Oral Pathology
Benign Lesions of Soft Tissue Origin
General Characteristics
B Age and gender vary with the type of lesion
D Histologic characteristics depend on the lesion (e.g., a lipoma is composed of fat cells)
E Lesion grows slowly, or it may be encapsulated, which contributes to an evaluation of a benign state
Irritative Fibroma (or Traumatic Fibroma) (see Figure 8-1)
A Etiology—chronic mild irritant; chronic trauma
B Age and gender related—40 to 60 years; more common in females (2 : 1)
C Location—most common on the buccal mucosa along the area of the occlusal plane and gingiva; also found on the tongue, lips, and palate
Papilloma
A Etiology—benign lesion of squamous epithelium; long duration; slow development
B Age and gender related—may arise at any age, but there is a 50% incidence between ages 20 and 50 years; no gender predilection
C Location—soft palate or tongue
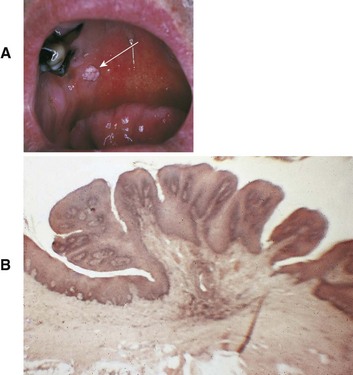
D Clinical features (Figure 8-2, A)
1. Cauliflower-like appearance
2. Usually grayish or white color; can also be pink; color depends on amount of keratin
3. Well-delineated, exophytic nodule with a pedunculated or sessile base
Verruca Vulgaris (Wart)
A Etiology—benign viral induced lesion of stratified squamous epithelium; caused by human papilloma virus (HPV)
B Age and gender related—more common in children; but lesions have also been identified in adults; no gender predilection
C Location—common skin lesion; lips are the most common intraoral site; can also be found on the tongue or mucosa
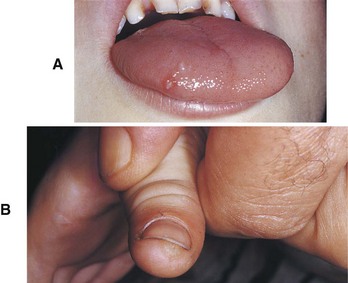
D Clinical features (Figure 8-3, A and B)
1. White, papillary exophytic lesion
2. Can spread to other areas of a person’s skin
3. Self-inoculated (finger-to-mouth)
5. Differs from a papilloma in that warts grow faster, are smaller, and develop in a shorter time
Hemangioma
A Etiology—congenital or developmental origin; when found in adults, these lesions develop as a response to trauma during the healing stages; a benign proliferation of blood capillaries
B Age and gender related—lesions present at birth or develop shortly thereafter; more common in females (3 : 1); occur in adults as a response to trauma
C Location—most common on the tongue; also found on the buccal mucosa, labial mucosa, and the vermilion of lips
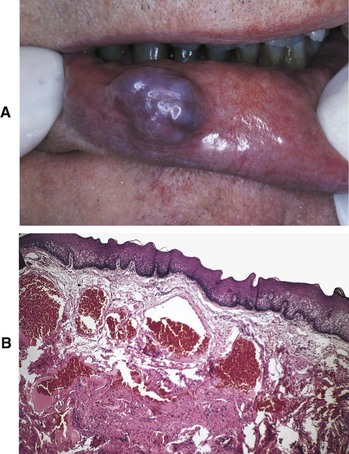
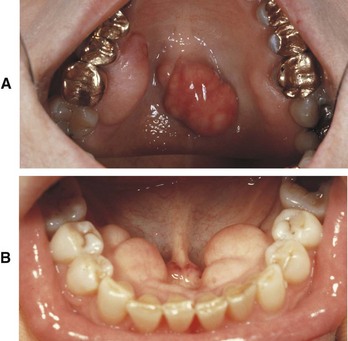
D Clinical features (Figure 8-4, A)
1. Flat or raised, well-circumscribed lesion on the mucosa or tongue
2. Deep red or bluish-purple color
E Histologic characteristics (see Figure 8-4, B)
1. Capillary—many small capillaries lined by a single layer of endothelial cells supported by a connective tissue stroma of varying density; endothelial cell proliferation
2. Cavernous—large, dilated blood sinuses with thin walls, each having an endothelial lining; sinusoidal spaces filled with blood and lymphatic vessels
Lipoma
A Etiology—unknown; rare; benign tumor of mature fat cells
B Age and gender—over 40 years; no gender predilection
C Location—most common on the buccal mucosa or in the mucobuccal fold
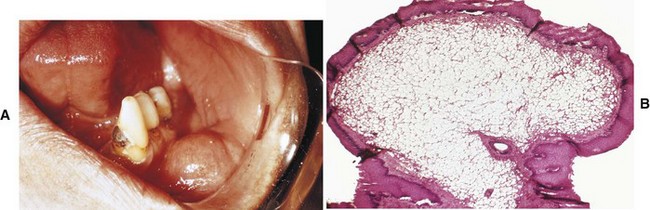
D Clinical features (Figure 8-5, A)
1. Single or lobulated, well-defined, painless mass <3 cm in size
2. Sessile or pedunculated base
4. Yellowish color (if aspirated, a brown-yellow fluid is withdrawn)
Inflammatory Tumors (Granulomas)
Pyogenic Granuloma
A Etiology—an exuberant tissue response to chronic irritants or trauma (i.e., plaque biofilm, calculus, poor restorative margins, hormonal levels)
B Age and gender related—children and young adults; more common in females (3 : 1), perhaps related to an increase in estrogen levels
C Location—much more common on the maxillary labial gingiva than mandibular gingiva; can occur on the lips, tongue, and buccal mucosa
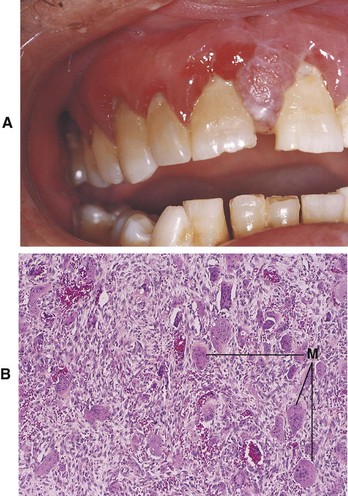
D Clinical features (Figure 8-6)
1. Protrusive mass; pedunculated, sessile, or lobulated base
2. Deep red rather than pink surface
3. Soft and spongy; freely movable; ulcerated, bleeds easily
4. Lesions are a few millimeters to several centimeters
5. In pregnancy, these lesions were formerly called pregnancy tumors
Papillary Hyperplasia of the Palate (Palatal Papillomatosis)
A Etiology—type of denture stomatitis; chronic irritation to the vault of the hard palate related to an ill-fitting denture (full or partial); excessive pressure of an ill-fitting denture; poor denture hygiene (secondary); can also be associated with an orthodontic appliance; wearing the prosthetic device 24 hours a day
B Age and gender related—no gender predilection
C Location—especially—in vault of the hard palate in maxillary denture wearers (suction chamber area)
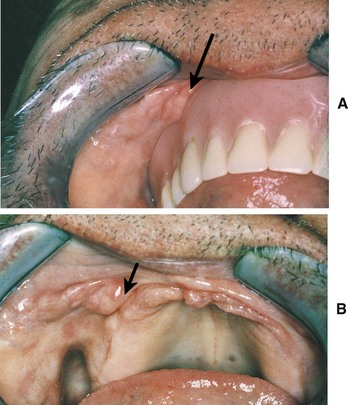
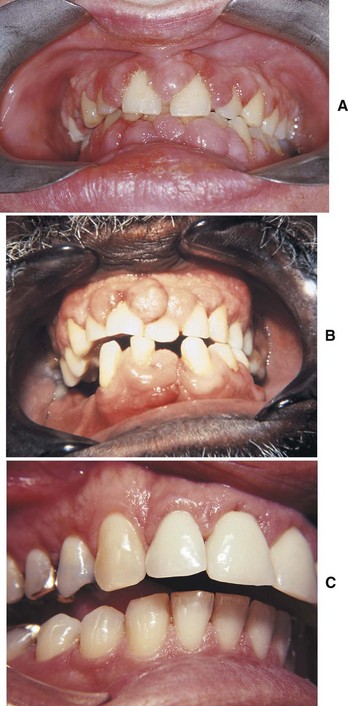
D Clinical features (Figure 8-7)
1. Closely clustered erythematous papillary projections, 1 to 4 mm in diameter
2. Round, smooth, glistening red surface; granular appearance
1. Small vertical projections, each composed of stratified squamous epithelium and a central core of connective tissue
Denture-Induced Fibrous Hyperplasia (Epulis Fissuratum, Inflamatory hyperplasia)
A Etiology—irritation caused by a denture flange, which produces a proliferation of tissue in the vestibule along the denture boarder
B Age and gender related—denture wearers; no gender predilection
C Location—vestibule along denture border; alveolar ridge in regions along the denture border
D Clinical features (Figure 8-8)
1. Exophytic folds of hyperplastic tissue in the vestibule under or around the denture flange
Peripheral Giant Cell Granuloma
A Etiology—a reactive lesion caused by local irritants
B Age and gender related—40 to 60 years; more common in females (2 : 1)
C Location—gingiva or alveolar process, anterior to molars
D Clinical features (Figure 8-9, A)
1. Exophytic lesion 0.5 to 2.0 cm in diameter
3. Pedunculated or sessile base
4. Arises from a deeper area in tissue than does a pyogenic granuloma or fibroma
E Radiographic appearance—this soft tissue lesion can cause superficial destruction of alveolar bone
Central Giant Cell Granuloma
A Etiology—occurs within bone; trauma caused by a fall, blow, or tooth extraction
B Age and gender related—children and young adults; more common in females (2 : 1) age 10–30 years
C Location—75% in the anterior segment of the mandible; also found in the maxilla
1. Appears as a swelling or bulge resulting from the expansion of cortical plates
2. No symptoms, so may be discovered by chance
3. A similar lesion, often called “brown tumor,” occurs in persons with hyperparathyroidism; resolves without treatment
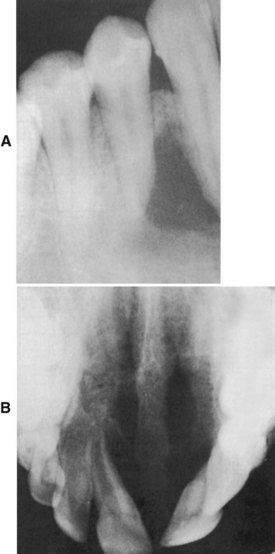
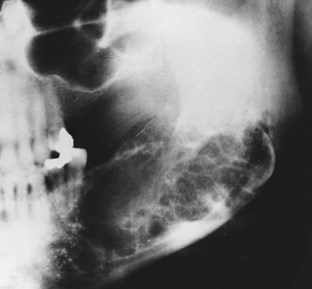
E Radiographic appearance (Figure 8-10, A and B)
1. Usually a large radiolucent area with diffuse margins that are ill defined with faint trabeculae
2. Displacement of teeth; divergence of the roots of teeth adjacent to the lesion
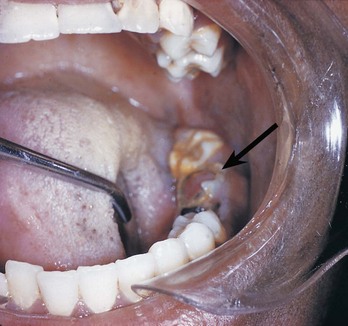
Chronic Hyperplastic Pulpitis (Pulpal Granuloma, Pulp Polyp)
A Etiology—excessive proliferation of inflamed pulp tissue found in teeth with large open carious lesions; rapid caries; lesion projects from the pulp chamber
B Age and gender related—children and young adults; no gender predilection
D Clinical features (Figure 8-11)
1. Red to pink outgrowth of pulp tissue protruding from the occlusal surface of the crown of a tooth that has a large, open, carious lesion
2. Lesion is not painful because hyperplastic tissue contains few nerves
Internal Resorption
A Etiology—not clear; theories include:
B Age and gender related—any age; no gender predilection
C Location—usually found within a tooth in the permanent dentition
1. Dentin immediately surrounding the pulp in the area of resorption is destroyed
2. The crown may appear pink (“pink tooth”) because of the vascularity of the lesion within (this is not easily observable on posterior teeth)
E Radiographic appearance well defined, but radiolucent lesion in close proximity to the pulp canal (Figure 8-12)
F Histologic characteristics—highly vascularized chronic inflammatory tissue
G Treatment—endodontic therapy if perforation of the root has not occurred; otherwise, extraction of the tooth is performed
Periapical Granuloma
A Etiology—dental caries or deep restorations
B Age and gender related—any age; no gender predilection
C Location—apex of a nonvital tooth
1. Nonvital tooth; asymptomatic
2. Fistula or parulis may be present if the condition has been chronic
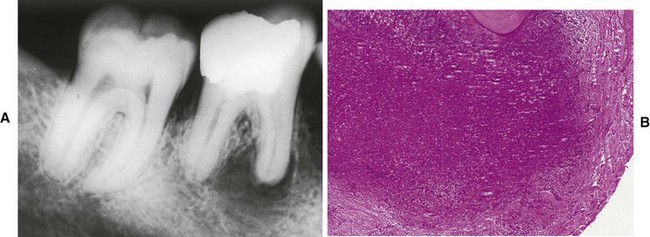
E Radiographic appearance—varies from a well-defined, circular, radiolucent lesion at the apex of the involved tooth to a diffuse radiolucency or thickening of the periodontal ligament space (Figure 8-13, A)
F Histologic characteristics (see Figure 8-13, B)
G Treatment—endodontic therapy or extraction of the affected tooth
Benign Intraosseous Neoplasms
Osteoma
A Etiology—asymptomatic benign tumor of compact bone; etiology generally unknown, but the cause may be irritation or inflammation; associated with a genetic condition called Gardner syndrome
B Age and gender related—more common in young adults but can be found at any age; no gender predilection
C Location—most common posterior mandible; mandibular condyle; craniofacial skeleton
D Clinical features—the affected individual may be unaware of the lesion because it grows slowly; considerable growth must occur before cortical plates expand
E Radiographic appearance—well-circumscribed radiopaque mass that is indistinguishable from scar bone; panoramic or lateral plate radiograph may be needed to view the lesion in its entirety (Figure 8-14)
F Histologic characteristics—extremely dense, compact bone or coarse, cancellous bone
Chondroma
A Etiology—benign tumors of hyaline cartilage; cause unknown
B Age and gender related—ages 30 to 40 years; no gender predilection
2. Mandible—posterior to canines
3. May involve the body of the mandible or the coronoid or condylar process
E Radiographic appearance—irregular radiolucent or mottled area in bone; may displace surrounding teeth or cause root resorption
Odontogenic Myxoma
A Etiology—unknown; benign; originates from mesenchymal tissue of the tooth germ
B Age and gender related—most often in young adults (ages 10 to 30 years); no gender predilection
C Location—mandible more often than maxilla
D Clinical features—deeply situated lesion; small lesions asymptomatic
E Radiographic appearance (Figure 8-15)
1. May be unilocular or multilocular
2. Several small radiolucencies occurring in groups, giving a “honeycomb” appearance
3. May show displaced teeth, mandibular canal, and antrum (may also invade the antrum)
4. Peripheral borders are irregular, diffuse, and not well defined
Exostosis
Torus Palatinus
A Etiology—inherited, autosomal dominant; some believe the cause to be genetic or environmental factors
B Age and gender related—usually seen by the age of puberty; rarely observed in children, but peak incidence occurs before 30 years; more common in females (2 : 1)
C Location—midline of the hard palate
D Clinical features (Figure 8-16, A)
1. Bony, hard protuberance in the midline in a variety of shapes—nodular; lobulated; smooth; spindle
2. Occurs in 20% to 35% of the U.S. population
3. Torus may appear ulcerated because of trauma to the thin overlying mucosa
E Radiographic appearance—dense radiopaque area
F Histologic characteristics—dense cortical bone
G Treatment—usually none, but surgical removal if the lesion interferes with a prosthodontic appliance
Torus Mandibularis
A Etiology—inherited, autosomal dominant; possibly genetic or environmental
B Age and gender related—first observed in early teen years; slightly more common in males
C Location—lingual surface of the mandible above the mylohyoid line in the area of premolars
D Clinical features (see Figure 8-16, B)
1. Bony, hard protuberance varying in size and shape; common exostosis
E Radiographic appearance—dense radiopaque area
F Histologic characteristics—dense cortical bone
G Treatment—surgical excision if the lesion interferes with a prosthodontic appliance
Odontoma
A Etiology—most common odontogenic tumor composed of all tooth structure and pulp but not considered a neoplasm
B Age and gender related—usually seen in adolescents and young adults (mean age 14 years); no gender predilection
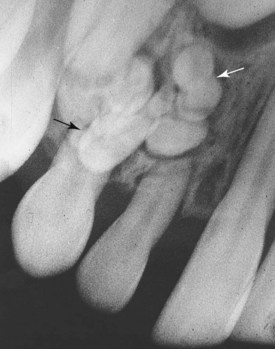
C Location—more frequently seen in the maxilla (especially the anterior maxilla for the compound type) than in the mandible; usually between the roots of teeth or near apices; complex odontomas seen more often in the posterior of the mandible
E Radiographic appearance—irregular mass of radiopacities (“tooth-like structures”) surrounded by a narrow radiolucent halo
F Histologic characteristics—tumor in which epithelial and mesenchymal cells show differentiation, resulting in abnormal enamel and dentin formation
Gingival Fibromatosis
General Characteristics
Irritative Fibromatosis
A Etiology—irritant such as mouth breathing, orthodontic appliances, bacterial plaque biofilm, dental calculus, debris, overhanging restorations, or ill-fitting dental appliances
B Age and gender related—any age; no gender predilection
C Location—localized areas on interproximal papillae; in mouth breathers, on maxillary and mandibular anterior labial gingivae
D Clinical features—solitary round, smooth-surfaced, pink enlargement of papillae; well attached to surrounding structures
E Histologic characteristics—proliferation of dense, fibrous connective tissue with an increase in the number of fibroblasts
Hereditary Gingival Fibromatosis (Gingival Lesions of Genetic Origin)
A Etiology (see the section on “Genetics” in Chapter 7)
1. Hereditary; believed to have genetic or developmental involvement or to be related to hormonal imbalances; a component of several syndromes (e.g., Zimmerman-Laband, Cross, Rutherfurd, Murray-Puretic-Drescher, and Cowden’s syndromes)
2. Contributing factors include poor oral hygiene, food impaction, calculus, malocclusion
3. Other conditions associated with gingival fibromatosis may include growth hormone deficiency, hypothyroidism, epilepsy, and intellectual and developmental disabilities (IDD)
B Age and gender related—appears during the eruption of primary or permanent teeth; slightly more common in females
C Location—excessive enlargement of interproximal gingival tissues; can be localized
1. Gingival enlargement may be generalized or localized
2. Diffuse, smooth-surfaced, pink, firm tissue involving the interproximal papillae
3. Multiple protruding pink, stippled, firm masses; labial and buccal areas are most affected; teeth may be displaced; delays eruption of teeth
E Histologic characteristics—bundles of fibrous connective tissue with fibroblasts and fibrocytes (depending on the formative stage)
Chemical Fibromatosis (Drug-influenced Gingival Enlargement)
A Etiology—reaction to drugs, specifically phenytoin (Dilantin); calcium channel blockers including nifedipine (Procardia), amlodipine (Norvasc), diltiazem (Cardizem), and verapamil (Calan); cyclosporin, an immunosuppressant drug given in association with organ transplants
B Age and gender—no gender predilection
C Location—papillae and gingivae
D Clinical features—smooth, pink, firm enlargement of the papillae (Figure 8-19)
E Histologic characteristics—extensive proliferation of connective tissue
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses