Chapter 6
Management of Impacted Teeth
Aim
To discuss the assessment and describe the surgical management of impacted teeth.
Outcome
After reading this chapter, you should have an understanding of the assessment of impacted teeth, and how such teeth should be managed.
Impacted Teeth
Impacted teeth are frequently found during routine clinical and radiographic examination. Once discovered, the clinician has to decide whether or not the tooth should be removed. Once the decision to remove the tooth has been made, the method of anaesthesia and surgical technique should be selected. This has to be done with an appreciation of the potential surgical complications.
What is an Impacted Tooth?
Impaction occurs when there is prevention of complete eruption into a normal functional position within the dental arch, caused by obstruction by another tooth, or development of the tooth in an abnormal position.
Which Teeth Become Impacted?
The tooth most commonly impacted is the mandibular third molar, with the maxillary canine the second most frequently impacted tooth with a prevalence of 1.7%.
Assessment of Impacted Teeth
Once an impacted tooth has been discovered, its position relative to the surrounding structures needs be assessed. This is usually done radiographically (Fig 6-1). Once the position of the tooth has been established, the clinician has to decide what to do about it.

Fig 6-1 Radiograph showing a horizontally impacted right mandibular wisdom tooth. The roots are lying close to the inferior alveolar nerve canal which can be clearly seen.
The decision to remove a symptomatic tooth is usually straightforward. This is guided by the need to relieve the patient’s symptoms, such as pain or infection. The difficulty arises with asymptomatic impacted teeth found during routine clinical examination or, more frequently, by radiographic examination (Fig 6-2).
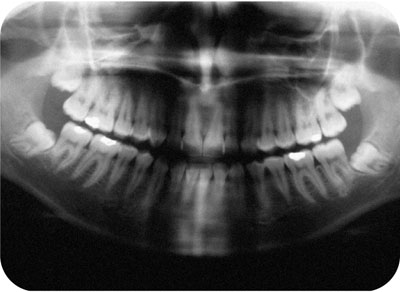
Fig 6-2 A dental panoramic radiograph showing four unerupted and impacted third molar teeth. The roots of both mandibular third molars are in close proximity to their respective inferior alveolar nerve canals.
There are a number of treatment options. The tooth can be left alone with periodic assessment; it can be surgically removed, or surgically exposed to encourage spontaneous eruption or facilitate orthodontic alignment. A further option of tooth transplantation may also be considered in certain circumstances (see Chapter 8).
Foremost in the decision-making process should be the wish of the patient, who must make the final decision. This judgment will normally be based on guidance given by the clinician. This should include indications for and against any proposed treatment. The different options are described below.
Observation of an Impacted Tooth
Doing nothing is a decision that often finds great favour with the patient. Although there may be no indication to remove the impacted tooth at that point in time, the patient should be made aware of any potential future complications that the impacted tooth may cause, when left untreated. Tooth movement, resorption of adjacent teeth and cyst formation are the main risks (Figs 6-3 and 6-4).
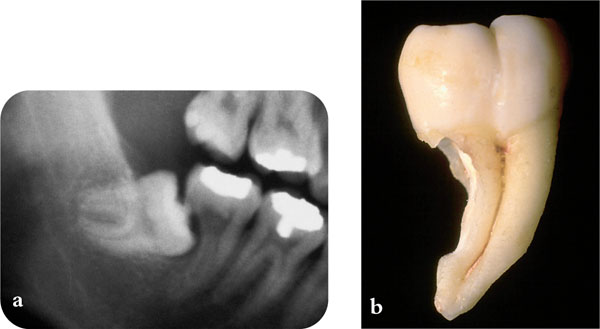
Fig 6-3 (a) This lower third molar has caused extensive resorption of the root of the adjacent second molar. (b) The degree of resorption can easily be seen on the extracted second molar.

Fig 6-4 A cyst associated with the crown of the unerupted left mandibular third molar, that has expanded to involve a large part of the mandible including the coronoid and condylar processes.
An impacted tooth that does not warrant treatment should be monitored periodically by both clinical and radiographic examination. This is to detect any change in position or a developing local pathology.
Surgical Removal of the Impacted Tooth
There are a number of indications for the surgical removal of an impacted tooth. Clinical guidelines such as those produced by the UK National Institute for Clinical Excellence (NICE) are useful in this regard. The indications for surgery are described overleaf.
Infection
When there is a history of infection, in particular recurrent infection, this is usually localised – such as pericoronitis, which is the commonest reason for the removal of impacted third molars (Fig 6-5). Cellulitis or abscess formation can also occur in relation to impacted teeth (Fig 6-6).

Fig 6-5 Pericoronitis associated with a partially erupted left mandibular wisdom tooth.

Fig 6-6 Cellulitis associated with an impacted left mandibular wisdom tooth.
Caries
The impacted tooth should be removed when it is carious, or when it is the cause of caries in an adjacent tooth (Fig 6-7).
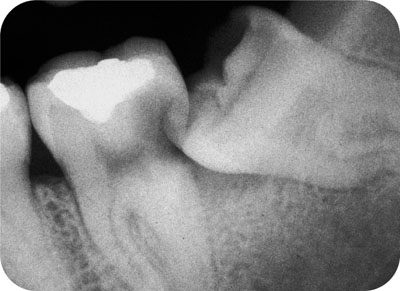
Fig 6-7 Caries in the distal aspect of the second molar due to the impacted third molar.
Pulpal or Periodontal Pathology
The presence of pulpal and/or periapical pathology is an indication for removal of an impacted tooth.
Periodontal disease, in particular when associated with an adjacent tooth, can often be arrested by removing the impacted tooth.
Resorption
When an impacted tooth has developed internal or external resorption, or there is resorption of an adjacent tooth (Fig 6-3), it should be removed. This can be a major problem in adolescent patients, in whom root resorption of the incisor teeth can be expected in about 12.5% of incisors adjacent to an ectopic canine (Figs 6-8 to 6-9).
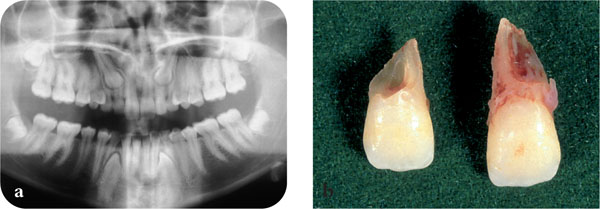
Fig 6-8 (a) Both maxillary canines have caused extensive resorption of the roots of the permanent lateral incisor teeth. (b) The extracted lateral incisor teeth showing extensive root resorption.
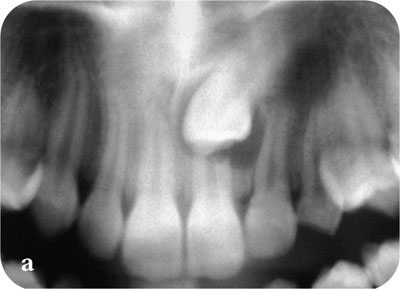
Fig 6-9 Even the roots of central incisor teeth may be resorbed by ectopic canine teeth.
Other Pathology
Impacted teeth should be removed if they are the cause of, or are associated with, pathology. Examples include disease of the follicle associated with the crown of an unerupted impacted tooth. This may be a cyst or tumour.
When an impacted tooth is lying in the line of a fracture it may be removed if it interferes with fracture reduction. This is often the case with impacted mandibular third molar teeth (Fig 6-10).

Fig 6-10 A fracture of the mandible passing through the socket of the unerupted third molar.
To Aid other Treatment
Removal of an impacted tooth may be indicated to allow:
-
the orthodontic alignment of the adjacent teeth
-
orthognathic or reconstructive surgery of the jaws. Impacted mandibular third molars are often removed around nine months prior to a sagittal splint mandibular osteotomy to facilitate surgery and reduce morbidity
-
restorative treatments such as the placement of a fixed prosthesis o/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


