Restorative paediatric dentistry
Erin Mahoney, Nicky Kilpatrick, Sally Hibbert and Timothy Johnston

Primary teeth
Why restore primary teeth?
Our child patients deserve the best dental treatment that clinicians can provide as any treatment, preventive or restorative, will shape their dental future. Doubts have been raised about the rationale behind restoring primary teeth, amid claims that the majority of carious primary teeth exfoliate without causing symptoms. While there is ample strong evidence to contradict this view, the quality of the restorative treatment performed remains paramount. However, it is essential that there is an understanding of the caries risk of the individual patient, the developmental stage of the dentition and the status of the dental pulp prior to determining the choice of restorative material and technique. The objective of any restorative technique is to:
Primary versus permanent teeth
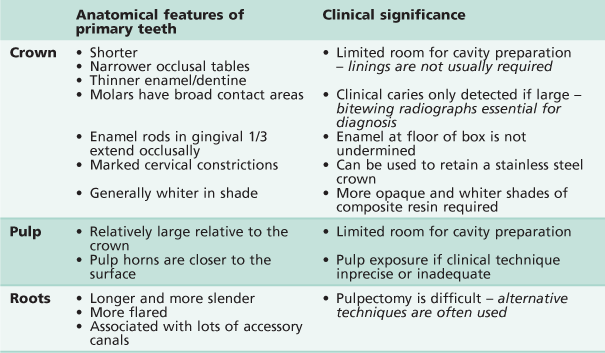
There are significant differences in the anatomy of the primary dentition in comparison with the permanent dentition that create some challenges when it comes to restoration of carious lesions (Table 6.1).
Restorative materials
There are a variety of restorative materials available to restore carious lesions in the primary dentition. Given the large number of techniques and products available on the market it is important for clinicians to understand the procedure they are using and to be aware that all approaches are operator and technique sensitive.
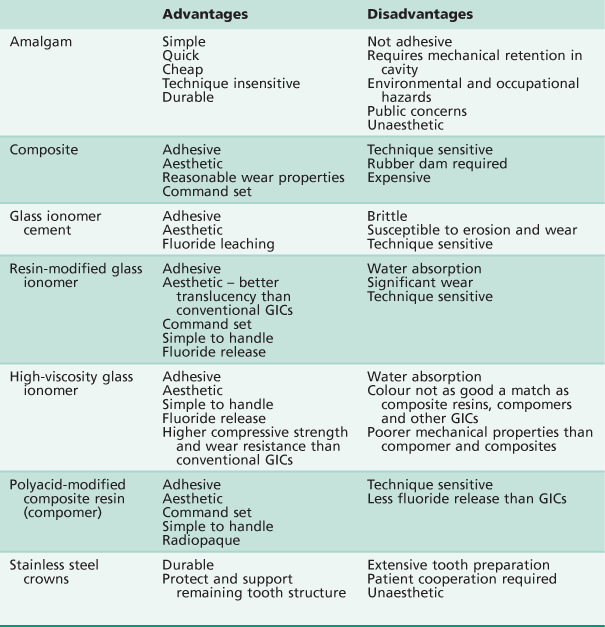
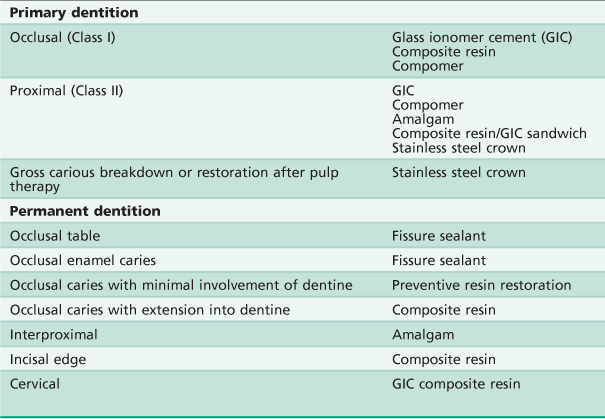
Table 6.2 summarizes the main advantages and disadvantages of the various dental restorative materials.
Amalgam
Historically, due to its simplicity, dental amalgam was the most popular restorative material. However today, as a result of concerns surrounding its potential toxicity and unfavourable aesthetics, amalgam is rarely used in the primary dentition. Indeed, in some parts of the world, it has been banned in children altogether. Today, dental amalgam has been largely superseded by alternative materials and techniques in the restoration of the primary dentition.
Glass ionomer cements (GICs)
A glass ionomer consists of a basic glass and an acidic water-soluble powder that sets by an acid–base reaction between the two components. A principal benefit of GIC is that it will adhere chemically to dental hard tissues. A number of GICs are available on the market today, each having its advantages and disadvantages, however indications for the use of GICs are limited and inappropriate use is likely to lead to failure.
Conventional GICs
Conventional GICs are chemical-set glass ionomers with the weakest mechanical properties. The initial setting reaction is complete within minutes but the material continues to ‘mature’ over the following months. It is important to protect these materials from salivary contamination in the hours following placement or the material may shrink, crack and even debond. Adhesion of all GICs may be enhanced by the use of a dentine conditioning agent before placement. Today, chemically curing GICs are available as both restorative and protective sealant types of materials with high fluoride releasing properties.
High-viscosity GICs
High-viscosity GICs were developed for the atraumatic restorative technique (ART). These chemically cured materials have significantly better mechanical properties than the conventional GICs and are fast setting. Research suggests that these materials have a durability comparable with amalgam, when used in occlusal (Class I) restorations in primary teeth, although the success rate is lower in inter-proximal (Class II) restorations, when other materials should be considered.
Resin-modified glass ionomer cements
Resin-modified glass ionomer cements were developed to overcome the problems of moisture sensitivity and low initial mechanical strength. They consist of a GIC along with a water-based resin system which allows photopolymerization to occur before the acid–base reaction of the glass ionomer is complete. This reaction then occurs within the light polymerized resin framework. The resin increases the fracture strength and wear resistance of the GIC. Resin modified GICs are manufactured as restorative and lining materials for use in both primary and permanent teeth.
Composite resins
Resin-based composites (along with photopolymerization) have revolutionized clinical dentistry. In the primary dentition, composite resins are being increasingly used in combination with GICs in a ‘sandwich’-style aesthetic restoration. Placement of these materials is highly technique-sensitive, as there is no doubt that patient compliance and adequate moisture isolation can prove difficult in the younger, more challenging child. There is little evidence to support this approach and yet, the demand for aesthetic restorations makes this an attractive option.
Compomers (polyacid-modified composite resin)
Polyacid-modified resin composite resins or ‘compomers’ are materials that contain a calcium aluminium fluorosilicate glass filler and polyacid components. They contain either or both essential components of a GIC. However, they are not water-based and therefore no acid–base reaction can occur. As such, they cannot strictly be described as a glass ionomer. They set by resin photopolymerization. The acid–base reaction does occur in the moist intra-oral environment and allows fluoride release from the material. Successful adhesion requires the use of dentine-bonding primers before placement.
Stainless steel crowns
Stainless steel crowns are preformed extra-coronal restorations that are particularly useful in the restoration of large multisurface cavities and grossly broken down teeth. They cover the entire clinical crown and therefore recurrent or further caries is very unlikely. Placement of traditional stainless steel crowns is associated with considerable tooth preparation that can be challenging for patient and clinician alike. However, the introduction of minimal intervention sealed restorations (known as the ‘Hall crown technique’) has made the use of these restorations more realistic. They are, without doubt, the most durable restoration in the primary dentition and should be the technique of choice in the high-caries mouth.
Choice of materials
The choice of material to use in a given situation is not always simple and should not be based merely on technical considerations. Factors other than durability may be equally important in the choice of material, particularly in children.
Age
The age of a child will influence their ability to cooperate with procedures such as rubber dam application and local anaesthesia. The age of the child will also dictate for how long a restoration is required to remain satisfactory. A restoration in a first primary molar in a 9-year-old child does not require the same durability as a restoration in a second primary molar in a 4-year-old child.
Caries risk
Restorations in a child considered to be at high risk of caries may need to fulfil different objectives from restorations in a low-risk child. Although the use of a fluoride-releasing material has obvious preventive advantages, glass ionomer cements (GICs) may not be the most appropriate choice in a mouth that is at high risk of further acid attack. Stainless steel crowns may involve a significant amount of tooth destruction, but this will be appropriate if it eliminates the need to re-treat in the future. Alternatively, GICs have a useful role in initial caries control in cases of rampant caries.
Cooperation of the child
Many young children have behaviour that is not conducive to perfect, textbook, cavity preparation and restoration. In these cases, highly technique-sensitive procedures are inappropriate. A more forgiving restoration that can tolerate some moisture contamination, without detriment to its longevity, may be suitable. The use of GICs in the management of caries in anterior primary teeth may be an excellent method of slowing the carious process and temporarily restoring aesthetics in a 2-year-old child, without recourse to general anaesthesia. By the age of 3 or 4 years, the child may be able to cope with more definitive treatment with composite resin and strip crowns.
Restorative implications of behaviour management
Unfortunately, not all children are able to cooperate with dental treatment under local anaesthesia. This may be because of their age or due to physical or intellectual disabilities necessitating the completion of treatment under sedation or general anaesthesia. When treatment is provided this way, the highest standard of dentistry possible should be provided to reduce future dental treatment for these high-need children. Use of materials and techniques that are known to have longevity, such as stainless steel crowns, are mandatory.
Restoring the primary dentition (Table 6.3)
Posterior teeth
GICs, resin-modified GICs and compomers
These materials have an increasingly important role in the management of carious lesions in primary molars because of their adhesive and fluoride-leaching properties.
Indications
Small occlusal and interproximal cavities. Because of their lack of strength, GICs should not be used in large restorations, particularly in teeth that need to be retained for 3 years or more. The use of polyacid-modified composite resins/compomers show considerable potential, particularly in terms of handling characteristics and radio-opacity. However, they have limited fluoride-leaching ability.
Success
The median survival time for conventional GICs is around 33 months. The failure rate of GICs is 33% over 5 years. High viscosity GICs demonstrate greater durability.
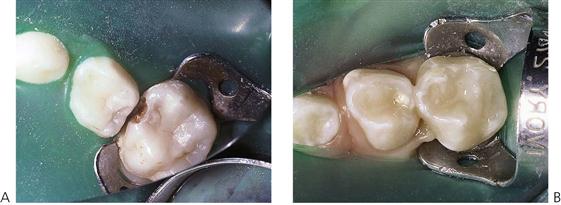
Technique
1. Local anaesthesia and rubber-dam isolation should be used where needed (Figure 6.1).
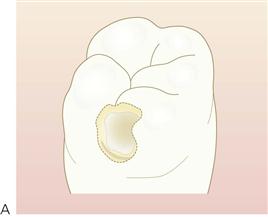
2. The outline of the cavity should follow the extent of the carious lesion. There is no need for extension for prevention. A small occlusal dovetail is not usually necessary for interproximal restorations, however, additional retention form for minimal proximal cavities can be achieved by placing grooves into the dentine using very small (size  ) round burs (Figure 6.2).
) round burs (Figure 6.2).
8. The occlusion should be checked on removal of the rubber dam.
Composite resins
In primary molars, composite is a satisfactory restorative material provided that the child is cooperative and good moisture control is achievable.
Indications
Small to moderately sized occlusal and proximal cavities.
Success
Clinical studies suggest that Class II composite restorations in primary molars are only moderately durable, with one study reporting <40% success after 6 years. However, recent studies have shown greatly improved success rates with the newer resin-based composites.
Technique
For interproximal lesions, the cavity design needs to be modified slightly in that a bevel should be prepared around the occlusal margins for additional adhesion to enamel. The biggest problem encountered with composite restorations is the integrity of the bond at the depth of the proximal box. Placement of composite is technically difficult and highly sensitive to moisture contamination. Placement of a glass ionomer liner over the dentine not only ensures a good bond at the base of the cavity, reducing microleakage, but also provides fluoride release locally. The use of rubber dam and incremental placement of composite in the proximal box may reduce handling and polymerization contraction problems.
Increasingly, parents are requesting tooth-coloured restorations. It should be recognized, however, that use of these materials is associated with increased technical demands and expense.
Stainless steel crowns
Indications
Stainless steel crowns are preformed extra-coronal restorations that are particularly useful in the restoration of:
Success
Stainless steel crowns undoubtedly provide the most durable restoration for the primary dentition with survival times in excess of 40 months.
Relatively expensive in relation to both time and money in the short term. However, the rate of replacement of these restorations is low (3% compared with 15% for class II amalgam restorations). This makes them economic/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses