Dental Implant Surgery
• Posterior Mandibular Implant Supported Fixed Partial Denture
• Posterior Maxillary Implant Supported Fixed Prostheses
• Contemporary Treatment Options for Edentulism
• Computer Assisted Implant Surgery
Posterior Mandibular Implant Supported Fixed Partial Denture
Examination
Examination of both the quality and quantity of bone is essential for successful implant placement.
Imaging
Although implant surgery can be planned on a panoramic radiograph with a surgical planning template coupled with bone mapping techniques, a far simpler and much more predictable methodology involves CBCT (Figure 6-1, A). The preoperative films show that the anterior implant site is 8.9 mm wide in a buccolingual dimension, 14.4 mm above the inferior alveolar neurovascular bundle, and 1.5 mm distal to the lower right mandibular cuspid tooth (Figure 6-1, B). At the proposed location of the more posterior implant, the buccolingual distance is 10.9 mm and the inferior alveolar neurovascular bundle lies 16.1 mm below the ridge crest (Figure 6-1, C). The bone quality is type II (Box 6-1). A surgical guide can be generated from the data contained in the CBCT if the surgeon feels it is necessary, and instrumentation keyed to this guide can be applied for precision placement; otherwise, a surgical guide is prepared on the study models.

Figure 6-1 A, CBCT panoramic image showing proposed implant sites in the right mandible posterior. B, CBCT coronal cut showing anatomic features of the proposed anterior implant site, in addition to the proposed posterior implant site (C), and the measurements generated by the implant planning software. D, CBCT panoramic image showing implant placement completed as planned.
Treatment
Under intravenous sedation and local anesthesia, implant surgery was performed according to the particular system protocol. The wound was sutured with nonresorbable sutures, and a gauze sponge was placed to obtain hemostasis. The patient was recovered and discharged with detailed instructions for home care, analgesics, and a return appointment in 1 week for suture removal. Postoperative CBCT images (see Figure 6-1, D) revealed satisfactory placement of implants well above the mandibular canal, with adequate spacing for a three-unit fixed partial denture. A final restoration was placed 4 months later, and a satisfactory cosmetic and functional outcome resulted, with contours and emergence similar to those of the replaced natural dentition.
Complications
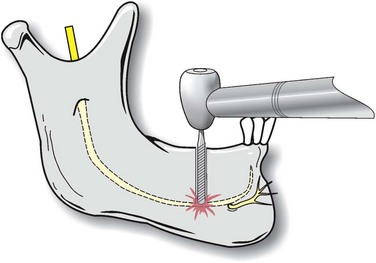
The direct anchorage of dental implants to the host surrounding bone (osseointegration) is a good indication of clinical success, and although a high success rate is seen in implantology, endosseous implants do fail. Early implant failure is associated with a lack of primary stability (possibly aggravated by early loading protocols), surgical trauma, and infection. Infection noted early is much more problematic than infection later in the course of treatment because of the disturbance in primary bone healing associated with the former. Occlusal overburden and peri-implantitis are the most important factors associated with delayed or late implant failure. The primary limiting factor for lower premolar and molar implants is the height of bone above the mandibular canal. If it is determined that an implant has been placed in contact with the mandibular canal, causing postoperative hypoesthesia or anesthesia, the implant should be backed off of this structure as soon as possible or removed and replaced with a shorter implant (Figure 6-2). CBCT, unlike a panoramic film, can differentiate superimposition from direct contact with the nerve. In the presence of symptoms (e.g., paresthesia) and a CBCT scan showing no direct contact with the nerve, removal of the implant is unlikely to resolve the paresthesia, and interval neurosensory testing determines whether microneurosurgical exploration is indicated.
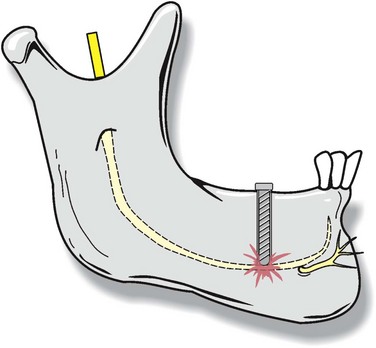
Figure 6-2 Injury to or contact with the inferior alveolar neurovascular bundle by an implant fixture.
Perforation with the implant drill and direct injury to the mandibular nerve are possible (Figure 6-3). Hemorrhage, salivary gland involvement, painful impingement of implants on the lingual surface of the mandible, and associated misalignment are all complications associated with lingually directed surgical misadventures. Such problems can be minimized by careful attention to the anatomic features of the lower posterior jaw as depicted on the CBCT. Frequently a slight buccal inclination of posterior mandibular implants is necessary to avoid lingual perforation, and this fact is best determined and discussed preoperatively with the restorative dentist to minimize misunderstandings. Should infection occur in the early postoperative period, conservative management, including antibiotics, debridement, incision and drainage, and irrigation, is indicated, with implant removal as a last resort. Occasionally, inflammation and the development of a fistula over an implant site occur, and this frequently indicates that the cover screw has loosened. In this case the implant site should be exposed, the screw removed, the site debrided and irrigated, and a new, sterile cover screw placed and tightened.
Ahmad, N, Saad, N. Effects of antibiotics on dental implants: a review. J Clin Med Res. 2012; 4:1–6.
Barewal, RM, Stanford, C, Weesner, TC. A randomized controlled clinical trial comparing the effects of three loading protocols on dental implant stability. Int J Oral Maxillofac Implants. 2012; 27:945–956.
Buser, D, Janner, SF, Wittneben, JG, et al. Ten-year survival and success rates of 511 titanium implants with a sand-blasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012; 14(6):839–851.
Lambert, PM, Morris, HF, Ochi, S. The influence of 0. 12% chlorhexidine digluconate rinses on the incidence of infectious complications and implant success. J Oral Maxillofac Surg. 1997; 55(12 Suppl 5):25–30.
Liddelow, G, Klineberg, I. Patient-related risk factors for implant therapy: a critique of pertinent literature. Aust Dent J. 2011; 56:417–426.
Marchand, F, Raskin, A, Dionnes-Hornes, A, et al. Dental implants and diabetes: conditions for success. Diabetes Metab. 2012; 38:14–19.
Misch, CE. Density of bone: effect on treatment plans, surgical approach, healing and progressive bone loading. Int J Oral Implantol. 1990; 6:23–31.
Renouard, F, Rangert, B. Risk factors in implant dentistry: simplified clinical analysis for predictable treatment, ed 2. Hanover Park, Ill: Quintessence; 2008.
Sakka, S, Baroudi, K, Nassani, MZ. Factors associated with early and late failure of dental implants. J Investig Clin Dent. 2012; 3(4):258–261.
Posterior Maxillary Implant Supported Fixed Prostheses
Imaging
A cone-beam computed tomography (CBCT) panoramic image (Figure 6-4, A) reveals that there is adequate bone for placement of implants in both areas selected, without the necessity of a sinus graft. The bone quality is judged to be type II. Bone quality is determined by radiographic appearance and also by the tactile feeling on drilling (see Box 6-1). If CBCT is not available, an implant tracing template at 25% larger than normal size (due to a 25% magnification factor on a panoramic radiograph) can be used with a panoramic radiographic image for surgical planning. CBCT helps to accurately determine the position of the floor of the maxillary sinus and the condition of the sinus membrane, which aids in determining the necessity and feasibility of sinus grafting. Coronal CBCT images in the area planned for the placement of the more anterior implant in this case (2 mm posterior to tooth #11) demonstrates that the buccolingual dimension is 7.55 mm, and a vertical height of 18.8 mm is available (Figure 6-4, B). In the area proposed for the placement of the more posterior implant, 8.16 mm is noted as the buccolingual dimension, and 12.65 mm of bone is present from the crest of the ridge to the floor of the right maxillary sinus (Figure 6-4, C). It is relatively uncommon to have adequate bone below the maxillary sinus for placement of implants of satisfactory length, as is seen in this case. Various strategies can be used when adequate volume is absent. Bone graft augmentation by open and closed technique using various graft materials (e.g., onlay grafting with particulate and/or block grafts of various natures), sinus membrane elevation followed by implant placement without grafting, and short implants are all methodologies used to overcome inadequate bone stock below the sinus floor in posterior maxillary constructs. Immediate, rather than delayed, implant placement in grafted sinuses is determined by the presence of at least 5 mm of bone, which allows for initial stability of immediately placed implants. In the case of two-stage sinus grafts, the primary graft placement is followed 4 months later by secondary implant surgery, with or without immediate loading as determined by initial stability at placement.
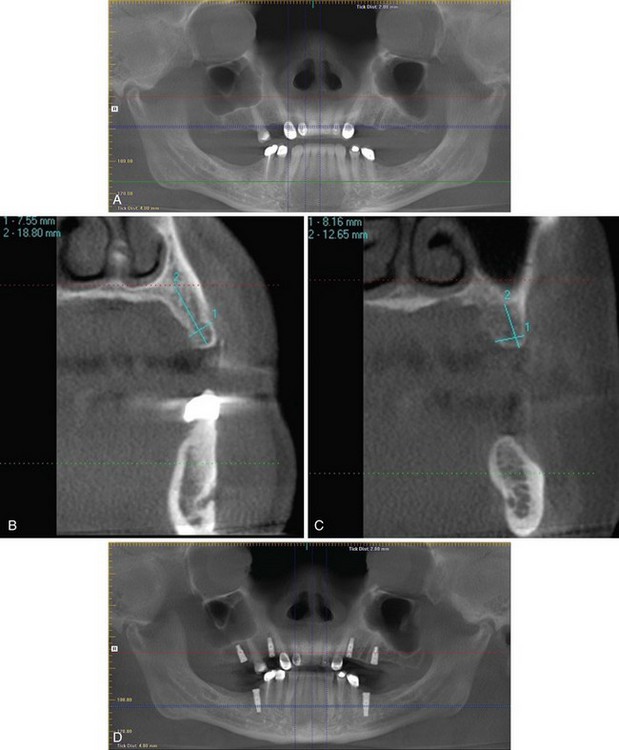
Figure 6-4 A, CBCT panoramic view showing proposed implant sites in right maxilla posterior. Quadrant CBCT coronal views showing the more anterior right maxillary implant site (B) and the more posterior right maxillary implant site (C), both with measurement data. D, Postoperative CBCT panoramic view showing implant placement in the right maxillary posterior, in addition to other fixtures placed at surgery (no sinus grafting was necessary).
Treatment
The planned surgery was discussed in detail with the restorative dentist, who showed the patient on a diagnostic wax-up what the final restoration will look like and has provided a surgical guide indicating the desired position and inclination for the implants. The patient had been off of clopidogrel for 6 days on presentation. He was given 2 gm of amoxicillin by mouth 1 hour before surgery, and chlorhexidine oral rinse was used immediately before surgery. Under intravenous sedation and local anesthesia, the implant surgery was performed in accordance with the manufacturer’s protocol. After the osteotomies were performed, the sites were probed with a blunt instrument, and the sinus floors were found to be intact at both sites. The implants were placed, and wound closure was obtained with 4-0 polyglactin (Vicryl) sutures. The patient recovered and was discharged with instructions for home care, analgesics, and a return appointment in 1 week for suture removal. Postoperative CBCT panoramic imaging revealed satisfactory implant placement (Figure 6-4, D).
Bahat, O. Brånemark system implants in the posterior maxilla: clinical study of 660 implants followed for 5 to 12 years. Int J Oral Maxillofac Implants. 2000; 15:646–653.
Benavides, E, Rios, HF, Ganz, SD, et al. Use of cone beam computed tomography in implant dentistry: the International Congress of Oral Implantologists consensus report. Implant Dent. 2012; 21:78–86.
Cheng-Ching, E, Samaniego, EA, Reddy Naravetla, B, et al. Update on pharmacology of antiplatelets, anticoagulants, and thrombolytics. Neurology. 2012; 79(13 Suppl 1):S68–S76.
Cho-Lee, GY, Naval-Gias, L, Castrejon-Castrejon, S, et al. A 12-year retrospective analytic study of the implant survival rate in 177 consecutive maxillary sinus augmentation procedures. Int J Oral Maxillofac Implants. 2010; 25:1019–1027.
Dent, CD, Olsen, JW, Farish, SE, et al. The influence of preoperative antibiotics on success of endosseous implants up to and including stage II surgery: a study of 2,641 implants. J Oral Maxillofac Surg. 1997; 55(Suppl 5):19–24.
Felice, P, Soardi, E, Pellegrino, G, et al. Treatment of the atrophic edentulous maxilla: short implants versus bone augmentation for placing longer implants: five-month post-loading results of a pilot randomised controlled trial. Eur J Oral Implantol. 2011; 4:191–202.
Kaufman, E. Maxillary sinus elevation surgery: an overview. J Esthet Restor Dent. 2003; 15:272–282.
Lambert, PM, Morris, HF, Ochi, S. The influence of 0. 12% chlorhexidine digluconate rinses on the incidence of infectious complications and implant success. J Oral Maxillofac Surg. 1997; 55(12 Suppl 5):25–30.
Liddelow, G, Klineberg, I. Patient-related risk factors for implant therapy: a critique of pertinent literature. Aust Dent J. 2011; 56:417–426.
Renouard, F, Rangert, B. Risk factors in implant dentistry: simplified clinical analysis for predictable treatment, ed 2. Hanover Park, Ill: Quintessence; 2008.
Sinus Grafting for Implants
Imaging
A panoramic cone-beam computed tomography (CBCT) image showed that there was inadequate bone beneath the maxillary sinus bilaterally (especially on the right) in the posterior maxilla to allow for adequate implant placement (Figure 6-5, A). A coronal CBCT cut (Figure 6-5, B) determined that an implant of 5 mm in diameter could be placed in the most posterior right maxilla site; however, only 3.6 mm of bone is present below the sinus membrane. Consequently, a sinus graft must be completed to place an implant of adequate length to support a fixed partial denture on two implants in this area of relatively high occlusal load. On the left side at the site of the more posterior implant, 9.7 mm of bone in the buccolingual dimension is seen, and 10 mm of bone is noted below the sinus floor in the area of the most posterior implant placement site (Figure 6-5, C). An 8-mm implant could be placed in this site; however, because this implant will be the posterior stop in a high occlusal force area, it was determined that a longer implant with a sinus graft was indicated here. It should be noted that on both the right and the left, the more anterior implant site showed adequate bone for fixtures of 4 mm in diameter and 13 mm or greater in length and no need for a sinus graft (Figure 6-5, D and E). Implants will be placed at the time of grafting, because adequate bone for initial stability (greater than 4 mm) is present in all sites planned for fixtures.
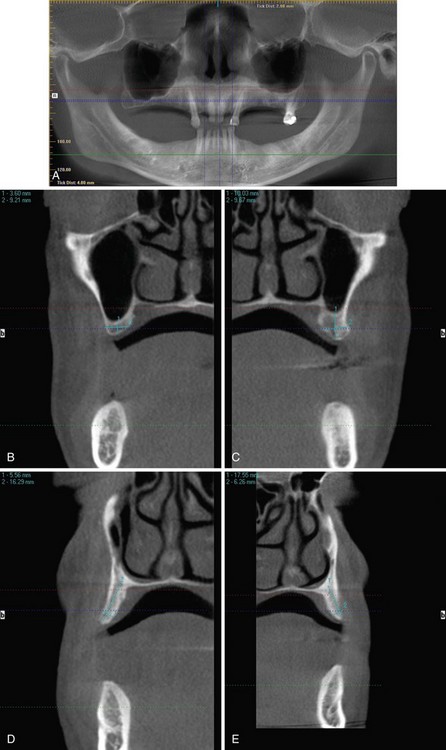
Figure 6-5 A, Panoramic CBCT showing proposed implant sites. Coronal CBCT cuts detailing area proposed for placement of the most posterior right maxillary implant (B) and the most posterior left maxillary implant (C). Coronal CBCT cuts detailing area proposed for placement of the more anterior right maxillary implant (D) and the more anterior left maxillary implant (E).
Treatment
There are four primary types of grafting material available for sinus augmentation:
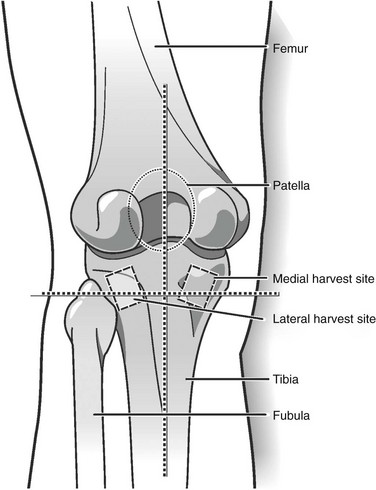
The technique of tibial bone harvest can be briefly discussed by pointing out that cancellous bone marrow of the tibial plateau can be approached by a medial or lateral route. Because the medial approach seems now to be the preferred method, this technique is discussed. The patient is placed in the supine position in the operating room or in the recumbent position in a dental chair if the procedure is performed in a clinic setting. A broad-spectrum antibiotic (generally a cephalosporin) is given as prophylaxis, and the surgical site is prepped and draped appropriately. The tibial tuberosity is located, and lines perpendicular and parallel to its long axis, intersecting at the center of the tuberosity, are scribed. A point 15 mm medial to the vertical line and 15 mm superior to the horizontal line is marked; this is the center of the incision. A 1- to 1.5-cm oblique incision is made over this point to the underlying bone (Figure 6-6). The periosteum is reflected, and a 1-cm circular osteotomy is prepared. The thin cortical window is removed, and cancellous bone is harvested with a curette. The upper boundary is 1 cm above the window to avoid the articular surface of the tibial plateau. Lateral and medial harvesting is done until the cortical bone is reached. Lower harvesting can proceed as far as the curette will reach. The wound is closed in layers, with attention paid to not tightly closing the periosteum. A pressure wrap is placed to complete the procedure. About 15 cc of noncompressed bone can be obtained in such a harvest. The strength of the tibia is unaffected by the surgery.
For the current patient, the immediate postoperative CBCT is shown in Figure 6-7, A. Subsequently, when the implants were uncovered and the healing caps placed (about 4 months after surgery), the sinus grafts demonstrated good consolidation (Figure 6-7, B). A CBCT cut from the area of the most posterior fixture on the right (Figure 6-7, C) further demonstrated graft remodeling and consolidation.
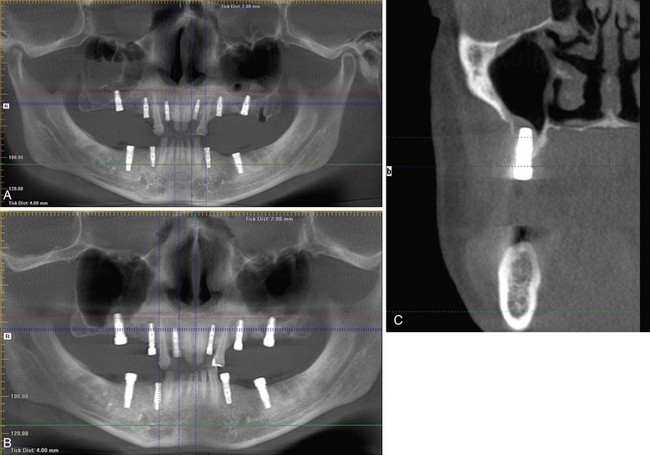
Figure 6-7 A, Panoramic CBCT immediately after grating and implant placement. B, Panoramic CBCT at implant exposure and placement of healing abutments (stage II). Note graft consolidation and return of aeration of maxillary sinuses. C, Coronal CBCT cut of most posterior implant site in the right maxilla, detailing graft consolidation.
Balaji, SM. Tobacco smoking and surgical healing of oral tissues: a review. Indian J Dent Res. 2008; 19:344–348.
Herford, AS, King, BJ, Audia, F, et al. Medial approach for tibial bone graft: anatomic study and clinical technique. J Oral Maxillofac Surg. 2003; 61:358–3563.
Jensen OT, ed. The sinus bone graft, ed 2, Chicago: Quintessence, 2006.
Jensen, T, Schou, S, Svendsen, PA, et al. Volumetric changes of the graft after maxillary sinus floor augmentation with Bio-Oss and autogenous bone in different ratios: a radiographic study in minipigs. Clin Oral Implants Res. 2012; 23:902–910.
Liddelow, G, Klineberg, I. Patient-related risk factors for implant therapy: a critique of pertinent literature. Aust Dent J. 2011; 56:417–426.
Lin, IC, Gonzalez, AM, Chang, HJ, et al. A 5-year follow-up of 80 implants in 44 patients placed immediately after the lateral trap-door window procedure to accomplish maxillary sinus elevation without bone grafting. Int J Oral Maxillofac Implants. 2011; 26:1079–1086.
Padmanabhan, TV, Gupta, RK. Comparison of crestal bone loss and implant stability among the implants placed with conventional procedure and using osteotome technique: a clinical study. J Oral Implantol. 2010; 36:475–483.
Renouard, F, Rangert, B. Risk factors in implant dentistry: simplified clinical analysis for predictable treatment, ed 2. Hanover Park, Ill: Quintessence; 2008.
Rodriguez-Argueta, OF, Figueiredo, R, Valmaseda-Castellon, E, et al. Postoperative complications in smoking patients treated with implants: a retrospective study. J Oral Maxillofac Surg. 2011; 69:2152–2157.
Singh, D, Teo, SG, Poh, KK. Regular narrow complex tachycardia. Singapore Med J. 2011; 52:146–149.
Testori, T, Weinstein, RL, Taschieri, S, et al. Risk factor analysis following maxillary sinus augmentation: a retrospective multicenter study. Int J Oral Maxillofac Implants. 2012; 27:1170–1176.
Triplett, RG, Nevins, M, Marx, RE, et al. Pivotal, randomized, parallel evaluation of recombinant human bone morphogenetic protein-2/absorbable collagen sponge and autogenous bone graft for maxillary sinus floor augmentation. J Oral Maxillofac Surg. 2009; 67:1947–1960.
Urban, IA, Nagursky, H, Church, C, et al. Incidence, diagnosis, and treatment of sinus graft infection after sinus floor elevation: a clinical study. Int J Oral Maxillofac Implants. 2012; 27:449–457.
Vittayakittipong, P, Nurit, W, Kirirat, P. Proximal tibial bone graft: the volume of cancellous bone and strength of decancellated tibias by the medial approach. Int J Oral Maxillofac Surg. 2012; 41:531–536.
Wallace, SS, Tarnow, DP, Froum, SJ, et al. Maxillary sinus elevation by lateral window approach: evolution of technology and technique. J Evid Based Dent Pract. 2012; 12(3 Suppl):161–171.
Wong, J, Lam, DP, Abrishami, A, et al. Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Can J Anaesth. 2012; 59:268–279.
Woo, EJ. Adverse events reported after the use of recombinant human bone morphogenetic protein 2. J Oral Maxillofac Surg. 2012; 70:765–767.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses