accept no new patients of any kind. Others may reject patients whose care is financed by public programs such as Medicaid (see Chapter 7). This rejection may be based on the dentist’s view that such programs offer poor compensation and are bureaucratic nightmares, or the dentist may be unable to accept the attitudes and values of low-income individuals.
From the community viewpoint, the principal advantages and disadvantages of private practice as a delivery system relate to economics. Private funds are used to build the facilities, buy equipment, hire auxiliary staff, and pay for some of the expenses (although by no means all; see Chapter 8) of dental education. Dentists set their own fees. Dentists also have traditionally practiced price discrimination, meaning that they have charged wealthy patients higher fees than they have charged poorer ones. Wealthier patients in these practices therefore subsidized the poorer ones.
The business demands of running a dental practice can conflict with the need to provide for the dental treatment of all people. Dental fees simply are too high for some. The solo dental practitioner has certain overhead costs to meet: utilities, rent, equipment, supplies, staff payroll, and insurance. These expenses must be met regardless of whether or not patients come and whether or not fees are collected. In addition, the dentist is a highly trained and qualified professional and thus is deemed by American culture to be entitled to a good income. Many dentists graduate from dental school heavily in debt because of the high costs of their education and thus have a strong incentive to begin showing profits soon after they begin practice. The average debt among all dental graduates in 2003 was $118,750.17 It is interesting to compare these facts of the dental practitioner’s position with those of the position of the medical surgeon, who does not have to pay for hospital beds and hospital support staff out of the physician’s fee.
Solo Practice
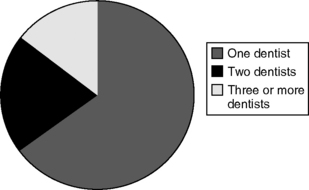
Within the overall realm of private practice, which is the principal form of dental practice in the United States, the solo practitioner is the most common form of practice. The ADA estimated that in 1998 almost two thirds (65%) of private practitioners worked in a practice with no other dentists, about 20.5% worked with one other dentist, and just over 14.5% worked with two or more other dentists.16 This distribution is shown in Fig. 6-2.
Group Practice
A nonsolo dentist works in a practice with at least one other dentist. Some of these dentists may be employed by the owner dentist in the practice.3
As demonstrated in Fig. 6-2, solo practice remains the most common form of dental practice, and nonsolo practices generally are small, most of them consisting of two dentists. Although it is uncommon for newly graduating dentists to directly enter practice as a solo practitioner, the long-term pattern suggests that the dominance of solo and small group practices will continue, with a possible gradual shift toward small group practices.
Franchised Practices and Department Store Clinics
By the early 1980s, there appeared to be the beginning of an explosive growth of franchised dental practices.9,18,71 The idea as applied to dental practice varied in detail among franchises but tended to include such things as a franchise name; marketing and management services; bulk purchasing of supplies; and sometimes the design, construction, and equipping of the practice itself. The dental clinic space was usually leased by a dentist, because many state laws do not allow dental practices to be owned by a nondentist.
After a quick start in the early 1980s, most franchise dental organizations had fallen on difficult times by 1988;73 all but a few were out of business or under bankruptcy protection. Reasons for this turn of events include undercapitalization, overexpansion, poor management control, unprofessional image, and high costs.73 Fundamental conflicts between the traditional strengths of franchises and dental practice make it unlikely that franchised dental practice will ever be a major force. The standardization of process and procedures that leads to cost savings and uniform quality in many businesses is unlikely to produce cost savings in dental care.
HOSPITAL DENTISTRY
Although only a small fraction of dental care is provided in hospitals, dentists still have a substantial role in hospitals. In the mid-1980s, approximately 1000 hospitals in the United States had formally organized departments of dentistry, and about 40,000 dentists were members of the medical staff of at least one hospital.10,33 In 1995, the number of dentists in the United States with hospital privileges was still about 40,000.13
The number of dental general practice residencies in hospitals grew rapidly through the 1970s, and as of 2003 there were 1423 first- year hospital-based residency positions.17 The extended experience in the hospital environment that these residencies provide is likely to make it easier for these dentists to make use of hospital privileges later in their careers. Many dentists affiliated with these and other educational programs in hospitals have full-time or substantial part-time commitments to hospital-based care. Dentists in the military and with the Department of Veterans Affairs are also commonly in hospital-based practices. The majority of dentists who have hospital privileges, however, are in private practice and provide care only occasionally in the hospital.
Dental care provided in hospitals is for those situations in which general anesthesia and other resources of a hospital are required, such as for treatment of very young children with rampant caries, oral surgery to remove carcinomas, cleft palate repair, and maxillofacial prosthetic treatment for victims of burns or trauma. In addition, some routine dental care is provided in hospitals for patients who are suffering from serious systemic disease and for whom the risk of being treated in the private dental office would be unacceptably high. The inclusion of ADA representation on the board of the Joint Commission on Accreditation of Healthcare Organizations since 1980 helps to ensure an appropriate role for dental consultation and services within hospitals.
Beyond the traditional role of educational programs and consultative services, a major challenge for hospital dental departments is economic justification. All departments within hospitals are increasingly being pressed to show that the income they produce is sufficient to justify their existence, and the traditional roles of teaching, consultation, and care for indigent patients do not provide high levels of revenue. On the other hand, moves by hospital-based programs to solicit insured patients through ambulatory care facilities are seen as unfair competition by some private practitioners.35,57
PUBLIC PROGRAMS
Many of the long-established clinical programs of the U.S. Public Health Service were described in Chapter 1. In addition, the Community and Migrant Health program of the U.S. Public Health Service provides grants to support public and nonprofit organizations to plan, develop, and operate health care facilities, known as community and migrant health centers, in rural and urban areas where existing health care resources are inadequate. These centers are primarily medical, but many provide dental services too. As of 2002 there were 1230 full-time-equivalent (FTE) dentists, 383 FTE dental hygienists, and 2291 FTE dental assistants, aides, and technicians employed at these health centers.66 These centers are established in areas where access to private care is limited, and they employ salaried dental personnel.
Another program aimed at making care available in areas unattractive to private practice is the National Health Service Corps. This program, discussed more fully in Chapter 8, has provided incentives, including scholarships and loan repayment, to encourage dentists to practice in remote and underserved areas. Many National Health Service Corps dentists practice in community and migrant health centers.
Auxiliaries in Public Programs
Auxiliary-based programs have long been the backbone of public dental care in some countries, although not in the United States. The oldest and best known is the New Zealand school dental nurse plan, introduced in 1921. New Zealand is a nation of some 4 million people in the South Pacific, 1500 miles off the eastern coast of Australia. Living standards are high, and New Zealand has been a world leader in a number of social programs: old-age pensions, visiting maternal and child health nurses, and the secret ballot at political elections. A number of these programs began in the late nineteenth century, about the time that social security programs were initiated in Bismarck’s Germany. Given these traditions, the introduction of the school dental nurse plan was not as radical an innovation as it might seem, although there was some concern among dentists at the time.61 The stimuli for the program were the extensive dental disease found in army recruits during World War I (1914-18) and government intent to do something about this problem. Dentists were in short supply at the time, and treatment of young children was not as accepted in dental practice as it is now. Caries experience remained high for a long time in New Zealand22,23 before that country joined in the worldwide decline in the late twentieth century (see Chapter 20).
When the service began, care was offered only to younger school-aged children, but eligibility was soon extended to all preschool-aged children and all children in primary and intermediate school. Although most care is provided by dental therapists (the current name for dental nurses), recent legislation will extend practice possibilities for dental therapists, including treating publicly funded clients in private practice and treating indigenous populations.41 The traditional 2-year diploma program has also been supplemented with a 3-year degree program.64
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses