6
Growth and Development
Case 1
Orthodontic Documentation, Evaluation, and Assessment
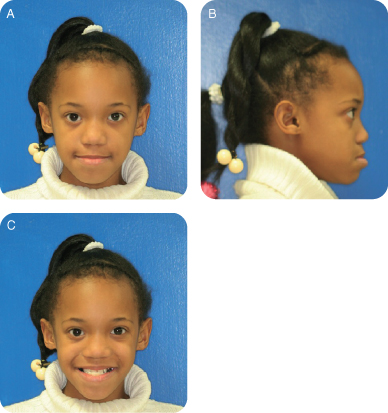
Figure 6.1.1a–c. Frontal, lateral, and frontal smiling extra-oral photos
A. Presenting Patient
- 8-year-, 5-month-old African-American female
B. Chief Complaint
- Mom’s complaint is that her daughter’s “lower jaw is too far forward”
C. Social History
- Patient is an active middle school student
- Both parents are teachers in local middle school
D. Medical History
- Non-contributory
E. Medical Consult
- Not necessary at this time
F. Dental History
- Seen for routine dental maintenance visits by her pediatric dentist after having comprehensive restorative care as a preschooler
- Optimal water fluoridation levels (city water)
- Dietary assessment is satisfactory
- Supervised brushing
G. Extra-oral Exam
- Concave and forward sloping, facial profile secondary to apparent mandibular prognathia
- Otherwise, fairly symmetrical facial features
H. Intra-oral Exam
- Transitional dentition
- Overbite: 2 mm, with -3 mm overjet and anterior crossbite
- Soft tissue within normal limits
- Mild plaque accumulation
- Caries free, but multiple restorations
Figure 6.1.2a–e. Intra-oral photos showing all views

I. Diagnostic Tools
- Full mouth radiographs and panoramic view
- Lateral cephalometric radiograph
- Well trimmed orthodontic study models
- Comprehensive orthodontic treatment requires a proper assessment to be done prior to initiation of care, including a questionnaire of the patient (medical/dental history, chief complaint, etc.), examination (oral health, function, and facial proportions) and diagnostic records
- Comprehensive diagnostic records include dental study models, an 8 series photographic collage, complete intra-oral radiographs, a cephalometric radiograph including tracing, and an anterior-posterior radiograph when indicated (for example, when there is a possible facial or occlusal asymmetry). Some adjustment in this standard will more than likely be forthcoming, with the use of cone beam computed tomography (CBCT) becoming more commonplace.
- Although it is generally understood that comprehensive orthodontic treatment requires this complete record documentation, questions often arise as to how many diagnostic records are needed for minor or interceptive treatment. While this can vary from case to case, the main concept is to ensure a full and complete diagnosis of the problem being evaluated so that the treatment addresses this problem and does not overlook confounding conditions. Dental versus skeletal crossbite correction is a good example. In the case of a simple, one-tooth anterior crossbite caused by dental tipping, dental study models or a photographic collage may be enough for documentation. However, if the patient appears to have an anterior crossbite because of a skeletal alignment problem, comprehensive diagnostic records are essential. When in doubt, a more thorough evaluation may be the most prudent approach
- See the American Academy of Pediatric Dentistry (AAPD) Guidelines on Management of the Developing Dentition and the American Board of Orthodontics Case Report Preparation
Figure 6.1.3. Panoramic radiograph
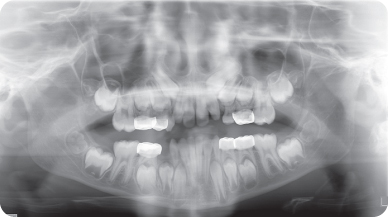
Figure 6.1.4. Cephalometric radiograph

J. Differential Diagnosis
- Maxillary deficiency or mandibular prognathia
K. Diagnosis and/or Problem List
Diagnosis
- Class III mixed dentition malocclusion
Problem List
- Class III skeletal and dental classification
- Anterior crossbite with significant negative overjet
- Informed consent is basically a discussion and documentation of the treatment to be rendered, as well as the risks, benefits and alternatives to this treatment
- Common orthodontic treatment risks to be covered during consent include caries, root resorption, periodontal disease, necrotic pulp, discomfort, trauma, temporomandibular joint disorder (TMD) considerations, impacted teeth, length of treatment, prognosis, and relapse
- Many examples of orthodontic informed consent forms are readily available and should be used by practitioners prior to treatment. Inherent in the concept of informed consent, however, is that these forms must be reviewed with the patient by the practitioner to ensure an understanding by the patient and parent
- See The Orthodontic CYBERjournal (http://www.oc-j.com/dec00/risks.htm) and the American Academy of Pediatric Dentistry Guidelines on Informed Consent (AAPD 2011–12b)
L. Comprehensive Treatment Plan
- Comprehensive orthodontic care to include two-phase treatment consisting of protraction headgear in phase one and comprehensive bracketing in phase two
M. Post-Operative Intra-oral Photographs
- N/A
N. Prognosis and Discussion
- The prognosis is guarded and the need for orthognathic surgery cannot be ruled out
O. Complications and Alternative Treatment Plan
- Complications to this patient’s care include the possibility of poor compliance or lack of protraction headgear treatment response, even with good compliance
- Alternative treatment could include waiting until growth is complete and addressing the skeletal discrepancy surgically
Self-study Questions
1. What are the three basic components of a comprehensive orthodontic assessment for a patient?
2. Is it true that diagnostic records for orthodontic patients must include a cephalometric evaluation?
3. What new imaging technique may influence substantial changes in the way comprehensive orthodontic assessments have been done in the past?
4. Name the four broad areas of treatment that need to be covered during the process of informed consent
5. What are the most common specific areas covered when reviewing orthodontic informed consent with a patient?
Answers are located at the end of the case.
Bibliography
American Academy of Pediatric Dentistry. 2011–2012a. Guidelines on management of the developing dentition, Reference Manual. Pediatric Dentistry 33(6), pp. 229–41.
American Academy of Pediatric Dentistry. 2011–2012b. Guideline on Informed Consent, Reference Manual. Pediatric Dentistry 33(6), pp. 285–7.
Proffit WR, Sarver DM, Ackerman JL. 2007. Orthodontic diagnosis: The development of a problem list. In: Contemporary Orthodontics, 4th edition. Proffit WR, Fields HW, Sarver DM (eds) Elsevier Publishing, St Louis. pp 167–233.
SELF-STUDY ANSWERS
1. Patient questionnaire, examination (oral health, function, and facial proportions), and diagnostic records
2. No, this is not true. Depending on the severity of the patient’s problem, certain orthodontic records may not be necessary
3. Cone beam computer tomography (CBCT) may eliminate the need to make separate dental study models, intra-oral radiographs, and cephalometric radiographs because all three of these items can be captured in the 3-dimensional CBCT image
4. Type of treatment to be rendered, the risks, the benefits, and the alternatives to this treatment
5. Risk for caries, root resorption, periodontal disease, necrotic pulp, discomfort, trauma, temporomandibular joint disorder (TMD), impacted teeth, length of treatment, prognosis, and relapse
Case 2
Space Management: Premature Loss of Primary Second Molar in Preschool Child
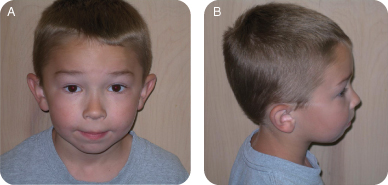
Figure 6.2.1a–b. Facial photographs
A. Presenting Patient
- 3-year-, 10-month-old Caucasian male
B. Chief Complaint
- Mother states, “My son has a bunch of cavities and pain in an upper left tooth”
C. Social History
- Patient is in preschool daycare
- Parents are divorced, no siblings
- Mother is the primary caregiver and works a full-time job
- Socio-economic status is low
D. Medical History
- Non-contributory
E. Medical Consult
- Not necessary at this time
F. Dental History
- Optimal water fluoridation levels (city water)
- Highly cariogenic diet
- Unsupervised brushing
G. Extra-oral Exam
- Normal facial symmetry with convex facial profile
H. Intra-oral Exam
- Primary dentition with distal step primary molar terminal plane
- 6-mm-deep overbite with 2-mm overjet, adequate dental spacing and arch circumference
- Soft tissue within normal limits
- Moderate plaque accumulation
- Extensive severe dental decay, including sensitivity to percussion on several teeth
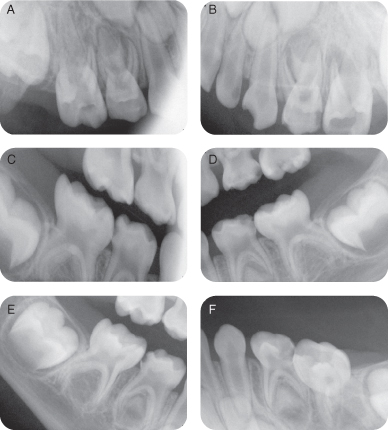
I. Diagnostic Tools
- Pre-op radiographs: Four periapicals and two bitewings
- Severe dental decay noted
- Periapical pathology noted with maxillary second molars
- Obtain a thorough medical history to determine if a patient can tolerate intra-tissue metal extensions (distal shoe) in the oral cavity. For example, is there a history of a congenital heart defect, heart surgery or bleeding disorder?
- Obtain a thorough dental history to manage all oral health problems, including restorative, preventive, educational, in conjunction with the space maintenance care
- Consider occlusal relationships and options for management of the early loss of the second primary molars. Which treatment will provide the most benefit with the least drawbacks?
Figure 6.2.2a–f. Pre-op radiographs
J. Differential Diagnosis
- N/A
K. Diagnosis and Problem List
Diagnosis
- Early childhood caries
- Poor diet
- Poor oral hygiene
Problem List
- High caries risk due to poor diet and oral hygiene
- Premature loss of the maxillary second primary molars
L. Comprehensive Treatment Plan
- A detailed informed consent should be obtained for this care. The patient will receive posterior stainless steel crowns, extraction of the maxillary right and left second primary molars, and placement of two distal shoe space maintainers to guide the eruption of the maxillary right and left first permanent molars
- Establish a dental home and aggressive preventive care to include caries risk assessment, parent education, adequate oral hygiene, fluoride varnish, and special maintenance intervals tailored to the responsiveness of the parent and child to the preventive care
- Prevent malocclusion with use of distal step primary molar terminal plane
- Maintain distal shoe space maintainer and eventually follow up with replacement bilateral maxillary lingual arch (Nance appliance)
M. Post-operative Intra-oral Photographs
- Post-op photos and panoramic radiograph were obtained at age 5 years, 5 months, showing stainless steel crowns and distal shoe space maintainers all in good repair
- The second primary molar is essential to the proper eruption and positioning of the first permanent molar, which is an essential tooth in establishing a normal permanent dentition occlusion
- Early loss of the second primary molar can lead to multiple occlusal problems such as space loss and altered eruption; however, these problems can be prevented with proper space maintenance
- While there are a few ways to address premature loss of this primary tooth, maintenance of its space minimizes orthodontic correction problems
- Distal shoe space maintainers or acrylic pressure (free-end) appliances are useful in guiding the eruption of the first permanent molar, but require some careful management and close follow-up
Figure 6.2.3a–b. Intra-oral photos showing space maintenance appliances in maxillary arch
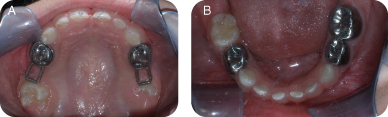
Figure 6.2.4. Post-op panoramic radiograph at age 5 yrs 5 mo

N. Prognosis and Discussion
- Prognosis for caries is now good secondary to compliance with the aggressive preventive plan that was implemented
- Prognosis for preventive occlusion management (space maintainers) is good secondary to success to date with the bilateral distal shoes and initial eruption of the first permanent molars. It will be essential that the patient continue regular dental visits to have the distal shoes removed and a bilateral maxillary lingual arch (Nance appliance) placed, once the first permanent molars are erupted far enough for banding
O. Complications and Alternative Treatment Plan
- Complications to this patient’s care could include premature loss of the distal shoes, mismanagement of the distal shoes (particularly if the first permanent molars erupted under the most gingival aspect of the distal shoe blades), and lack of adequate follow-up by the mother
Self-study Questions
1. What alternative management plans related to the maxillary second primary molars were available for this patient at the initiation of care?
2. What alternatives to bilateral distal shoes could be considered as this patient matures?
3. What angulation is usually built into the distal shoe blades from an occlusal to gingival direction and why?
4. What about this patient’s occlusal relationships presents a positive prognosis regarding the need for future orthodontic care?
5. What about this patient’s occlusal relationships presents a negative prognosis regarding the need for future orthodontic care?
Answers are located at the end of the case.
Bibliography
Barberia E, Lucayechi T, Cardenas D, Maroto M. 2006. Free-end space maintainers: design, utilization and advantages. J Clin Pediatr Dent 31(1):5–8.
Brill WA. 2002. The distal shoe space maintainer chairside fabrication and clinical performance. Pediatr Dent 24(6): 561–5.
Durward CS. 2001. Space maintenance in the primary and mixed dentition. Ann R Austral Coll Dent Surg 15:203–5.
Terlaje RD, Donly KJ. 2001. Treatment planning for space maintenance in the primary and mixed dentition. J Dent Child 68(2):109–14.
SELF-STUDY ANSWERS
1. Aggressive pulpectomies of the second primary molars, although given the clinical signs and symptoms and the periapical radiographic appearance, particularly the maxillary left second primary molar, the prognosis is questionable
2. Either no space management at this time, permitting the permanent molars to drift mesially and impacting the second premolars, or the use of a removable acrylic pressure appliance that would guide the first permanent molars via pressure and without penetrating the alveolar mucosa
3. Angled mesially to help prevent the first permanent molar from getting impacted under the distal shoe blade
4. Adequate primary dentition spacing needed for the transition into the full permanent dentition
5. Deep overbite, distal step primary molar terminal plane and convex facial profile that would most likely lead to a class II deep overbite relationship in the permanent dentition
Case 3
Bilateral Space Management in the Mixed Dentition
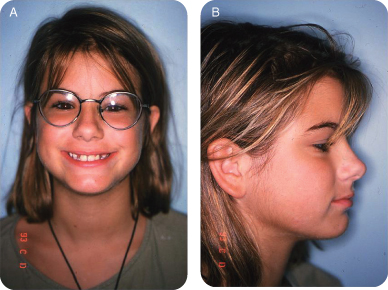
Figure 6.3.1a–b. Facial photographs
A. Presenting Patient
- 12-year-old Caucasian female
B. Chief Complaint
- Mom states, “My child has crooked and missing teeth”
C. Social History
- Patient is a happy, well developed adolescent
- Lives with mother and father
- Middle class socio-economic status
- One younger brother
D. Medical History
- Non-contributory
E. Medical Consult
- Not necessary at this time
F. Dental History
- Regular dental maintenance visits
- Optimal water fluoridation levels (city water)
- Fairly healthy diet with low caries risk
- Supervised brushing
G. Extra-oral Exam
- Normal facial symmetry with slightly convex facial profile
H. Intra-oral Exam
- Healthy mixed dentition with lower lingual arch in place (Figure 6.3.2)
- 4-mm overbite with 1 mm-overjet
- Soft tissue within normal limits
- Mild plaque accumulation
- Good oral hygiene
- Caries free with sound pit and fissure sealants on the first permanent molars
Figure 6.3.2a–c. Intra-oral photos showing bilateral space maintenance appliance

I. Diagnostic Tools
- Panoramic radiograph reveals congenitally missing and ectopically erupting teeth (Figure/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


