Gingival Diseases
Gwen Essex, Dorothy A. Perry, Based on the original work by
• Define the types of gingivitis.
• Relate the clinical signs and symptoms of gingivitis to the pathogenesis of each stage of disease.
• List the similarities and differences in the clinical presentation, treatment, and healing of dental plaque biofilm–induced gingivitis and other gingival conditions.
• Identify the medications that can cause gingival hyperplasia in patients.
• Describe examples of bacterial, viral, and fungal infections that affect the gingiva.
• Define necrotizing ulcerative gingivitis.
• List the relatively common systemic conditions that have gingival manifestations.
• Describe the role of the dental hygienist in the treatment of gingivitis.
A description of the gingival tissues in health is presented in Chapter 2. To review, in health, the gingival epithelium is usually described as pink or coral pink, with significant variation based on the presence of melanin in the tissue, which is a genetic characteristic. The attached gingiva is tightly bound to the underlying connective tissue and is not movable. The surface epithelium of the attached gingiva is often stippled, shows no signs of inflammatory color changes, and the papillae fill the interdental spaces completely. The marginal gingiva reaches the tooth surface in a knife edge pattern, and there are measurable sulcus depths of less than 3 mm. The gingival epithelium consists of a keratinized oral epithelium, a keratinized or parakeratinized sulcular epithelium, and a junctional epithelium that forms the attachment to the root surface. Beneath the gingival epithelium, there is dense connective tissue coronal to the alveolar bone. This tissue is laced with bundles of collagen fibers. The normal appearance of healthy gingiva is shown in Figure 6-1.
Gingivitis
Gingivitis is inflammation of the gingival tissues. It occurs in a periodontium with no attachment loss or in a periodontium with attachment loss that is not progressing. Gingivitis manifests as color change (redness), edema (swelling of the tissues), exudate (drainage of gingival fluid from the sulcus), and a tendency to bleed readily (hemorrhage in response to gentle periodontal probing or tooth brushing).1 In addition, there may be changes in gingival contour, loss of tissue adaptation to the teeth, and an increased flow of gingival crevicular fluid.2 Gingivitis is perhaps the most common human disease and among the easiest to treat and control. However, gingivitis is painless and often unrecognized. Many patients are unaware that they have it, even though their gums bleed, and, because it is so common, dentists and dental hygienists frequently do not emphasize its importance. Perhaps the best approach that dental hygienists and dentists can take is to inform their patients that they have a disease—gingivitis—and that it is easily treated and cured. When the balance between disease and health is understood, patients often cooperate with dental hygiene care and improve their daily oral hygiene practice to cure the disease.
Pathogenesis of Gingival Disease
Research has also defined a fourth stage, characterized by the extension of inflammation into the alveolar bone, which is the stage of periodontal breakdown, or advanced stage.4 The fourth stage is the point at which the gingival disease has progressed to periodontal disease.
Stage I Gingivitis (Initial or Subclinical Stage)
Stage I gingivitis, the initial stage, occurs in the first few days of contact between microbial plaque and the gingival tissues. This stage is an acute inflammatory response that is characterized by dilation of the blood vessels and increased blood flow. The polymorphonuclear leukocytes (PMNs, or neutrophils) attach to the vessel walls and begin to migrate into the surrounding connective tissues. PMNs (white blood cells with multilobulated nuclei) are the principal defense in acute inflammation. They phagocytize (engulf) bacteria, their products, and other products of destroyed tissue. Small amounts of plasma also leak into the surrounding tissues, causing edema in the tissues. PMNs amass in the connective tissue and migrate through the sulcular epithelium into the plaque, forming exudate. Exudate from early gingival inflammation, composed mostly of serum, is referred to as gingival fluid flow. The gingival fluid is clear, not yellow (like pus), because few cells are present. A significant number of lymphocytes appear in the gingival connective tissues. These are almost all T lymphocytes, the type that do not cause tissue damage but maintain a homeostatic (stabilizing) response to bacterial infection.5 In addition, there are epithelial cell changes and collagen degradation caused by activation of the host immune system. These first tissue reactions to plaque infection are not visible in the gingival tissues because they do not cause obvious clinical changes. This initial inflammatory response with no outwardly observable clinical signs is a subclinical infection.4
Stage II Gingivitis (Early Stage)
Stage II gingivitis is referred to as early gingivitis. Lesions begin to form 4 to 7 days after plaque has accumulated in the gingival sulcus. The T lymphocytes increase in number and are localized in the connective tissue under the epithelium of the gingival sulcus. The inflammatory exudate increases; it may appear white or yellow. Clinically, the tissues appear slightly red and swollen. The increase in gingival fluid flow (exudate) reaches its peak 6 to 12 days after clinical redness is observed. The perivascular collagen fibers in the connective tissues are destroyed by the inflammation and replaced by blood plasma and inflammatory cell infiltrate. Collagen fibers that attach the underlying connective tissue to the gingival epithelium are also destroyed and gingival stippling, if present, begins to disappear, causing the gingiva to appear shiny. The junctional epithelium begins to lengthen against the root surface and it is disrupted by the migrating PMNs and lymphocytes. The gingival tissues tend to bleed when gently probed and often do so when a patient brushes and flosses. Cellular changes occur in the connective tissue fibroblasts, leading to their destruction, probably related to interaction with the lymphoid tissues. The early stage of gingivitis may continue for 21 days or longer. It is the earliest clinical evidence of gingivitis.4
Stage III Gingivitis (Established Stage)
After 15 to 21 days, the gingival inflammation reaches the established stage, called stage III gingivitis.4 In established gingivitis, there is a distinct change in the type of white blood cells seen in histologic specimens. Plasma cells, usually associated with an intense antigen-antibody response, are present. T and B lymphocytes are found in equal amounts, indicating that tissue destruction by the inflammatory reaction is taking place. B lymphocytes are related to cell surface immunity and release lymphokines that accelerate the tissue destruction in inflammation. More connective tissue collagen is destroyed and the junctional epithelium begins to thicken and extend apically on the root surface and deep into the underlying connective tissues. This activity represents a conversion of the junctional epithelium into one correctly described as pocket epithelium. The clinical probing depth increases for two reasons: the periodontal probe penetrates more deeply through the junctional epithelium into the connective tissue by about 1 mm because of the loss of collagen, and edema in the tissues moves the gingival margin coronally, increasing the probe readings.
The established gingivitis lesion may persist unchanged for months or years. The condition is reversible when plaque is regularly removed, permitting the tissues to return to normal. When healing occurs, there is no residual tissue destruction.2
Stage IV Gingivitis (Advanced Stage)
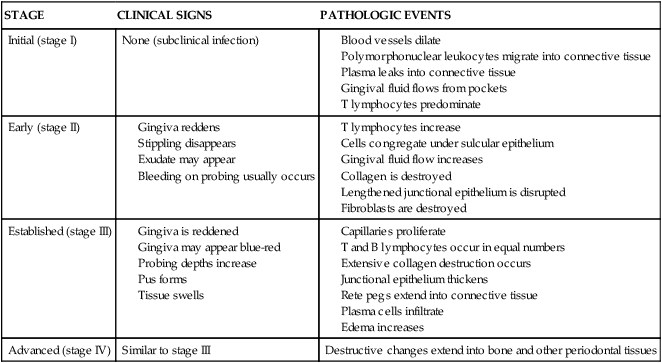
Stage IV gingivitis is the advanced stage of gingivitis. The inflammatory processes have extended beyond the gingiva and into the other periodontal tissues.4 The extension of disease into the bone, referred to as periodontitis, is described in Chapter 7. The pathogenesis of the stages of gingivitis is summarized in Table 6-1.
TABLE 6-1
Correlation of Clinical Signs to the Pathogenesis of Gingivitis
| STAGE | CLINICAL SIGNS | PATHOLOGIC EVENTS |
| Initial (stage I) | None (subclinical infection) |
Healing of the Gingiva After Treatment
In some cases, stable gingivitis transforms into progressive disease. This change results in advanced lesions with bone destruction, progressing from gingivitis to periodontitis.5 Periodontitis is discussed in Chapter 7.
Gingivitis has been classified into a number of categories on the basis of the clinical manifestations of the disease, etiology, association with systemic diseases, association with medications, or other causes. The gingiva mirrors the effects of many factors beyond disease-associated causes, including allergies and injuries. The classification of gingival diseases and conditions is complex and is presented in Box 6-1.5,6 The major elements of gingival diseases and conditions are described and illustrated in the remainder of this chapter.
Recession of the Gingiva
Recession of the gingiva refers to the location of the margin of the tissue, not its condition. Recession can occur in gingivitis, or it can be associated with clinically healthy tissue. Gingival recession, which is common, increases with age. It can be localized to one tooth or extend to any number of teeth. It has been reported to be present in 8% of children and 100% of adults by the age of 50 years. Etiologic factors associated with recession are as follows7:
Dental Plaque–Induced Gingival Disease
Gingivitis Associated with Dental Plaque Biofilm Only.
The most common form of gingivitis found in the general population is gingivitis associated with dental plaque only, also called plaque-associated gingivitis, or gingivitis. This disease is directly related to the presence of bacterial plaque on the tooth surface.1
Clinically, gingivitis causes a reddened gingival margin (with pocket formation as a result of gingival swelling and edema), hypertrophy, and deepened penetration of the periodontal probe on clinical evaluation. The surface of the gingiva may appear glazed or smooth, and stippling (when present in health) usually disappears. Microscopically, there is an increase in capillaries along the gingival margin and the epithelium lining the gingival sulcus is ulcerated. This ulceration results in a tendency to bleed when a periodontal probe is placed in the gingival crevice. Bleeding in response to gentle probing is the major clinical indicator of gingivitis. Another common feature of chronic gingivitis is a clear gingival fluid flow, or exudate, which appears to increase with the severity of the gingivitis. Figure 6-2 shows the typical appearance of dental plaque–induced gingivitis.

The clinical signs of plaque-associated gingivitis are an intense inflammatory response at the gingival margin and bleeding in response to gentle probing. The marginal gingiva is very red around the lower anterior teeth, and slight bleeding is evident at the gingival margin after probing.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



