Periodontal and Periimplant Surgical Anatomy
A sound knowledge of the anatomy of the periodontium and the surrounding hard and soft structures is essential to determine the scope and possibilities of periodontal and implant surgical procedures and to minimize their risks. The spatial relationship of bones, muscles, blood vessels, and nerves as well as the anatomic spaces located in the vicinity of the periodontal or implant surgical field are particularly important. Only those features of periodontal and implant surgery relevance are mentioned in this chapter; the reader is referred to books about oral anatomy for a more comprehensive description of these structures.4,6
Mandible
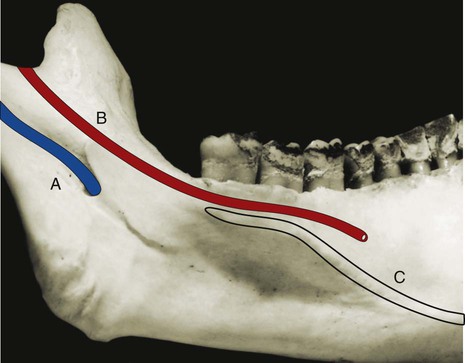
The mandibular canal, which is occupied by the inferior alveolar nerve and vessels, begins at the mandibular foramen on the medial surface of the mandibular ramus and curves downward and forward until it becomes horizontal below the apices of the molars (Figure 54-1). The distance from the canal to the apices of the molars is shorter in the third molar area and increases as it goes forward. A small percentage (1%) of mandibular canals bifurcate in the body of the mandible, thereby resulting in two canals and two mental foramen.5,10 In the premolar area, the mandibular canal divides in two branches, with one exiting the mandible and the other continuing anteriorly: the incisive canal, which continues horizontally to the midline, and the mental canal, which turns upward and opens in the mental foramen.
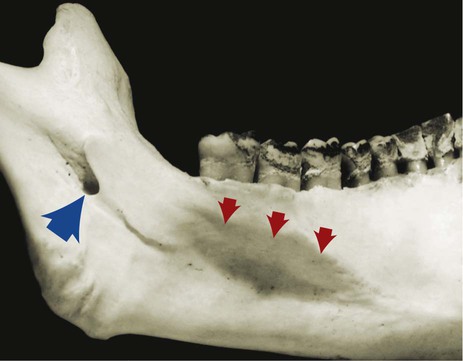
The mental foramen, from which the mental nerve and vessels emerge, is located on the buccal surface of the mandible below the apices of the premolars, sometimes closer to the second premolar and usually halfway between the lower border of the mandible and the alveolar margin (Figure 54-2). It is often but not always visible on conventional radiographs. The opening of the mental foramen, which may be oval or round in shape, typically faces upward and distally, with its posterosuperior border slanting gradually to the bone surface. An “anterior loop” of the mental foramen has been described, with the use of cadaver dissection, as a reverse turn and looping back of the mental nerve before its exit out of the mental foramen; its length ranges from 0.5 to 5.0 mm.10 More recent evaluation of the anterior loop of the mental nerve involving the use of cone beam scans and cadaveric dissection reported this loop extension to range from 0.0 to 9.0 mm.22,23 The anterior loop of the mental nerve has a high prevalence (88%), symmetric occurrence, and a mean length of 4.13 ± 1.08 mm.18 As it emerges, the mental nerve divides into three branches. One branch of the nerve turns forward and downward to supply the skin of the chin. The other two branches course anteriorly and upward to supply the skin and mucous membrane of the lower lip and the mucosa of the labial alveolar surface.
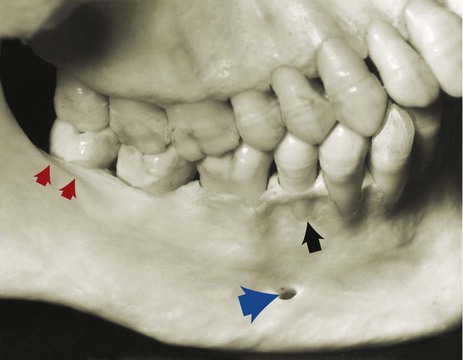
Surgical trauma (e.g., pressure, manipulation, postsurgical swelling) to the mental nerve can produce paresthesia of the lip, which recovers slowly. Partial or complete cutting of the nerve can result in permanent paresthesia, dysesthesia, or both. Familiarity with the location and appearance of the mental nerve reduces the likelihood of injury (Figure 54-3).
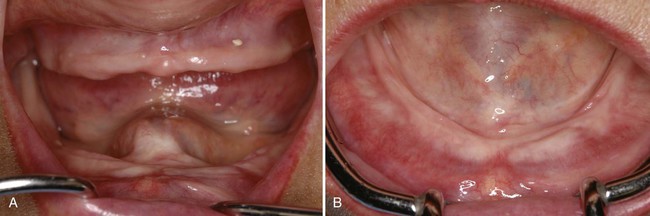
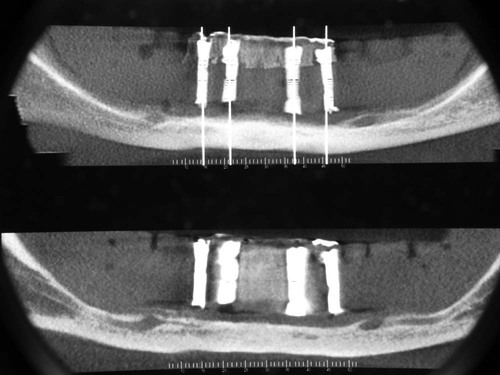
In partially or totally edentulous jaws, the disappearance of the alveolar portion of the mandible brings the mandibular canal and mental foramen closer to the superior border (Figures 54-4 and 54-5). When these patients are evaluated for the placement of implants, the distance between the canal and the superior surface of the bone as well as the location of the mental foramen must be carefully determined to avoid surgical injury to the nerve (see Chapter 73).
The anterior extension of the inferior alveolar nerve or incisive nerve has been measured with the use of conventional radiographs, computed tomography (CT) scans, cadaver dissections, and cone beam scans.3,10,22,23 This nerve, which is less evident on conventional radiographs and often unnoticed, extends beyond the anterior loop of the mental foramen in a horizontal direction toward the midline. The length of the incisive canal has been reported to be up to 21.45 mm from the mesial aspect of the mental foramen and to terminate just 4 mm from the midline.3
The lingual nerve, along with the inferior alveolar nerve, is a branch of the posterior division of the mandibular nerve. It descends along the mandibular ramus medial to and in front of the inferior alveolar nerve. The lingual nerve lies close to the surface of the oral mucosa in the third molar area and goes deeper as it travels forward (Figure 54-6). It can be damaged during anesthetic injections and during oral surgery procedures (e.g., third molar extractions).14 Less often, the lingual nerve may be injured when a periodontal partial-thickness flap is raised in the third molar region or when releasing incisions are made in the area.

The alveolar process, which provides the supporting bone to the teeth, has a narrower distal curvature than the body of the mandible (Figure 54-7), thus creating a flat surface in the posterior area between the teeth and the anterior border of the ramus. This results in the formation of the external oblique ridge, which runs downward and forward to the region of the second or first molar (Figure 54-8) to create a shelflike bony area. Resective osseous therapy may be difficult or impossible in this area because of the amount of bone that must be removed distally toward the ramus to achieve resection of a periodontal osseous defect on the distal aspect of the mandibular second or third molar.
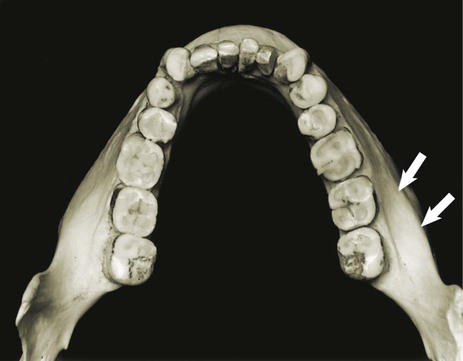

Distal to the third molar, the external oblique ridge circumscribes the retromolar triangle (see Figure 54-8). This region is occupied by glandular and adipose tissue and covered by unattached, nonkeratinized mucosa. If sufficient space exists distal to the last molar, a band of attached gingiva may be present; only in such a case can a distal flap procedure be performed effectively.
The medial side of the body of the mandible is traversed obliquely by the mylohyoid ridge, which starts close to the alveolar margin in the third molar area and continues anteriorly in an apical direction, thereby increasing its distance from the osseous margin as it travels forward (Figure 54-9). The mylohyoid muscle inserts along this ridge and separates the sublingual space, which is located above or more anteriorly and superiorly, from the submandibular space, which is located below or more posteriorly and inferiorly.
Maxilla
• The alveolar process contains the sockets for and supports the maxillary teeth.
• The palatine process extends horizontally from the alveolar process to meet its counterpart from the opposite maxilla at the midline intermaxillary suture, and it extends posteriorly with the horizontal plate of the palatine bone to form the hard palate.
• The zygomatic process extends laterally from the area above the first molar and determines the depth of the vestibular fornix on the lateral aspect of the maxilla.
• The frontal process extends in an ascending direction and articulates with the frontal bone at the frontomaxillary suture.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses