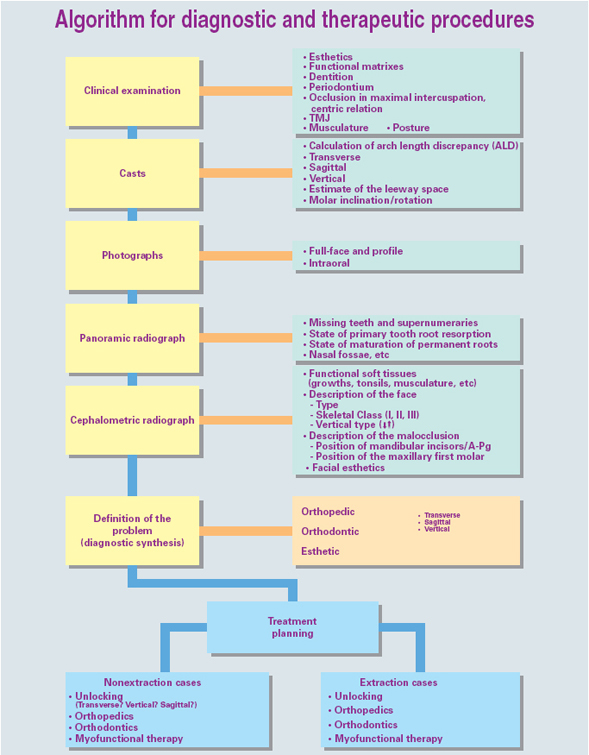
Choosing an appliance to treat the patient is nothing more than the final step in a complete diagnostic process that flows from the clinical examination to the study of the casts, photographs, and the cephalometric radiograph. The complete procedure for arriving at this important decision is summarized in Fig 5-1.
The construction and activation of the different appliances described in this chapter are discussed more fully in chapter 6.
The term unlocking refers to the elimination of all impediments or constraints, both mechanical and functional, on the maxilla or on the mandible.
The objectives of removing impediments are:
1. To free the mandible from all occlusal obstacles by “recontouring” the maxilla, which is the guiding arch. This is accomplished through rotation of the molars and expansion of the maxilla both anteriorly and posteriorly.
2. To neutralize any flawed operation of the functional matrixes such as mouth breathing, abnormal swallowing, muscular imbalance, or faulty posture.
3. To free the temporomandibular joint (TMJ) from any compressive restraints so that the full potential for growth of the condylar region can be achieved.
4. To liberate sufficient space in which the tongue can move to the fullest extent and be retrained as effectively as possible.
5. To restore the normal intercanine dimension by expanding the premaxilla, a maneuver that will have positive repercussions in clearing the nasal passages and on the functioning of the facial envelope (Talmant et al 1982).
Principles of unlocking
1. Preparing a diagnosis and beginning treatment when the child is still young
2. Normalizing functions
3. Treating transverse and vertical problems first
4. Placing teeth in a neutral zone
5. Ensuring that the condyles are positioned correctly in the glenoid fossae and aiding the joint to function properly
6. Establishing correct occlusal function
7. Employing a comprehensive medical point of view
Class I Discrepancies and Anomalies Common to All Classes of Malocclusion
Included in this discussion are the malformations that occur in the so-called normal Class I category that can appear as vertical disorders, such as short- or long-face syndrome, and in the transverse plane, as a lack of harmony between basal bone and tooth size.
Anomalies of number and position
Ageneses
Ageneses rarely occur in the primary dentition. When they do occur, ageneses usually affect the maxillary incisor region and, next most frequently, the mandibular incisor region. If primary teeth are missing, their permanent successors usually are also.
Supernumerary teeth
Supernumerary teeth occur only rarely in the primary dentition and, when they do, there is no need to extract them.
In the mixed dentition, they are usually found in the incisor region, causing a midline deviation. The orthodontist should plan to have these supernumerary teeth extracted as soon as possible.
Impacted teeth
Impacted teeth are extremely rare in the primary dentition. In the mixed dentition, a supernumerary tooth can cause a permanent incisor to be impacted. The orthodontist makes the diagnosis radiographically. The initial treatment consists of extracting the supernumerary tooth, but often the impacted tooth must be guided into the arch orthodontically.
Ankyloses of primary teeth
Primary molars can be considered to be ankylotic when they drop out of occlusion by distances that vary from less than 1 mm to a few millimeters or even to the extent of becoming covered by bone. When primary roots become ankylosed, the associated permanent teeth may cease to erupt and, in effect, become ankylosed themselves, or, by assuming faulty positions, become ectopic. The maxillary second molars are the most frequently affected primary teeth, followed by the primary mandibular second molars, the primary maxillary first molars, and the primary mandibular first molars. Again, the final diagnosis is made radiographically. Treatment is surgical removal, which may be difficult if the roots are too stubbornly affixed to the bone.
Ectopic eruptions in the mixed dentition
A tooth is said to have erupted ectopically when it emerges into an abnormal position. Ectopic eruption may result from a traumatic event to the primary dentition that caused premature loss of a primary incisor with loss of arch space; transmission of the force of the blow to the corresponding permanent tooth bud; or posttraumatic necrosis of the pulp of the affected tooth, which slows down its root resorption, leading to overretention that may deflect the eruption of its permanent successor.
These traumatic events can also provoke lesions in unerupted permanent teeth, such as enamel dysplasia if the event occurs when the child is around 1 year old, or deformation or curvature of the crown or root of the unerupted tooth if the event occurs when the child is 3 to 4 years old.
An odontoma can deflect the path of eruption of a tooth. The defective orientation may cause a root deformation if the root comes in contact with the hard cortical bone of the palatal vault, the midline suture, or the maxillary sinus. Treatment consists of maintaining space left by a lost tooth; extracting a devitalized tooth to allow eruption of its permanent successor; or eliminating the obstruction of an odontoma by extracting it.
Crowding
When the primary teeth are crowded, it is almost certain that the permanent teeth will also be crowded. Crowding in the mixed dentition can be classified as primary or secondary. Primary crowding, which is hereditary, derives from an arch length discrepancy (ALD).
Primary crowding
When the actual arch length is greater or less than the sum of the mesiodistal diameters of all the permanent teeth, an ALD exists. If there is insufficient room, a relative macrodontia can be said to exist; if spaces, or diastemata, are present, the condition can be described as relative microdontia.
Early diagnosis. In the primary dentition, there is no correlation between size of primary teeth and the size of their permanent successors; nevertheless, it is usually true that the permanent teeth will be less likely to erupt in good alignment if the mixed dentition has no interdental spacing than if diastemata had been present.
Following are some of the warning signs that can be observed in the primary dentition:
1. Bimaxillary protrusion: protrusion of both dental arches with no crowding.
2. Crowding of the incisors: Often the mandibular incisors will be positioned lingually. The maxillary incisors may be placed too far labially as a result of mesial drift of the permanent canines.
3. Small primary canines and molars.
4. Premature loss of a primary canine whose root has been resorbed by crowded erupting incisors. The mandibular midline will deviate in the direction of the lost tooth.
5. Premature loss of both primary canines: The mandibular incisors will then be excessively vertical with an accompanying increase in overjet and/or crowding.
6. Gingival recession affecting the most labially placed mandibular incisor.
7. Pronounced maxillary or mandibular bulge of the erupting canines because of crowding of the buccal segments.
8. Ectopic eruption of the permanent first molars in overly mesial positions and loss of the primary second molars, indicating insufficient development in the tuberosity regions.
9. Disharmony in tooth size (Bolton).
10. Radiographic signs on the cephalometric radiograph: diminished maxillary arch length; mandibular canine buds in the symphysis area; and labial positioning of the incisors.
11. Radiographic signs on the panoramic radiograph: resorption of the roots of many primary teeth associated with the eruption of a single permanent tooth; Quintero’s sign (fanning out of the incisors); mesial positioning of the maxillary canine buds; superimpositioning of proximal surfaces of teeth; impaction or atypical positioning of canines or premolars; resorption of the roots of the primary second molars by the erupting permanent molars; vertical alignment of the buds of the maxillary molars; exaggerated curve of Spee; and mesiodistal diameter of unerupted premolars that is equal to or greater than that of primary molars.
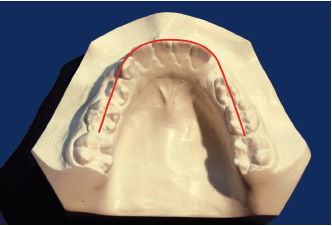
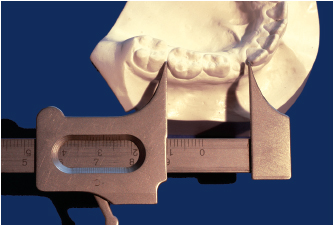
After having assessed the clinical and radiographic signs, the orthodontist can make the diagnosis by measuring the study casts to calculate whatever lack or excess of space may exist for the correct placement of the permanent teeth as they emerge into the arch. Two parameters must be determined: a measurement of the available space by Nance’s method (Fig 5-2) and a measurement of the needed space (Fig 5-3).
To calculate the ALD, which can be positive or negative, the orthodontist finds the difference between the future required length and the present length.
The orthodontist should consider the transitory disharmony, which is the chronologic gap between the patient’s “bone age” and “dental age,” when formulating the differential diagnoses. Premature eruption of permanent teeth accompanying incipient crowding can be a signal of such a gap, but the problem may disappear if the patient goes through a sufficiently generous growth spurt. In the differential diagnoses, the orthodontist should also consider anteriorly positioned molars, anomalies in the path of jaw closure, and alveolar and incisal protrusion.
Treatment of slight or transitory ALD of up to 4 mm with crowding. The orthodontist should vigilantly protect available arch length, using every preventive means at his or her disposal, such as seeing that caries lesions are restored promptly and broken-down molars are restored.
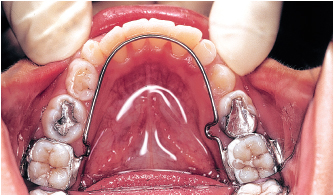
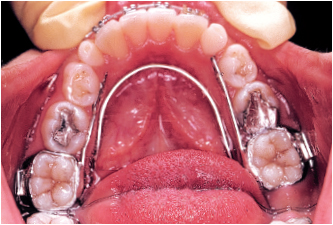
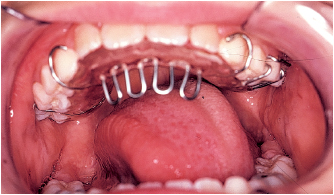
Extractions are contraindicated. The leeway space of about 4 mm, which is present before the primary second molars are shed, can be utilized to correct mild anterior crowding. The orthodontist can use a passive lingual arch contacting the lingual surfaces of the anterior teeth to preserve space and, when indicated, can reduce incisal width with interproximal stripping (Figs 5-4 and 5-5).
When this course is adopted, the orthodontist must know the precise location of the terminal plane. In the case of a flush terminal plane, if a lingual arch is being used to keep the permanent mandibular first molars in place, preventing them from moving forward in the normal physiologic drift, the gain of approximately 4 mm in arch length will provide sufficient space for proper eruption of the incisors and canines. Following this, when necessary, the orthodontist can move the permanent maxillary first molars distally to obtain a Class I molar relationship.
If the terminal plane has a distal step, maintaining the permanent mandibular first molars signifies that the permanent maxillary first molars will be in a Class II relationship. The same procedures utilized in the preceding situation should be carried out in this case, provided that there is sufficient room for distalizing the maxillary molars, whose position with regard to the pterygoid plate must be assessed.
If the terminal plane has a mesial step, the maxillary 6-year molars will erupt into a Class I relationship.
Treatment of ALD of 4 to 7 mm. When assessing patients in this category, the orthodontist must consider the possibility of extracting teeth; however, before making this decision, the clinician must carry out a careful clinical examination, giving particular attention to the functional matrix.
An analysis of the lateral cephalogram must be performed to evaluate the facial type. It is also important to determine the position of the mandibular incisors with respect to point A–pogonion, the normal value of which is 1 mm. In brachyfacial types, this measurement can be as high as 3 to 4 mm. The position of the maxillary molars in relation to the vertical pterygoid plane has a normal value (in millimeters) of the patient’s age plus 3 ± 2 mm. When this value is high, it may be possible to distalize the maxillary molars (see Fig 4-24).
An evaluation of the study casts must be undertaken to determine whether it would be possible to expand the arches enough to acquire the needed arch length and to distalize the molars.
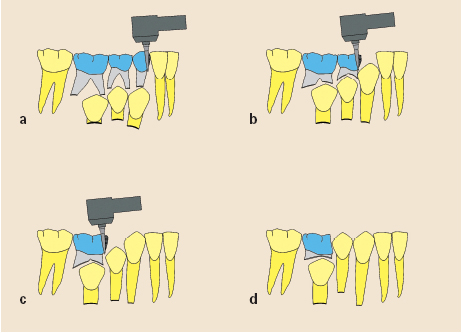
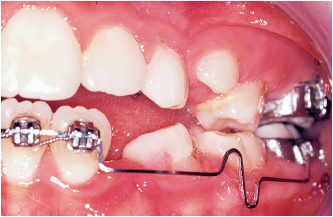
Space can be gained, or recovered, by a variety of methods. Among these are orthodontic mechanics. In the maxillary arch, space can be increased with a quadhelix (Fig 5-6), a Crozat quadhelix (Fig 5-7), or a removable expansion appliance (see chapter 6). The mandibular arch can be expanded with a bihelix (see Fig 5-6c), a Crozat bihelix if it is necessary to advance the incisors (Fig 5-8), or a utility arch for advancing the incisors (Fig 5-9).
Space can also be increased through use of a functional appliance. A Fränkel appliance (Fig 5-10; see also Fig 5-33b), thanks to its screening plates, fends off the centripetal intruding forces exerted by the lips and the cheeks, thus giving the tongue a clear field to freely exert its expansive muscular force. In its physiologic operations, the tongue will naturally create 4 to 5 mm of mandibular arch length.
Orthopedic mechanics can be applied in the form of a rapid palatal expansion appliance (see chapter 6). This device can expand the maxillary arch by as much as 11 mm as its screw is turned daily toward the posterior. Alternatively, a quadhelix with built-in buccal root torque, a device that is useful for expanding the palates of very young children, can be used.
Treatment of crowding and ALD exceeding 7 mm. If, after having evaluated every possible technique for acquiring the space needed for aligning the crowded teeth, the orthodontist determines that a malocclusion cannot be corrected without the removal of permanent teeth, there are two options: First, the orthodontist can refrain from beginning treatment in the mixed dentition with the expectation that teeth in the permanent dentition will be extracted. If this decision is made, it is critical to avoid any temptation to create space by expansion. However, when anterior or buccal crossbites or any other interference is present, this problem should be corrected promptly, even if extractions in the permanent dentition will be required.
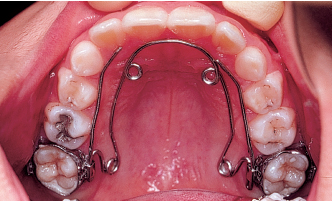
Fig 5-6b A quadhelix is used to reshape the maxillary arch.
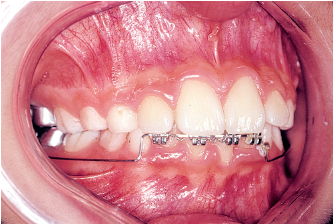
Fig 5-6d A utility arch is used to align the mandibular incisors. After this is accomplished, a fixed mandibular lingual arch serves as a retainer. This child did not have to have any permanent teeth extracted. The earlier treatment is accomplished, the more stable will be the alveolar, dental, periodontal, and neuromuscular changes achieved.
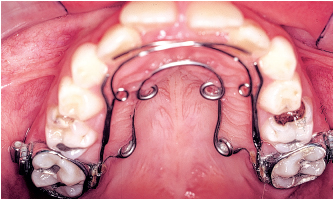
Fig 5-7b A Crozat quadhelix with springs against the lateral incisors is used to move them into position.
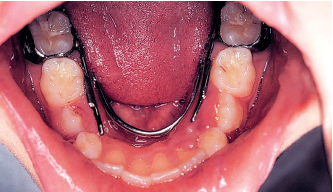
Fig 5-8b The result after the mandibular arch has been reshaped.
1. Removal of a primary tooth whose root has scarcely begun to resorb will delay the eruption of its successor.
2. Removal of a primary tooth more than half of whose root has been resorbed will hasten eruption of its successor; the objective is to encourage eruption of the first premolars (for their expeditious removal) before the canines erupt.
The most frequently utilized plan for serial extraction is: primary canine, primary first molar, permanent first premolar. Orthodontic treatment to optimize tooth positioning and occlusion should begin after the permanent dentition is fully in place. The orthodontist should be sure primary left and right canines are extracted at the same time to avoid the development of a midline deviation.
Serial extractions are indicated for a limited number of situations:
1. For a skeletal Class I relationship with significant crowding
2. For a mixed dentition with a terminal plane that ends in a mesial step
3. For slight overjet and crowding
4. For mesofacial and dolichofacial types
5. For children about 8 years old
The approach would be inappropriate or contraindicated in many instances:
1. For a skeletal Class II relationship
2. For a skeletal Class III relationship
3. For brachyfacial types
4. For slight or transitory arch length discrepancy
5. For congenitally missing teeth
6. For convex facial type; bimaxillary retrusion
7. For bialveolar protrusion cases that will require impeccable anchorage
8. For lingually inclined mandibular incisors
9. For deep overbite
10. For reduced intercanine distance
11. For children with psychological difficulties such as excessive fear of extractions
If the practitioner has any doubts, the decision to extract should be deferred, because this step is irreversible.
In patients with excess arch length, the orthodontist should delay treatment until the adult dentition is in place.
The following procedures are available for increasing arch length:
1. Advancement of point A with facial mask or Class III elastics
2. Maintenance of the leeway space, which is approximately 2 mm on each side
3. Correction of rotated maxillary first molars, which should gain approximately 1 mm on each side
4. Expansion in the canine and molar regions in accordance with the limits presented in chapter 4 (“Examination of Casts”)
5. Advancement of mandibular incisors, 1 mm of incisor advancement yielding 2 mm of arch length
6. Interproximal stripping
7. Premolar extractions, which should be done only in the permanent dentition and only when clearly required, providing about 7 mm of space per tooth
Secondary crowding
Secondary crowding is functional in origin and occurs when there has been a reduction in arch length, mandibular incisors are lingually inclined, or primary teeth have been shed in atypical order.
Reduction in arch length (perimeter). This can result from interproximal dental caries in primary teeth or the premature loss of a primary second molar with a resultant crowding in the buccal segment. In these ways, the space that primary molars should have preserved by their very presence may be encroached upon. Whenever it finds a mesial space to occupy, an erupting permanent first molar will tend to move into that space.
Immediately after premature extraction of a primary second molar, if the permanent first molar is already present, the orthodontist must be sure that the space is preserved with one of the following devices, which are described in detail in chapter 6: a unilateral space maintainer whose mesial extensions abut the distal surface of the primary first molar, a bilateral space maintainer from permanent molar to permanent molar contacting the lingual surfaces of the incisors, or a Nance palatal arch for maintaining space in the maxillary arch.
If the space maintainers have not been placed in a timely fashion, and the permanent molars have begun to move mesially, the orthodontist must recover the lost space with an appropriate appliance to ensure that space is available for eruption of the second premolars.
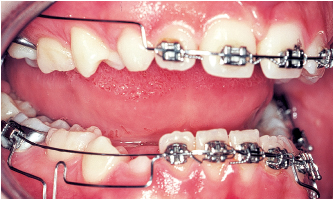
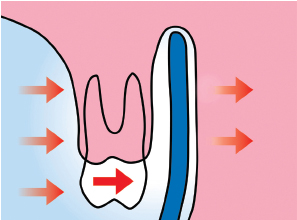
To regain space in the mandibular arch, the orthodontist can use a lip bumper (Fig 5-11). Lip pressure on the appliance will transmit force to the molars, moving them distally while at the same time cutting off unwanted centripetal pressure on the incisors (see chapter 6). A removable appliance with a screw or spring can be used to distalize molars (see chapter 6). A utility arch works effectively when the orthodontist not only needs to recapture lost space but also has to intrude the mandibular incisors or move them labially.
In the maxillary arch, space can be gained with a transpalatal bar that can either be soldered to the molar bands or inserted into lingual tubes on them. When the bar is activated, it distalizes those molars (see chapter 6). A removable appliance with distalizing springs or screws can also be used (see chapter 6). Extraoral force remains a useful technique for distalizing molars but requires good cooperation from the young patient, among other inconveniences.
A quadhelix can be used if expansion is also indicated. When activated correctly, this device not only expands but also moves molars distally (see chapter 6).
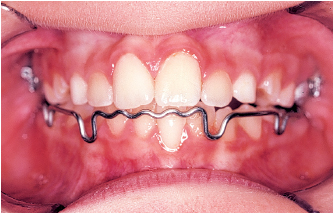
Fig 5-11b The maxillary arch is expanded with a quadhelix and the mandibular arch is expanded with a Korn lip bumper. The lip bumper keeps the lips from exerting compressing, centripetal forces against the teeth, freeing the muscles of the tongue to effect a passive expansion of the mandibular arch.
Lingually inclined mandibular incisors. This condition usually results from functional causes, such as thumb, finger, or lower lip sucking or habitually holding the tongue crooked over the mandibular incisors. A lip bumper works effectively to discourage these habits and to prevent muscle pressure from lips and cheeks from working against the teeth. A Crozat appliance can be added to the setup to add lingual pressure against the mandibular incisors.
If the tongue is habitually held in a faulty position, two devices can be useful. Bonnet’s lingual night envelope encourages the tongue to assume a normal posture by guiding it against the retroincisive papillae. Alternatively, Fränkel’s functional regulator is also effective.
Faulty sequence of exfoliation of the primary teeth. When this happens, a midline deviation can result. If not accompanied by a similar shift of the frenum, the deviation becomes a dental problem like the one caused by the loss of a single primary canine. The first step in correcting a midline deviation caused by a premature loss of a primary canine is extraction of the contralateral primary canine. This course of action could diminish arch length and worsen overbite. In cases where future extractions of first premolar teeth are likely, the orthodontist may wish to consolidate the situation with a mandibular lingual arch contacting the lingual surfaces of the incisors (see the discussion of serial extractions earlier in the chapter). If extractions are not envisioned, the orthodontist should recapture lost space with a utility arch activated unilaterally (Fig 5-12).
Diastemata
When diastemata are present in the primary dentition, they indicate that the risk of crowding in the permanent dentition is 50% if they are 3 mm or less, 20% if they are 3 to 6 mm, and very slight if they are greater than 6 mm.
Because diastemata occur so rarely in the mixed dentition, the orthodontist should diligently search for the cause of any diastemata observed.

Fig 5-12c Space has been regained for eruption of the permanent mandibular left canine, and the midline has been corrected.
Localized diastemata
The causes of diastemata include missing teeth as well as impediments to the eruption of a permanent tooth, such as odontomas, especially in the maxillary incisor area. Periapical and panoramic radiographs are essential for proper diagnosis. In addition, lip or finger sucking can cause the maxillary anterior teeth to protrude and become spaced. The effects of these habits on the soft and hard tissues of the oral cavity vary with the frequency, duration, and intensity of the behavior (for suggested treatment, see the section, “Maxillary [alveolar] protrusion with diastemata”). Lingual frena or maxillomandibular sutures are responsible for the midline diastemata that usually disappear when the lateral incisors and canines erupt. If they persist, the frenum is hypertrophied.
In the clinical examination, the orthodontist should check to see if lateral incisors are congenitally absent or the maxillary frenum is hypertrophied. With this clinical and radiographic information, the orthodontist can make the diagnosis. If the frenum lying in a normal V-shaped septum divides it in two, the orthodontist should see that this hypertrophied tissue is removed surgically and then close the space orthodontically.
The causes of generalized diastemata include a positive malrelation between teeth and supporting bone due to microdontia (ie, teeth are too small to fill the available space) and open bite and spacing between the teeth caused by abnormal behavior of the tongue (ie, thrusting; see Fig 4-5). Treatment usually consists of tongue retraining with or without the use of a lingual night envelope. When a short, tight frenum that constricts the tongue in a low posture is present, surgery followed by retraining exercises may be advisable.
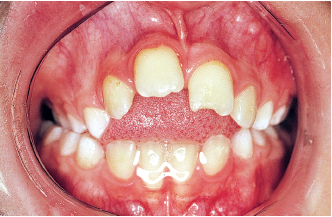
Maxillary (alveolar) protrusion with diastemata
“Deforming” habits usually cause this condition. When objects are sucked forcibly, they may cause the maxillary teeth and supporting tissues to protrude, force the mandibular teeth and supporting structures lingually, and, in some cases, lead to an open bite.
The first steps should be thoughtfully psychological, rather than punitive, in character; screens, spikes, and thumb restraints should be avoided so that the treatment does not add to the emotional stress that seems to be such a frequent complication of family life. Other somewhat more aggressive techniques, such as a bandage on the thumb or a soft glove sewn to a pajama sleeve, may be helpful in some patients without doing too much emotional damage, but the orthodontist will always be well advised in persuading young patients that cessation of the habit is in their own best interests.
Only when all else has failed should the orthodontist resort to coercive habit-breaking methods. In some cases, with highly recalcitrant children, the orthodontist may wish to enlist the assistance of a professional psychologist.
In the primary dentition, when children are very young, Hinz’s buccal shields may be indicated for improving muscle tone of the lips and to prevent children from forcing their lips over their mandibular incisors and against the lingual surfaces of the maxillary anterior teeth. The buccal screen is interposed between the teeth and the lips as shown in Fig 5-13.
A quadhelix with lingual spurs attached to the primary maxillary second molars can be placed to make it difficult for children to suck their fingers.
In the mixed dentition, a variety of appliances can be used: a removable plate with a grill (Fig 5-14), a quadhelix to rotate molars and widen a V-shaped palate, and a quadhelix with a grill (Fig 5-15). A contracting utility arch can be used to retract protruded incisors (Fig 5-16).
When children swallow atypically, the orthodontist should employ myofunctional therapy as a supplement to orthodontic treatment.
Open bites or retruded mandibular incisors
These conditions result from a lack of vertical development of the anterior alveolar processes. By examining the study casts in occlusion, the orthodontist can note the incisor infraocclusion. By examining the casts separately, the practitioner can localize the root of the problem. The malocclusion can be functional or skeletal in origin.
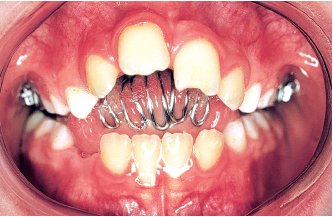
Fig 5-15b A quadhelix with spurs is the only appliance used.

Fig 5-15c The open bite and the crossbite have been corrected and the patient has received myofunctional therapy. The chief advantage of this device is that the child cannot remove it. Its principal disadvantage is that the forces it develops are transmitted solely to the banded teeth that support the appliance and may, therefore, tilt the teeth unfavorably.

Fig 5-16b A contracting utility arch was used to retract and depress the incisors.

Fig 5-16c Final result.
Functional open bite
Open bites usually result from disturbances in the functional matrix triggered by harmful habits such as mouth breathing, low tongue posture, abnormal swallowing, and sucking on a finger, pacifier, or bottl/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses