Chapter 5
Treatment of a Patient with a Partially Edentulous Mandible Using Intraoral Scanning (IOS) of a CADCAM Healing Abutment
LITERATURE REVIEW
Endosseous implants have become an integral part of prosthodontic treatment for edentulous and partially edentulous patients. This has come about for multiple reasons: among them, excellent long-term success rates published in multiple refereed journals around the world, improvements in implant and restorative component designs and machining, and decreased surgical morbidity and increased consumer demand for noninvasive tooth replacements (O’Neal & Butler 2000).
Dental implants were originally developed to restore compromised edentulous patients to normal function (Branemark et al. 1985). Aesthetics and phonetics were of lesser importance. Implant restorations are now expected to predictably restore function, aesthetics, and phonetics. In edentulous patients, dental implants were originally placed into sites where there was adequate bone for implants. Precise implant placement relative to tooth positions was not required because implants could be placed between artificial teeth of the implant prosthesis without aesthetic compromise (Figures 5.1 and 5.2). Implants placed into embrasure spaces in partially edentulous patients may result in aesthetic and/or phonetic compromises (Figures 5.3–5.5).
If dental implants are to be successful in solving functional, aesthetic, and phonetic needs of partially edentulous patients, they must satisfy the same demands that patients have for natural teeth or conventional restorations (Garber 1995) (Figure 5.6).
Replacement of Individual Teeth
Single missing teeth may be replaced with fixed partial dentures (FPDs) or single-implant-retained crown restorations. Priest (1996) performed a comprehensive review of failure rates for conventional FPDs, resin-bonded FPDs, and single-unit implant-retained crown restorations. Priest acknowledged the difficulties in obtaining data on FPD failures due to nonstandardized methods of reporting and recording failures. Priest (1999) also reported on single-tooth implants and their roles in preserving remaining natural teeth. He hypothesized that teeth adjacent to edentulous spaces should exhibit improved prognoses if restorative trauma (tooth preparations) is eliminated or minimized. He reported on implant survival and prosthetic complications of implants that replaced single missing teeth during a 10-year period. Priest further examined the preoperative status and survival of teeth adjacent to the implant restorations during the same 10-year time span. Priest reported on the results of 99 patients treated with 116 implants and 112 single-tooth implant prostheses between 1988 and 1998. The purpose of this study was to evaluate the role of implants in preventing the use of intact teeth for initial support of prostheses and in avoiding the use of additional teeth as abutments upon replacement of the existing restorations. Three implants failed over a 10-year period; the cumulative survival rate (CSR) was 97.4%. Priest reported that the complications included the loss of two implant crowns, screw loosening, broken screws, cement washout, margin exposure, and porcelain fracture. Of 196 teeth adjacent to edentulous spaces, 156 (79.6%) were intact or minimally restored. Only three of these teeth were restored as part of initial prosthodontic therapy. Over the ensuing 10 years, only one tooth required a replacement restoration; one tooth was extracted. Results of this patient evaluation demonstrated that implant survival over the 10-year period was favorable, with minimal prosthetic complications. Furthermore, Priest also concluded that teeth adjacent to single-tooth implants exhibited an extremely low complication rate. This report indicated that implants were effective in preserving intact teeth in patients undergoing initial prosthodontic therapy and prevented the use of additional teeth as abutments in patients whose existing prostheses needed to be replaced.
Figure 5.1 Anterior view of maxillary and mandibular fixed implant prosthesis 2 years after placement. The implants were placed according to an edentulous protocol where the treatment plan called for hybrid designs for both implant prostheses. Implants did not have to be placed in line with any of the artificial teeth. With the lips retracted, the metal/acrylic resin finish line was visible in the mandibular anterior vestibule.

Figure 5.2 This patient was also illustrated in Figure 5.1. Even with a full smile, the patient did not expose either the implants or metal/acrylic resin finish lines.

Figure 5.3 Clinical image of a patient who was missing the maxillary left central and lateral incisors. The implant that replaced the central incisor was placed distal to ideal, optimal placement for an aesthetic implant restoration, and possibly was placed too close to the implant in the lateral incisor site.

Figure 5.4 Clinical image of the patient in Figure 5.3 with the implant restorations in place. Note the less than optimal gingival-third contours of the implant restorations. The implant restorations were not symmetrical relative to the contralateral natural teeth.

Figure 5.5 Clinical image of the patient in Figures 5.3 and 5.4 smiling. Due to the patient’s low lip line, the aesthetic compromises in the gingival thirds of the implant restorations were not visible.

Figure 5.6 Clinical image of a patient with an implant-retained crown that replaced a congenitally missing left maxillary lateral incisor. Initially, there was not enough bone for optimal implant placement. Bone was grafted into the edentulous site and allowed to heal. The implant was then placed into an optimal position for an aesthetic and functional restoration.

Priest (2011) published another paper regarding tooth preservation in prosthodontic therapy. The purpose of this paper was to appraise tooth preservation while considering implants as additional and even preferred support mechanisms for dental prostheses. Priest reviewed and compared implants and traditional prostheses and their effects on abutment teeth, the use of periodontally and endodontically compromised teeth as abutments, and prosthetic complications potentially created by healthy remaining teeth. The evidence presented suggested that the long-standing objective of tooth preservation during prosthetic treatment be appended to include the use of dental implants for fixed/removable prostheses and to avoid or remove teeth presenting as liabilities that diminish the overall prognosis for a given patient. Priest stated that patients are not well served if they are faced with biologic, economic, and psychological burdens associated with ongoing revisions of dental rehabilitations using natural teeth. Priest advised dentists to use all means available to carefully evaluate remaining teeth to determine if they benefit or impair proposed prosthetic outcomes.
Schwartz et al. (1970) reported a mean life for 3-, 4-, and 5-unit FPDs was 12.3 years. Authors have identified the most frequent cause of failures for FPDs as recurrent caries and endodontic problems post prosthesis insertion (Schwartz et al. 1970; Reuter & Brose 1984; Walton et al. 1986).
Single-Unit Implant Restorations
Single-unit implant restorations were initially reported as having more mechanical problems than full-arch implant restorations. The success of single-unit implant restorations was dependent upon two distinct entities: osseointegration of the implants and biomechanical success of the restorations (Priest 1996). The long-term effectiveness (osseointegration) of dental implants has been well documented and is thought to be predictable in clinical practice (Adell et al. 1981; Lazzara et al. 1996; Testori et al. 2002; Misje et al. 2013).
Figure 5.7 Laboratory view of broken implant restorative components. This prosthesis was inserted in 1989. There was micro movement among the implant restorative components that was apparently below the patient’s consciousness. The movement continued until such time that the abutment screws fractured.

Figure 5.8 Laboratory image of a porcelain-fused-to-metal (PFM), implant-retained crown after the abutment screw fractured. Note the size of the buccal cantilever; this may have had a bearing on increased lateral forces and resulted in fracture of the abutment screw.

The biomechanical success and failure of single-unit implant restorations has been the subject of multiple reports (Jemt et al. 1990; Andersson et al. 1998; Lindh et al. 1998; Drago 2002; Pettersson and Sennerby 2013) (Figures 5.7–5.9). Eckert and Wollan (1998) reviewed 1170 dental implants, placed into anterior/posterior (A/P) maxillary and mandibular quadrants, in partially edentulous patients. They reported CSRs at 10 years in the mid to high 90%, except for the posterior mandible. They noted cement-retained crown failures (biomechanical) at 5 years to be 22.5%. Eckert and Wollan also noted a significant difference in biomechanical success after June 1, 1991. They noted that the prosthetic components from the implant manufacturer that they used were reengineered and improved for the system after this date. Eckert and Wollan determined that the relative risk for implants placed and restored prior to June 1991 was 2.096 times greater than for implants placed and restored after this date. They also noted a reduction in screw loosening from more than 46% to 3.2% after the abutment screws were redesigned.
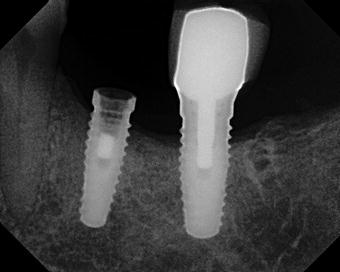
Figure 5.9 Radiograph of the implant restoration in Figure 5.8. The apical third portion of the abutment screw was retained within the implant after the restoration was dislodged from the implant.
Pettersson and Sennerby (2013) reported on the results of a 5-year retrospective review on patients restored with single-unit implants and restorations. Fifty-one patients with 160 implants were followed throughout their study. One implant failed at the time the healing abutment connection 4 months after insertion; the CSR for this study was 99.6%. The average crestal bone loss that was reported was 0.9 ± 1.6 mm after 1 year and 0.1 ± 2.4 mm after 5 years. Almost 15% of the implants (14.8%) had bone loss in excess of 2 mm; more than 5% (5.2%) of the implants had more than 3 mm bone loss after 5 years. Pettersson and Sennerby also noted that bone loss did not increase after the 1-year examination. One patient (2.0%) treated with six implants had significant crestal bone loss and recurrent peri-implant purulent infections at all implants. Pettersson and Sennerby concluded that the results of this retrospective 5-year study, with specific single implants, demonstrated a high survival rate (SR) and steady crestal bone levels.
Wittneben et al. (2013) reported on long-term outcomes associated with implant-supported fixed dental prostheses (FDPs) and single-implant-retained crowns. Out of 397 fixed reconstructions in 303 patients, 268 were single-implant-retained crowns; 127 were FDPs. Of these 397 implant-supported reconstructions, Wittneben and others reported that 18 had failed; this resulted in a failure rate of 4.5% and an SR of 95.5% after a mean observation period of 10.75 years (range, 8.4–13.5 years). They noted that the most frequent complication was ceramic chipping (20.31%) followed by occlusal screw loosening (2.57%) and loss of retention (2.06%). They reported that there were zero occlusal screw fractures, one abutment became clinically loose, and two abutment fractures. This resulted in a total mechanical/technical complication rate of 24.7%. The prosthetic success rate over a mean follow-up time of 10.75 years was 70.8%. Generalized attrition and FDPs were associated with statistically significantly higher rates of ceramic fractures when compared with single-implant-retained crowns. Wittneben and others also reported that cantilever extensions, screw retention, anterior versus posterior, and gender did not influence the chipping rate.
Dental endosseous implants have demonstrated high CSRs in numerous prospective and retrospective studies around the world. Dental implant manufacturers have continued to improve the machining of implant components and made improvements in the biologic designs to make dental implant treatment for edentulous and partially edentulous patients predictable and practical for patients and practitioners alike (Drago 1994). New developments in computer-aided design and computer-aided manufacturing (CADCAM) have made their way into dentistry in the twenty-first century.
Computer-Aided Design/Computer-Aided Manufacturing (CADCAM) Healing Abutments
Priest (2005) published a paper on virtual-designed and computer-milled implant abutments. He stated that CADCAM implant abutments will fundamentally change restorative protocols for implant dentistry. Standard implant prosthetic techniques relied on implant-level impressions and costly casting technology for abutment and crown fabrications. Priest noted that many dentists were uncomfortable making implant-level impressions and resorted to time-consuming conventional techniques of intraoral abutment preparation or did not offer implants as treatment alternatives for their patients. CADCAM implant abutments have been proven to be more precise than those created using traditional casting technology. This increased accuracy had specific applications to implant dentistry, where component precision may affect implant longevity, prosthetic success, and ease of restoration. Three current (at the time of publication – 2005) CADCAM implant abutment systems were reviewed, including a description of an innovative digital system which eliminated the need to make implant-level impressions for construction of implant abutments. With the use of specialized healing abutments (Encode, Biomet 3i, Palm Beach Gardens, FL, USA) (Figures 5.10 and 5.11), definitive impressions could be made at the healing abutment level, without removing the healing abutment (Figure 5.12). That impression could be poured in dental stone, and the cast would be optically scanned in a dental laboratory or milling center (Figures 5.13 and 5.14). The codes on the occlusal surfaces of the healing abutment would then be recognized by a specific computer software program (Figure 5.15), and patient-specific definitive abutments would be created virtually (Figures 5.16–5.18). Once the abutment design was approved, the abutment would then be milled and shipped to a commercial dental laboratory for fabrication of the definitive crown.
Figure 5.10 Laboratory image of the occlusal surface of a BellaTek® Encode® Healing Abutment in the master cast. This is a two-piece healing abutment; the codes on the occlusal surface of the healing abutment can be recognized by a computer software program and provide information relative to the implant/abutment connection, implant restorative platform size, orientation of the implant hex, and orientation of the implant to a dental designer/dental laboratory technician for fabrication of a CADCAM abutment.

Figure 5.11 Clinical occlusal image of a BellaTek Encode Healing abutment in place.

Figure 5.12 Laboratory image of the intaglio surface of a poly vinylsiloxane impression of the occlusal surface of the CADCAM healing abutment. The occlusal codes were accurately captured in the impression and would be transferred to the master cast.

Figure 5.13 Laboratory occlusal image of the master cast that included the occlusal codes of the CADCAM healing abutment. The codes were supragingival and were easily recognized by the laboratory scanner.

Figure 5.14 Laboratory image of the optical scanner used in this CADCAM system.
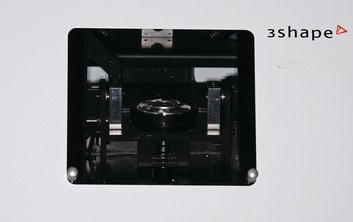
Figure 5.15 This is a screenshot of the computerized digital scan (.stl file) of a mandibular master cast with two CADCAM healing abutments in place.
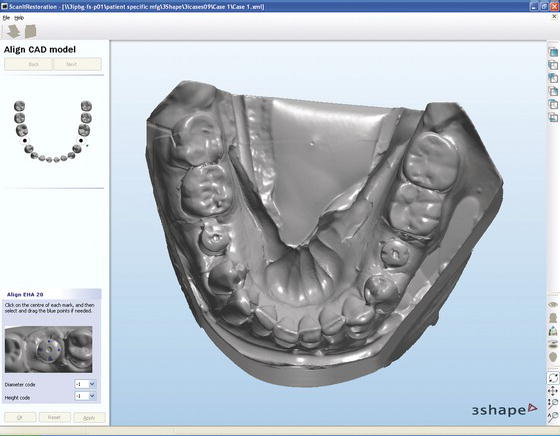
Figure 5.16 This is a screenshot of the virtual abutment design for a mandibular second premolar definitive CADCAM abutment.
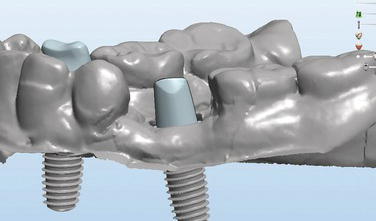
Figure 5.17 This is a screenshot of the virtual, custom abutment design for a mandibular canine definitive CADCAM abutment. The abutment pictured here would be milled from a titanium blank.

Figure 5.18 This is a screenshot of the virtual abutment design for a mandibular premolar definitive CADCAM abutment. The abutment pictured here would be milled from a titanium blank and then coated with a gold-colored titanium nitride coating.

The original protocol still called for a master cast with an implant analog to fabricate the definitive crown (Drago 2006). In some instances, clinicians made implant-level impressions of the implants, and the laboratories placed an Encode Healing Abutment into the analog in the master cast. This negated one of the benefits of the Encode Impression System. As CADCAM protocols and software programs became more sophisticated, robotic analog implant placement was also developed (Biomet 3i, Palm Beach Gardens, FL, USA). After the scanning process was completed, the digitized data were sent to an automated robot in a different section of the milling center, whereby the dental stone replica of the healing abutment was removed and an implant analog was placed (Figures 5.19–5.23). This cast was packaged with the CADCAM abutment and returned to the commercial dental laboratory for fabrication of the definitive implant crown restoration (Figures 5.24–5.26).
Figure 5.19 This is a laboratory image of the computerized robot designed to place implant analogs into master casts via digitized data received from the scan of the CADCAM healing abutment in the master cast. Reproduced with permission from Biomet 3i.

In spite of the fact that this CADCAM system is relatively new, several reports have been made relative to the accuracy of the system, including the robotic placement of analogs into master casts. Eliasson and Ortorp (2012) published the results of a study where they compared the accuracy of implant analog placement in working casts using a robot technique and an impression of Encode Healing Abutments with traditional implant-level impressions and fabrication of master casts. One acrylic resin master model was fabricated; three posterior implants were placed into each posterior segment. The implants were placed vertically and relatively parallel to each other. Encode Healing Abutments (Biomet 3i, Palm Beach Gardens, FL, USA) were placed onto the test side implants; conventional pickup implant impression copings were placed onto the implants on the control side. Fifteen impressions were made with a poly vinylsiloxane impression material. Implant analogs were placed into the casts by a robot on the test side; implant analogs were attached to the impression copings, and casts were poured in dental stone for the control side. The center point of each implant analog restorative platform was measured with a laser measuring machine in the x-, y-, and z-axes, as were also the angular direction of the center axis and the position of the antirotational hex. The statistical significance was set at P < 0.05. Eliasson and Ortorp reported that the mean center point deviations for the test and control sides were 37.4 µm versus 18.5 µm (P = 0.001) in the x-axis, 47.3 µm versus 13.9 µm (P < 0.001) in the y-axis, and 35.0 µm versus 15.1 µm (P < 0.013) in the z-axis. The mean angle error was reported to be 0.41° for the test sides and 0.14° for the control sides (P < 0.001). The mean rotation of the hexagon was reported to be 2.88° for the test sides and 1.82° for control side (P < 0.001). Eliasson and Ortorp concluded that casts made with conventional implant impressions and casts made with robotic analog placement presented low levels of displacement of the implant analogs in all casts. They also concluded that the test technique was less precise, but the difference in accuracy was small; both techniques were precise enough for single crowns and short-span, implant-supported fixed partial prostheses.
Figure 5.20 This is a laboratory image of a mandibular cast in place on a holder during the process that involved drilling a hole into the cast in the location of the CADCAM healing abutment that corresponded to the location of the implant intraorally.

Figure 5.21 Laboratory image of the hole drilled into the cast in Figure 5.20. The hole was slightly oversized relative to the planned implant analog. The oversize allowed room for the adhesive that would hold the analog in its correct position.

Figure 5.22 Laboratory image of the robotic element that held the analog in place per the digitized instructions received from the scan of the CADCAM healing abutment. The analog was held in place by the robot until the adhesive was fully cured/set.

Figure 5.23 Laboratory occlusal image of the analog in place within the master cast. This cast was called a robocast. The implant analog was correctly oriented in three dimensions per the digitized data received from the scan of the CADCAM healing abutment.

Figure 5.24 Laboratory image of a titanium milled abutment and its package. These were packaged and shipped to the commercial dental laboratory for fabrication of the definitive implant-retained crown restoration.

Figure 5.25 Laboratory occlusal image of the titanium abutment in Figure 5.24 in place on the analog in the master cast. The definitive crown restoration was fabricated on this abutment.

Figure 5.26 Laboratory occlusal image of the definitive crown in place on the titanium abutment in Figure 5.24 in the master cast.

Howell et al. (2012) also compared the accuracy of implant master casts fabricated using Robocast™ Technology (Biomet 3i, Palm Beach Gardens, FL, USA), with master casts fabricated using traditional transfer (closed-tray) and pickup (open-tray) impression techniques. A stereolithographic replica of a Kennedy Class I human mandible was fabricated for use as the master model. Implants were placed into each posterior quadrant (teeth #18, #20, #29, #31), implants were placed vertical and parallel to each other on one side, and implants were placed divergent on the opposite side. Impressions were made of the master model (patient replica model) with Encode Healing Abutments (E), open-tray (O), and closed-tray (C) impression copings. Identical metallic spheres were placed into each implant analog in the stone master casts. Casts/spheres were scanned using a digital scanner (3 Shape, Denmark). Measurements were made between the center points of the spheres using Rapidform XOR (INUS Technology, South Korea) software and compared to the master model. Data were divided into parallel (P), nonparallel (NP), and individual (I) sites. Differences were analyzed using ANOVA and Tukey tests (α = 0.05). Encode master casts were less accurate than the open-tray impression groups (O) in the nonparallel (NP) sites. Encode master casts were less accurate than the O and closed-tray impression (C) groups in the parallel implant (P) sites. Master casts of the NP implants demonstrated less accuracy than P implants within the Encode group. Encode master casts were less accurate than the O and C groups at site #29. Site #20 was less accurate than site #31 in the Encode group. Howell et al. (2012) concluded that within the limitations of this lab-based study and analysis, the Encode Impression System resulted in master casts that were less accurate than master casts made from traditional open- and closed-tray impression techniques. They also concluded that further research was necessary before specific clinical judgments can be made. The clinical takeaway from Howell et al.’s (2012) research was that, for nonparallel implants, a clinical try-in appointment may be needed for complex cases involving multiple implants. The clinical takeaway for Eliasson and Ortorp’s (2012) research was that for single implants, robot-fabricated master casts will likely be accurate enough for clinical use.
Commencing in approximately 1998, CADCAM technology was used to create custom implant abutments (Kucey and Fraser 2000). Custom abutments, by definition, may be designed to provide physiologic peri-implant soft tissue contours that mimic the gingival architecture around natural teeth. CADCAM processes eliminate the majority of the limitations associated with conventional casting technology; costs may also be reduced (Drago 2006). In 2004, another CADCAM process was developed to further simplify the clinical and laboratory processes associated with custom CADCAM abutment fabrication. It involved the use of specially coded healing abutments (BellaTek® Encode Impression System, BIOMET 3i, Palm Beach Gardens, FL, USA). Facets or codes were machined into the occlusal surfaces of two-piece healing abutments that enabled a computer software program to identify:
The initial protocol called for definitive fixed prosthodontic-type impressions of these healing abutments and fabrication of stone master casts. The casts needed to be mounted in a specialized articulator mount for insertion into a laboratory scanner. The codes on the healing abutments would then be read by the scanner, and a dental designer would then design the abutment, and the abutment would be returned to the commercial dental laboratory for fabrication of the definitive crown.
Intraoral Scanning
Ramsey and Ritter (2012) published a report on the utilization of digital technologies for fabrication of definitive implant-supported restorations. They noted that the introduction (2005) of specially coded healing abutments dramatically simplified the task of obtaining implant impressions. Such coded abutments (BellaTek® Encode® Healing Abutments, Biomet 3i, Palm Beach Gardens, FL, USA) eliminated the need for impression copings. In their place, clinicians could make supragingival impressions and send the impressions to commercial dental laboratories for fabrication of patient-specific abutments and restorations. Ramsey and Ritter combined this technology with digital intra-oral scanning and noted that this further simplified the procedures and decreased the time between impression making and delivery of definitive restorations. They also noted that it offered additional benefits to both patients and clinicians.
Ramsey and Ritter stated that an alternative to making conventional elastomeric impressions for conventional fixed prosthodontic treatment was to record the intraoral geometry of tooth preparations with a digital scanner. Christensen (2008) rhetorically raised this same question earlier. Commercially available intraoral scanning (IOS) systems have been available for several years and have made it possible to capture digital informatio/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


