Oral and Maxillofacial Radiology
General Considerations
Radiation Physics
A Radiation is the emission or movement of energy through space in the form of particles or waves
a. Particles have both mass and energy
b. Some particles may have a positive, negative, or neutral charge
c. Particles cannot reach the speed of light
d. Examples—neutrons, protons, electrons, α-particles, and β-particles
b. Energy charges and currents associated with electric and magnetic waves and frequencies
(1) Wavelength—distance from one crest of a wave to the next; the shorter the wavelength, the greater are the energy and penetrating ability of the radiation; the shortest wavelengths are measured in nanometers (nm) (1 × 10−9 meters [m]), and the longer wavelengths are measured in meters
(2) Frequency—number of wavelength crests passing a particular point per unit of time; measured in hertz (Hz); 1 Hz is equal to 1 cycle per second; the frequency of electromagnetic radiation ranges from <3 × 109 to >3 × 1019 Hz
(3) Photon and quantum—terms used to designate a single unit or bundle of energy
(4) Energy—ability to do work; energy of electromagnetic radiation is measured in electron volts (eV); x-ray energy ranges from 100 to 100,000 eV (1 kiloelectron volt [keV] is equal to 1000 eV)
(1) Bundles of energy that have neither mass nor charge
(2) Travels at a velocity of 186,000 miles per second (the speed of light)
(3) Electromagnetic energies exist over a wide range of magnitudes; the range is termed the electromagnetic spectrum
(4) The electromagnetic spectrum is measured according to frequency, energy, and wavelength
(5) Interaction with biologic tissue causes changes in the tissue as a result of ionization
d. Examples—radio waves, microwaves, infra-red light, visible light, ultraviolet light, x-rays, gamma rays, and cosmic rays
(1) Ion—charged particle; either positive or negative
(2) Ion pair—positive ion and negative ion
(3) Ionization—process by which radiant energy removes an orbital electron from an atom to yield an ion pair
(4) Ionizing radiation—particulate and electromagnetic radiation with sufficient energy to cause ionization of atoms; radiation must have energy greater than electron-binding energy
b. Biologic significance—damage of biologic systems results from the ionization process
c. Examples—α-particles, β-particles, x-rays, and gamma rays
1. Naturally occurring (or background) radiation constitutes 50% of the overall exposure to the United States population1
a. Radon gas, the result of naturally occurring radionuclides found in soil (a radionuclide is an unstable atom that decays by emitting particles and energy from the nucleus to become electrically stable) accounts for 37% of the natural background radiation (Figure 6-1)
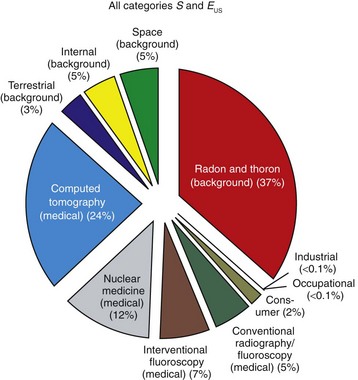
FIGURE 6-1 Annual effective dose equivalent of ionizing radiations. This chart illustrates the approximate percentage of exposure of the U.S. population to background and artificial radiations. (Reprinted with permission of the National Council on Radiation Protection and Measurements, http://NCRPonline.org)
b. Other terrestrial sources, cosmic radiation from outer space, and internal sources make up another 13% of natural exposure
2. Medical applications make up 48% the overall exposure to the United States population1
a. Computed tomography (CT) and nuclear medicine lead medical exposures by 24% and 12%, respectively
b. Other conventional radiographs, including oral and maxillofacial radiography, constitute 5% of medical exposures
3. Consumer products and industrial and occupational exposures account for the remaining 2% of total exposure to the United States population
D Exposure—defined as the average annual effective dose equivalent of ionizing radiation
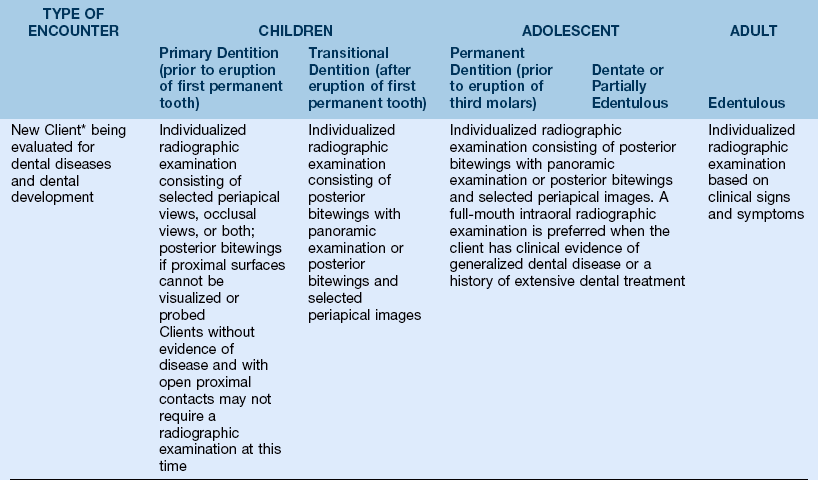
1. Average annual effective dose equivalent of ionizing radiation to a member of the U.S. population is 6.2 millisieverts (mSv) up from 3.6 (mSv) in the early 1980s1 (Figure 6-2)
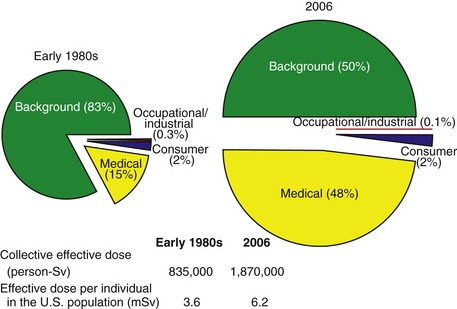
FIGURE 6-2 Comparison of effective dose equivalents. These charts illustrate the difference in approximate percentage of exposure of the U.S. population to background and artificial radiations in the early 1980s and 2006. (Reprinted with permission of the National Council on Radiation Protection and Measurements, http://NCRPonline.org)
2. Significant increase largely arising from the increased use of large-dose medical imaging technologies1
Electricity
A Definition—flow of electrons through a wire or other electrical conductor
1. Direct current (DC)—electrons flow in one direction only along an electrical conductor
2. Alternating current (AC)—electrons flow in one direction and then reverse to flow in the opposite direction
1. Ampere (A)—the number of electrons flowing in an electrical circuit; one milliampere (mA) is equal to  ampere; modern dental machines commonly operate between 5 mA and 15 mA
ampere; modern dental machines commonly operate between 5 mA and 15 mA
2. Volt (V)—electrical potential or force that moves electrons along an electrical conductor; one kilovolt (kV) is equal to 1000 volts; kilovolt peak (kVp) refers to the peak voltage of an alternating current; dental units usually operate between 60 kVp and 100 kVp
D Power supply to dental x-ray machines is primarily 110 -V, 60-Hz alternating current
X-Ray Machines
1. Intraoral units—designed to provide sufficient radiation output for standard intraoral bitewing, periapical, and occlusal radiographs
a. the x-ray beam is restricted to provide exposure of small anatomic sites
b. Kilovolt peak (kVp) and milliampere (mA) settings may be constant or variable, depending on the manufacturer
2. Extraoral units—designed to provide greater radiation output as required by extraoral procedures; the x-ray beam is larger to accommodate larger anatomic areas under study
1. Generator—device that supplies electrical power to the x-ray tube
a. Transformer—device that changes the potential difference of incoming electrical energy to any desired level
(1) Step-up transformer—increases the voltage sufficiently to propel electrons across the vacuum tube circuit to produce x-ray energy
(2) Step-down transformer—decreases the voltage to generate the electrons needed at the filament circuit
(3) Autotransformer—a special type of self-rectifying transformer designed to supply voltage of varying magnitude to several different circuits of the x-ray machine (e.g., filament circuit and high-voltage tube circuit)
(1) Definition—process of changing an alternating current into a direct current
(2) Rectifier—an electrical device that changes AC to DC
(3) Dental x-ray units are considered to be self-rectified or half-wave rectified
(a) In half-wave rectification, x-rays are generated during the first (positive) half of the electrical cycle; the filament is negative and the target is positive
(b) X-rays are not generated during the second (negative) half of the electrical cycle
(c) With a 60-cycle alternating current, 60 pulses of x-rays are generated per second, with each having a duration of  second
second
(4) In full-wave rectification, x-rays are generated during both phases of the alternating current cycle
(1) Lead-lined metal casing for the x-ray tube designed to prevent excessive radiation exposure and electrical shock
(2) Limits amount of radiation leakage from unit
(3) Provides mechanical support and protection for the x-ray tube
(1) Oil, gas, or air is sealed within protective housing and surrounds the x-ray tube
(2) The system serves as both a thermal cushion and a lead-lined electrical insulator
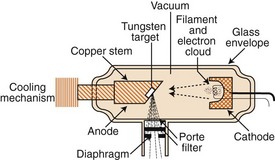
(1) Surrounds the electrodes of the x-ray tube to provide a vacuum
(2) The aperture, or window, is a thin segment of the glass that allows maximum emission of x-rays and minimum absorption by the glass
(1) Electrically negative portion of the x-ray tube
(3) Milliamperage control regulates the:
(c) Quantity of electrons are “boiled off” during thermionic emission (when electrical current is passed through a coil of tungsten wire, atoms of the wire absorb thermal energy, and some outer-shell electrons acquire enough energy to move a small distance away, forming an electron cloud)
(4) Because like charges repel, the electron beam is directed to a small area on the anode
(1) Electrically positive portion of an x-ray tube
(a) Tungsten target (tungsten is used as the target material because of its high atomic number, which yields higher efficiency in x-ray production plus higher-energy x-ray photons; conducts heat well; has high melting point [3380°C])
(b) Copper stem—functions to conduct heat away from the target
(1) Process of selectively removing x-rays from the beam
(2) Total filtration—the result of inherent and added filtration
(a) Inherent filtration—filtering of a beam by a glass tube
(b) Added filtration occurs by placing metal discs (usually aluminum) in the path of an x-ray beam
(3) Low-energy, nonpenetrating x-rays are filtered from the beam
(4) Federal regulations require 1.5 millimeters (mm) of aluminum-equivalent filtration for units operating below 70 kVp and 2.5 mm of aluminum-equivalent filtration for units capable of operating above 70 kVp
3. Position-indicating device (PID)
a. Definition—an open ended, circular or rectangular “cone” that extends from the tube head to direct the x-ray beam toward the image receptor
b. Federal regulations limit the size of the intraoral x-ray beam to 7 cm (2.75 inches) in diameter
c. Rectangular PIDs have an exit size of 3.5 × 4.4 cm (1.375 × 1.75 inches)
d. Available lengths of PIDs are 20 cm (8 inches), 30 cm (12 inches), and 40 cm (16 inches)
e. The longer PID produces an x-ray beam that is less divergent
a. Description—exposure factors (mA, kVp, and exposure time) are set, and electrical circuits are activated by using the controls located there
(1) Most intraoral machines available today have preset mA and kVp
(2) Usually, settings of 5, 7, 10, or 15 mA are available; kVp settings range from 60 to 100
(3) Depending on the machine type, the automatic timer is adjusted in impulses ( of a second) or in fractions of a second
of a second) or in fractions of a second
(4) The exposure switch is depressed to initiate the emission of x-radiation
(5) The emission of x-radiation from the machine is indicated by an audible “chirping” sound and the glow of an exposure indicator light
(6) The control panel must be located in a protected area and still allow for observation of the client during exposure
Production of X-Radiation
1. Initial process for x-radiation production is achieved by the activation of the on–off switch located on the unit control panel; this process completes the filament circuit, and the filament is heated
2. Appropriate mA, kV, and exposure time are set by using the controls located on the unit console; if mA and kV are preset by the manufacturer, the control panel will be labeled with the preset values
a. Milliamperage control, which is connected to the mA-filament circuit (step-down transformer), allows for warming of the cathode filament and determines the number of electrons available for x-ray production; the higher the mA, the hotter the filament becomes, resulting in a greater number of available electrons
b. Kilovoltage control, which is connected to the high-voltage circuit (step-up transformer), establishes the high voltage needed for x-ray production; this control also provides the condition in which the anode is positively charged and the cathode is negatively charged for the attraction and high-speed acceleration of electrons from the cathode to the anode; the higher the kVp setting, the greater is the speed of acceleration of electrons from the cathode to the anode
c. The exposure time establishes the time during which electrons are available for the bombardment of target material
B Electronics of x-ray production
1. X-rays are produced by the interactions that occur when high-speed electrons strike a target material
2. The phenomenon of x-ray production occurs only when the exposure switch on the console is pressed, which completes the high-voltage circuit
a. The heated filament provides electrons for x-ray production by thermionic emission
b. Thermionic emission occurs when electrons absorb sufficient thermal energy (from the mA circuit) to allow for the electrons’ short movement away from the filament; commonly referred to as a “boiling off” of electrons; an electron cloud surrounding the filament is formed
c. The closure of the high-voltage circuit creates an electrical potential difference whereby electrons are attracted from the negative cathode to the positive anode
d. The one-directional flow of electrons (from the negative cathode to the positive anode) is influenced by the focusing cup of the cathode; electrons are repelled away from the negatively charged focusing cup because like charges repel; this mechanism controls the size and shape of the electron stream
C Electron–target interactions
1. The electron stream is directed at a small portion of the target called the focal spot
2. The actual production of x-radiation occurs by the interaction of accelerating electrons and target atoms
3. Less than 1% of the kinetic energy leaving the cathode is converted into x-ray energy; just over 99% of the kinetic energy leaving the cathode is converted into heat energy
4. Two types of interactions for x-ray production
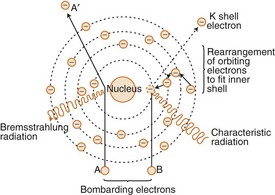
a. General (braking, or bremsstrahlung) radiation (Figure 6-4)
(1) 70% of x-ray photons produced by dental x-ray units in this manner2
(2) The accelerating electron passes near the nucleus of the target atom and is slowed down by the attraction of the nucleus
(3) The slowing-down process results in the transference of the electron’s kinetic energy into x-ray energy plus a change in the traveling direction of the electron
(4) The energy of the photon produced depends on the amount of kinetic energy transferred
(5) The closer the accelerating electron passes by the nucleus, the greater is the nuclear attraction, which thereby yields greater energy transference and higher photon energy
b. Characteristic radiation (see Figure 6-4)
(1) Can only occur at 70 kVp or higher with a tungsten target;2 accounts for a small portion of x-rays produced by dental x-ray machines
(2) Occurs when an electron removes an orbital electron from the target atom
(3) During restabilization of the ionized atom, the hole created by the ejected orbital electron is filled by an outer-shell electron; the movement of the outer-shell electron results in the transference of electron-binding energy into x-ray energy
(4) The energy of the resulting characteristic x-ray photon occurs from the difference in binding energies of the orbital electrons involved
Interactions of X-Rays with Matter
1. When x-ray photons interact with matter, they may be either absorbed or scattered
a. If an incident (initial) photon is absorbed, it ceases to exist
b. If an incident photon is scattered, its direction of travel is altered; scattered photons do not aid in the formation of the radiographic image and only increase image density; scattered radiation causes fog (or “noise”) that degrades image quality
2. Attenuation (removal) of x-ray photons from the beam as they travel through matter (tissue) is determined by the intensity (energy) of the radiation and the density, atomic number, and electrons per gram of the matter
a. Refers to the passing of x-ray photons through a material without any alteration of the photon or the material; accounts for approximately 9% of interactions
a. Results from an incident photon colliding with a tightly bound inner-shell electron
b. The incident photon ceases to exist; the electron is ejected as a recoil electron (or photoelectron)
c. Ionization of the atom occurs; the ejected electron leaves a vacancy in the shell that must be filled
d. Low-energy characteristic radiation is produced by the shifting of an outer-shell electron to the inner vacancy
e. In the energy range used for diagnostic applications, the photoelectric effect accounts for approximately 30% of interactions
a. Results from an incident photon colliding with a loosely bound outer-shell electron
b. Incident photon gives up part of its energy in the ejection of the orbiting electron
c. Ionization of the atom occurs
d. The direction of travel of the incident photon is changed; its energy is reduced
e. The scattered photon and the ejected electron may have sufficient energy to undergo many more ionizing interactions before losing their entire energy
f. Compton-scattered x-radiations may exit the patient’s tissues and cause image fogging
g. In the diagnostic energy range, Compton scattering accounts for approximately 60% of interactions
a. The interaction of an incident photon passing near an outer-shell electron and being scattered without losing energy
b. The incident photon ceases to exist, and a new photon of identical energy is released from the electron
c. In the diagnostic energy range, coherent scattering accounts for approximately 8% of total interactions
C Image formation and differential attenuation
1. Radiographic image formation depends on the differential attenuation of x-ray photons from the primary beam by the client’s tissues
2. If all photons exited the client’s tissues (no absorption), the image receptor would be totally exposed; if all photons were attenuated (absorbed), the image receptor would be unexposed
3. As a result of photoelectric, Compton, and coherent interactions, x-ray photons are removed from the beam
4. Variances in the ability of tissues to absorb x-rays produce radiographic contrast
5. Generally, as density, atomic number, and electrons per gram of tissue increase, the number of absorbed photons increases; metallic dental restorative materials, enamel, dentin, cementum, and bone absorb photons to a great extent and produce radiopaque images; bone marrow spaces, sinuses, pulp chambers, and periodontal ligament spaces do not attenuate photons and produce radiolucent images
Interactions of Ionizing Radiation with Cells, Tissues, and Organs
1. Whole-body exposure (total body)—each gram of tissue in the entire body absorbs equal amounts of radiation
2. Specific-area exposure (localized)—each gram of body tissue irradiated in the specific area absorbs equal amounts of radiation (e.g., skin exposure from four bitewing radiographs)
3. Direct effect—transfer of energy by ionization mechanism from an x-ray photon to a biologically critical molecule such as deoxyribonucleic acid (DNA)
4. Indirect effect—transfer of energy by the ionization mechanism from an x-ray photon to a noncritical molecule, which, in turn, delivers the energy to the biologically critical molecule
5. Genetic effect—causes mutations in future generations; results from the exposure of reproductive cells, yielding alterations in genetic coding
6. Somatic effect—injury in the person being irradiated
7. Latent period—time between the exposure and development of the biologic effect
8. Deterministic effect— when the severity of a biological response is dependent on the dose; for example: erythema (redness of the tissue) would be expected to increase in direct proportion to exposure to damaging radiation
9. Stochastic effect—a biologic response that is based on the probability of occurrence rather than its severity; for example: cancer may or may not occur with exposure to damaging radiation
10. Acute effects (short-term or early)—effects that may occur minutes, hours, or weeks after exposure; usually result from high doses of whole-body exposure
11. Chronic effects (long-term or late)—effects observed years after original exposure
B Units of radiation measurement—two systems used to define radiation measurement: the metric equivalent system, or Systeme Internationale (SI), adopted in 1985, is preferred;3 an older, traditional system may be found in the research literature published prior to 1985
1. Radiation exposure—measurement of ionization in air produced by x-rays
a. SI units of exposure—defined as electrical charge per unit mass of air or coulomb (C) per kilogram (kg)
b. The traditional unit of exposure is a roentgen—1 roentgen is the amount of x-radiation or gamma radiation that will produce 2.08 × 109 ion pairs in 1 cubic centimeter (cm3) of air
2. Radiation absorbed dose—amount of radiation absorbed by tissue
3. Dose equivalent—measure of biologic effects produced by different types of radiation
C Characteristics of dose–response relationships
1. Linear—the response is directly proportional to the dose
2. Nonthreshold—any dose, regardless of its size, is expected to produce a response
3. Threshold—from zero to a particular point, no response would be expected; above the threshold point, any dose will produce a response
D Biologic responses to irradiation
a. Radiation exposure is harmful to all living tissues and should be used cautiously
b. Injury to cells, tissues, and organs occurs at the time of exposure but may take hours, days, or generations to manifest
c. Radiation injury is caused by ionization
(1) The excitation of orbital electrons in an atom and the deposition of energy in the tissues
(2) Occurs when atoms of a molecule are separated into charged atomic particles (e.g., table salt [NaCl] yields Na+ Cl− when mixed in water [H2O])
(3) May cause a breakage in the molecule or a relocation of the atom in the molecule
(4) Altered molecules may function improperly or cease to function altogether
a. Two types of cells in the human body:
b. Nucleus of proliferating somatic and genetic cells—area of the cell most sensitive to ionizing effects
(1) Exposure to the nucleus results in cell inhibition
(2) Most sensitive sites within the cell’s nucleus—DNA and chromosomes
(3) Chromosomal aberrations in somatic cells are observed during the metaphase stage of mitosis (cell division); changes in genetic material can occur during meiosis or reduction division
(a) Chromosomes—control cell growth, development, and maintenance
(b) Sufficient radiation damage to the DNA may yield visible or invisible chromosomal aberrations that may lead to cell death or malfunction
(c) Tissue or organ destruction—occurs when several cells are damaged and not sufficiently repaired by the body’s repair mechanism
(d) DNA damage can result in an uncontrolled, rapid proliferation of cells, the principal characteristic of radiation-induced malignant disease
(e) Genetic cell or germ cell injury—observed only in future generations (including increased susceptibility to disease, birth defects, and cancer)
c. Cells most sensitive to radiation exposure—young, rapidly dividing, nondifferentiated cells such as those of the developing fetus
d. Cell responses to irradiation
(1) Cell death—the immediate or delayed death of a cell following exposure to a lethal dose
(2) Swelling of the cell results from interference of fluid exchange through the cell wall
(3) Alterations in specific cell function, such as the production of a protein or enzyme of changed chemical composition, can also occur following excessive exposure
(4) Cellular aberration results from damage occurring during mitosis or meiosis
a. Yields radicals that combine to form hydrogen peroxide
b. Hydrogen peroxide is toxic to living tissues; its formation is an indirect, damaging effect of ionizing radiation
4. Factors that determine tissue sensitivity
a. The more mature the cell, the more resistant it is to radiation
b. The younger the tissues and organs, the greater is their radiosensitivity
c. The higher the metabolic activity of the cell, the higher is its radiosensitivity
d. The higher the proliferation rate for cells and the growth rate for tissues, the higher is their radiosensitivity
e. The more differentiated (or specialized in function) the cell, the more resistant it is to the biologic effects of radiation
5. Degree of tissue and organ sensitivity4
c. Organ tissues considered critical for dental radiography are skin, thyroid gland, lens of the eyes, and hemopoietic tissue
d. Continued low-dose exposure negatively affects the repair mechanism; overloading of the repair system by time or amount of exposure can result in somatic or genetic damage
6. Repair and accumulation of radiation effects
a. Most injury resulting from low-dose radiation exposure is repaired within cells, tissues, and organs (depending on the relative biologic damaging ability of the radiation)
b. Repeated exposure may lead to some unrepaired effects that accumulate in exposed tissues
c. Accumulated radiation effects accelerate and increase the probability of inducing cancer and the normal aging process; high doses result in a more rapid expression of the effects
Ethical Considerations Regarding the Use of Ionizing Radiation
A Regulatory and recommending agencies (see the unnumbered table “Web Site Information and Resources” at the end of this chapter)
1. International Commission on Radiological Protection (ICRP)
2. National Council on Radiation Protection and Measurements (NCRP)
3. Federal and State Bureaus of Radiological Health
4. American Dental Association (ADA)
5. American Academy of Oral and Maxillofacial Radiology (AAOMR)
B Assessment of need for radiographic procedures
1. A licensed physician or dentist must prescribe radiographic services
2. Dental hygiene assessment for recommendation of need for radiographs
a. Must be based on a review of the client’s health and dental histories; clinical examinations; client signs, symptoms, and complaints
b. Radiographs are recommended only in the presence of reasonable expectation of client benefit2
c. Recommendations based on U.S. Food and Drug Administration (FDA) selection criteria guidelines (Table 6-1)
TABLE 6-1
Guidelines for Prescribing Dental Radiographs
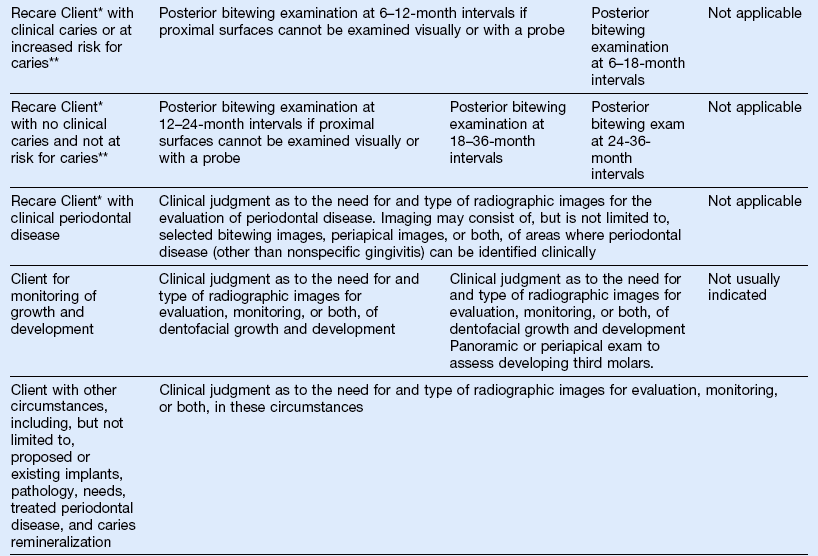
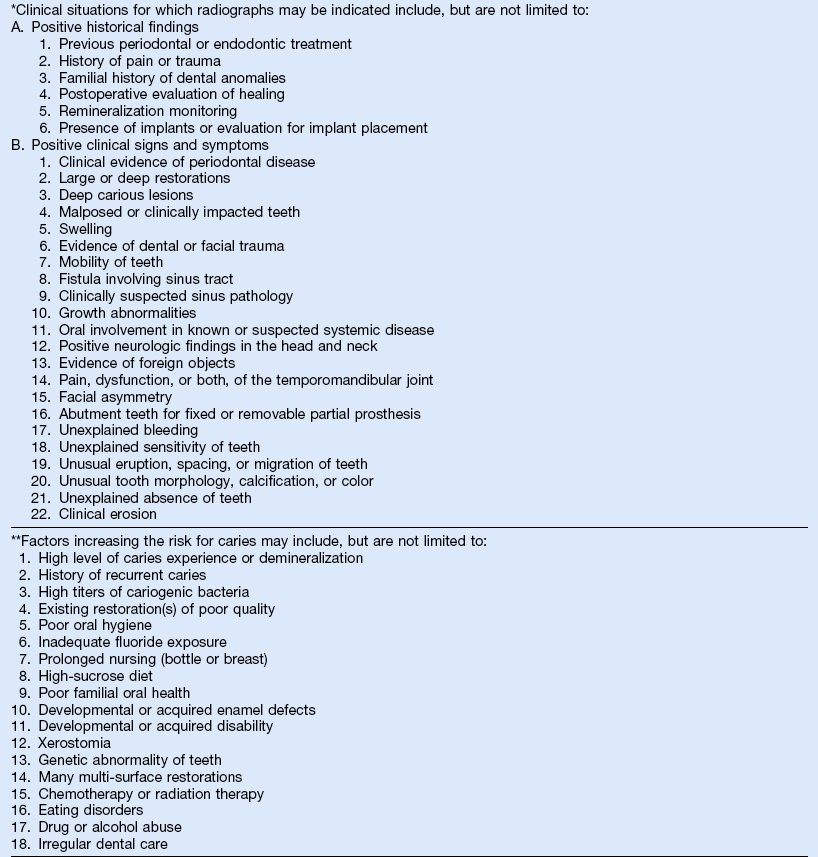
(Data from U.S. Department of Health and Human Services: The selection of patients for dental radiographic examinations, Revised 2004 by the American Dental Association: Council on Dental Benefit Program, Council on Dental Practice, Council on Scientific Affairs.)
d. If no positive findings are noted in the clinical examination or the client’s history, radiography should not be performed
1. ALARA (“As Low As Reasonably Achievable”) concept—individuals working with radiation should attempt to keep all radiation exposure as low as reasonably achievable
2. Maximum permissible dose (MPD) (Table 6-2)
TABLE 6-2
U.S. Nuclear Regulatory Commission Occupational Dose Limits
| Tissue | Annual Dose Limit |
| Whole body | 0.05 Sv |
| Any organ | 0.5 Sv |
| Skin | 0.5 Sv |
| Extremity | 0.5 Sv |
| Lens of eye | 0.15 Sv |
(United States Nuclear Regulatory Commission: Standards for protection against radiation, Title 10, Part 20, of the Code of Federal Regulations. December 4, 2007: Available at http://www.nrc.gov/reading-rm/doc-collections/cfr/part020/part020-1201.html: Accessed Apr.11, 2010.)
a. “The maximum dose of radiation that in light of present knowledge would not be expected to produce significant radiation effects”2
b. Possible occupational exposures received by oral health care personnel is small compared with other medical settings (Figure 6-5)
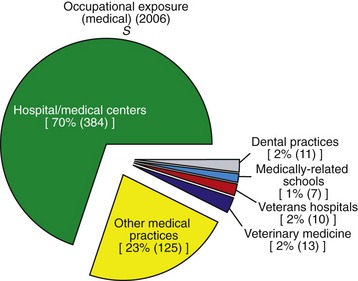
FIGURE 6-5 Occupational exposures by medical profession. This chart illustrates the approximate percentage of occupational exposures to medical radiations. (Reprinted with permission of the National Council on Radiation Protection and Measurements, http://NCRPonline.org)
c. Annual MPD for occupationally exposed workers is 50 mSv (or 5000 millirems [mrem])5
d. Nonoccupational exposure (whole-body) is 10% of that for the radiation worker (5 mSv or 500 mrem per year)5
3. Reduction of unnecessary client dose
a. Eliminate unnecessary examinations
b. Eliminate repeat examinations
(1) Receive training and update skills to avoid retakes
(2) Prepare the client correctly to gain adequate cooperation to perform the procedure
c. Use proper exposure settings
(1) Display exposure-setting guidelines and safety protocol near the control panel
(2) Obtain a working knowledge of the exposure settings for kilovoltage, milliamperage, and exposure time to accurately adjust for proper image density and contrast
(a) Removal of less penetrating x-rays from the beam
(b) Inherent filtration—built into the x-ray unit, includes glass tube, insulating oil, and tube head
(c) Added filtration—aluminum discs placed in the path of the x-ray beam at base of the position-indicating device (PID)
e. Use the fastest image receptor system available
(1) Currently the “F” speed intraoral film requires the least amount of radiation to produce a diagnostic image
(2) Intraoral digital imaging systems that replace film with a solid state sensor or phosphor plate further reduce client radiation exposure
(3) Rare-earth intensifying screens with corresponding green-light–sensitive extraoral film require less radiation than calcium tungstate intensifying screens with blue-light sensitive extraoral film
f. Position client and image receptor properly
(1) The client’s head should be stabilized; place the client’s head against the headrest
(2) Image receptor holders should be used to stabilize intraoral receptors; never use the client’s finger
g. Shield specific areas from possible secondary radiation with 0.25-mm–thick lead or lead equivalent apron
4. Reduction of occupational exposure
a. Use protective shielding and apparel
(1) The operator should remain behind a barrier during client exposure
(2) Any part of the operator’s body that will be in the path of the primary beam must be covered with 0.25 mm of lead or lead-equivalent protection
b. Distance from the source of radiation, if structural shielding is not available
(1) The operator should stand as far away as possible from source of radiation during exposure (a distance of 6 feet is considered the minimum safe distance)
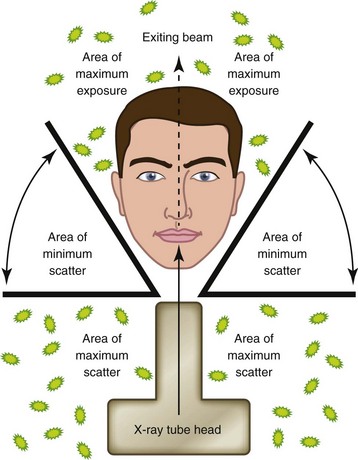
(2) The operator should be in a position of 90 to 135 degrees out of path of the primary beam4 (Figure 6-6)
c. Never hold the client, the image receptor, or the tube head during exposure
D Personnel radiation-monitoring devices4
a. Specialized film packet sandwiched between metal filters contained inside a plastic holder or badge
b. Advantage—inexpensive, reliable technology
c. Limitation—cannot be worn for periods longer than 1 month
E Documentation of client’s radiographic exposure
1. The client’s record should include appropriate space for listing radiographic services
2. All radiographic exposures, both diagnostic and undiagnostic, should be entered sequentially and cumulatively
F Documentation of client’s refusal of radiographic services
1. The client must be informed of possible diagnostic information and possible risks from radiographic procedure
2. The client should be informed of all protection procedures used (e.g., equipment standards, quality assurance, standard darkroom procedures, protective shielding, and operator competence)
3. Having the client sign a refusal-of-radiographic-services form does not release the oral health care provider from responsibility
Infection Control
See the section on “Prevention of Disease Transmission During Radiographic Procedures” in Chapter 10.
1. Infection control procedures established for the oral health care setting must include guidelines for dental radiographic procedures
2. The client’s health history must be reviewed and an oral examination performed before radiographic services
a. Clean and disinfect the radiographic equipment (e.g., tube head and PID, tube-head support arm, control panel, countertop, treatment chair)
b. Use the barrier technique and disposable plastic wrap to cover items likely to become contaminated (e.g., tube head and PID, tube-head support arm, control panel, countertop, treatment chair)
c. Obtain radiographic supplies (e.g., image receptors, holding devices) before starting the procedure
d. Disposable intraoral film packet barrier wraps may be used to minimize the possibility of disease transmission during the radiographic procedure and processing
c. Digital sensors should be wiped with an Environmental Protection Agency (EPA)–accepted disinfectant before placing the protective sheath barrier and following removal; consult the manufacturers’ recommendations
2. While exposing intraoral radiographs, wear disposable client-care gloves
a. Wipe the film packet with an EPA-accepted disinfectant after removal of the film from the client’s mouth and drop the film into a containment cup6 (Figure 6-7)
b. If using a disposable intraoral film packet barrier wrap, after wiping the packet barrier wrap with an EPA-accepted disinfectant, aseptically tear open the wrap, allowing the protected film to drop aseptically into a containment cup; this same procedure is used for phosphor plates; allow the protected phosphor plates to drop into the light-tight containment box; consult the manufacturer’s recommendations.
3. Process intraoral radiographs under safelight conditions
a. Use disposable client-care gloves, and grasp the tab on the back the outer protective wrap and pull it open without touching the film inside
b. Grasp the black paper tab, and pull it straight out, allowing the film to drop out onto a barrier such as a paper towel placed on the counter
c. When all film packets are opened, remove and properly dispose of the client-care gloves
e. With clean, dry hands, grasp the films by their edges and place them into the automatic film processor or onto manual film-processing racks
f. Put on nitrile or neoprene utility gloves to remove the lead foils for proper disposal; properly dispose of other film packaging wastes and paper towels
Image Receptors
1. Mechanism for transferring information contained in an attenuated remnant x-ray beam into a visible image
2. For dental radiography, the image receptor has traditionally been film
3. Digital radiography requires the use of a sensor, or phosphor plate
1. Classified as direct-imaging and indirect-imaging systems
a. Direct imaging—exposure of the film by the interaction of the x-ray beam and the photographic emulsion; exposure of a solid-state digital sensor by the interaction of the x-ray beam and a computer chip composed of a grid of x-ray sensitive cells7
b. Indirect imaging—exposure of the film primarily by the light emitted from an intensifying screen and, to a lesser extent, by the x-ray beam; exposure of a polyester plate coated with phosphors that “store” the energy until stimulated by a laser to release light that is converted into an electronic signal7
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 second
second