Case history
The orthodontist should begin taking a case history to find the reasons—cosmetic, functional, emotional, or other—that impelled the patient and the parents to seek an orthodontic consultation. The case history should also include general medical as well relevant dental information.
Functional matrix
The orthodontist should begin the clinical examinations by surveying the patient’s general appearance and the status of the patient’s functional matrix.
Breathing apparatus
Upper airways
Examination of the upper airway consists of determining whether the patient is breathing primarily through the mouth, the nose, or both and noting whether the adenoidal and tonsillar tissues are enlarged and inflamed, whether there is a nasal septal deviation, whether the nasal openings are narrowed, and whether there is any other obstructive or allergic problem (Figs 4-1 and 4-2).
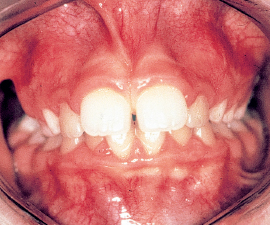
Intraoral examination
In this inspection, the orthodontist looks for the presence of maxillary, mandibular, or functional anomalies. The patient may have an underdeveloped maxilla, a V-shaped maxilla, a retruded mandible, an excessively low position of the tongue, atypical swallowing, or partial or more generalized discrepancies in occlusion (see chapter 3 on the functional matrix).
Tests for revealing pathologic mouth breathing
To discern improper mouth breathing, the orthodontist can use the Rosenthal test: While the child is taking 10 to 15 deep breaths with his or her mouth closed, inhaling and exhaling through the nose, the practitioner measures the patient’s pulse rate. Children who are normal nasal breathers have no difficulty in complying and show no rise in pulse rate. This reaction is considered a negative test for mouth breathing. The mirror test (Fig 4-3) and the nares reflex (Fig 4-4) are also useful for revealing mouth breathing.
Signs of allergy
For the sake of completeness, the orthodontist should refer patients to pediatricians or allergists for allergy tests.
Tongue and deglutition
The orthodontist must evaluate:
1. The position of the tongue at rest and as it functions in swallowing. Does it take a high, middle, or low position?
2. The volume and the mass of the tongue. Are they normal or could the state of the tongue be described as microglossia or macroglossia? Can imprints of the teeth be seen on the tongue’s surface? This would indicate that the tongue is thrust between the teeth during swallowing.
3. The length of the frenum. Is it normal or is it short? The length will suggest the influence it exerts on the mobility of the tongue; a short frenum restricts tongue protraction (Fig 4-5).

Fig 4-5b The consequence of the short frenum will be a low positioning of the tongue, which leads to generalized diastemata.
The orthodontist should examine both upper and lower lips (Figs 4-6 to 4-8), the labiomental groove (Fig 4-9), and the buccinator muscle (Fig 4-10).

Fig 4-7a Evaluating the shape and the esthetic quality of the lips. The closure line should be located 2 mm above the incisal edge of the maxillary anterior teeth.

Fig 4-7b Evaluating the behavior of the lips as they function in swallowing. Contraction of the perioral musculature indicates atypical swallowing.
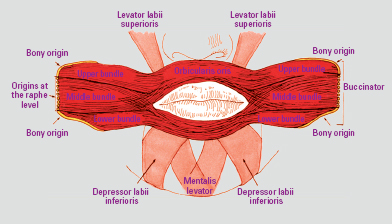
Fig 4-10b A hypertonic buccinator muscle pulls on the orbicular muscles of the lips through their anatomic connections, creating problems for the incisor and canine teeth. (Illustration by S. Frederick.)

Fig 4-10c Enlarged view showing the effect the orbicularis oris muscle has had on the dentoalveolar process. In such cases, any expansion or buccal movement of teeth should be undertaken with extreme caution because of the likelihood of relapse.
Temporomandibular joint (TMJ) and muscles of mastication
Children are not spared from postural craniomandibular dysfunction (PCMD).
More than 30% of children show signs and symptoms of PCMD: clicking of the joint, deviations in opening, articular or muscular pain, headaches, and so on. This is why orthodontists should routinely examine the functioning of patients’ muscles and the TMJ, which should be palpated at rest and in movement (Fig 4-11).
A dynamic examination of the TMJ is made with the patient’s teeth apart so that no dental interference can occur. The primary goal at this stage of the examination is to assess the functional capabilities, the limits, and the deviations or deflections, if any, of the TMJ (Fig 4-12).
If clicking is noted, the orthodontist should determine at what point in the trajectory of mandibular movement it occurs, in opening or in closing. Clicking usually denotes some disruption in condyle-disc coordination. Clicking amounts to an early, intermediate, or late mini-subluxation (Figs 4-13 and 4-14).
After palpating the muscles of mastication, the orthodontist should note any disturbances or pain reported by the patient, using a scale of 1 (least) to 3 (greatest) (Fig 4-15).
Dentition
The orthodontist should conduct the clinical examinations in all three planes of space. In the sagittal plane, the assessment should include:
1. The relationships between the molars and canines, on the right and left sides
2. The nature of the terminal plane formed by the primary second molars: flush, mesial step, or distal step
3. The presence or absence of diastemata
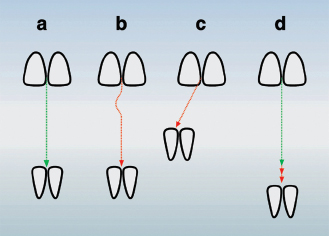
4. The presence or absence of anterior crossbite
5. The presence or absence of overjet
In the transverse plane, the orthodontist should look for:
1. Unilateral or bilateral posterior crossbites
2. Midline deviations or problems with frena
In the vertical plane, the examination should evaluate:
1. The interincisal relationships
2. The presence or absence of closed bite or overbite
Other evaluations
Esthetics of the dentition and the smile
Esthetics is evaluated only in the mixed and permanent dentitions, not in the primary dentition. The orthodontist should assess the relationship between the incisal edges of the maxillary anterior teeth and the upper lip, the smile line, and the extent of the exposed gingiva to see if the patient has a “gummy” smile.
Symmetry between the frena and the face
The median labial frena, maxillary and mandibular,/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses