5
Traumatology (Adult)
In cases of trauma to the dentition, a comprehensive medical history and a history of the traumatic incident are essential. The medical history should include immunization status, allergies, conditions that require pre-medication with prophylactic antibiotics, and any other specific medical problems or systemic conditions that require special consideration in the rendering of dental care.Awell-documented history of the traumatic incident provides valuable information about the location, nature, and extent of the injuries; the probability of contamination; the best choice of treatment based on time factors; and the prognosis for recovery.
Since trauma sufficient to create dental injury could have created more extensive damage, it is important to rule out neurologic involvement or other systemic injury. Determine whether the patient was unconscious or has experienced headache, nausea, or vomiting. Obtain a history of past trauma to the dentition and determine whether any treatment has already been rendered. Inquire about the nature, severity, and duration of any dental pain and whether there has been a change in occlusion.
Crown Fractures
Brief Overview
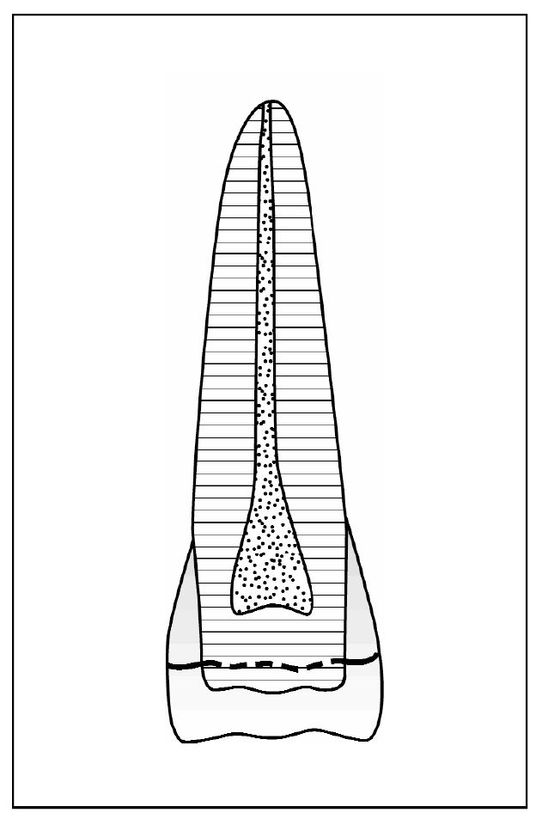
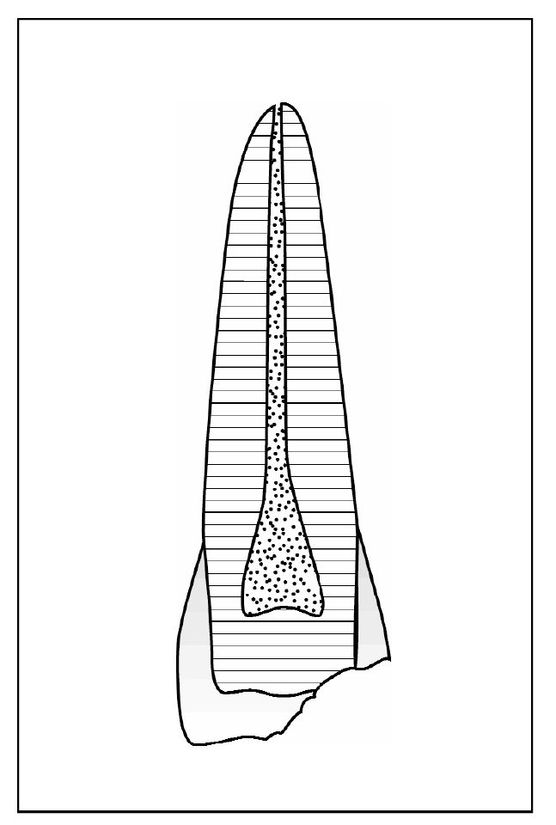
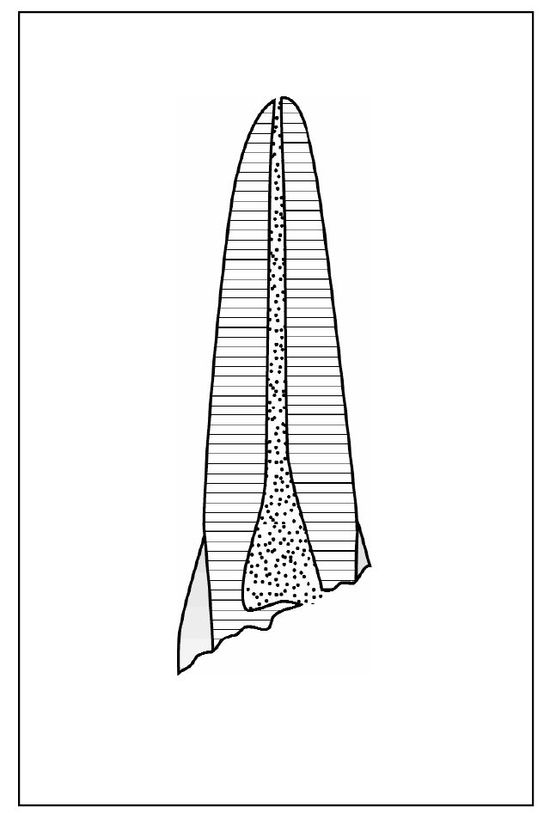
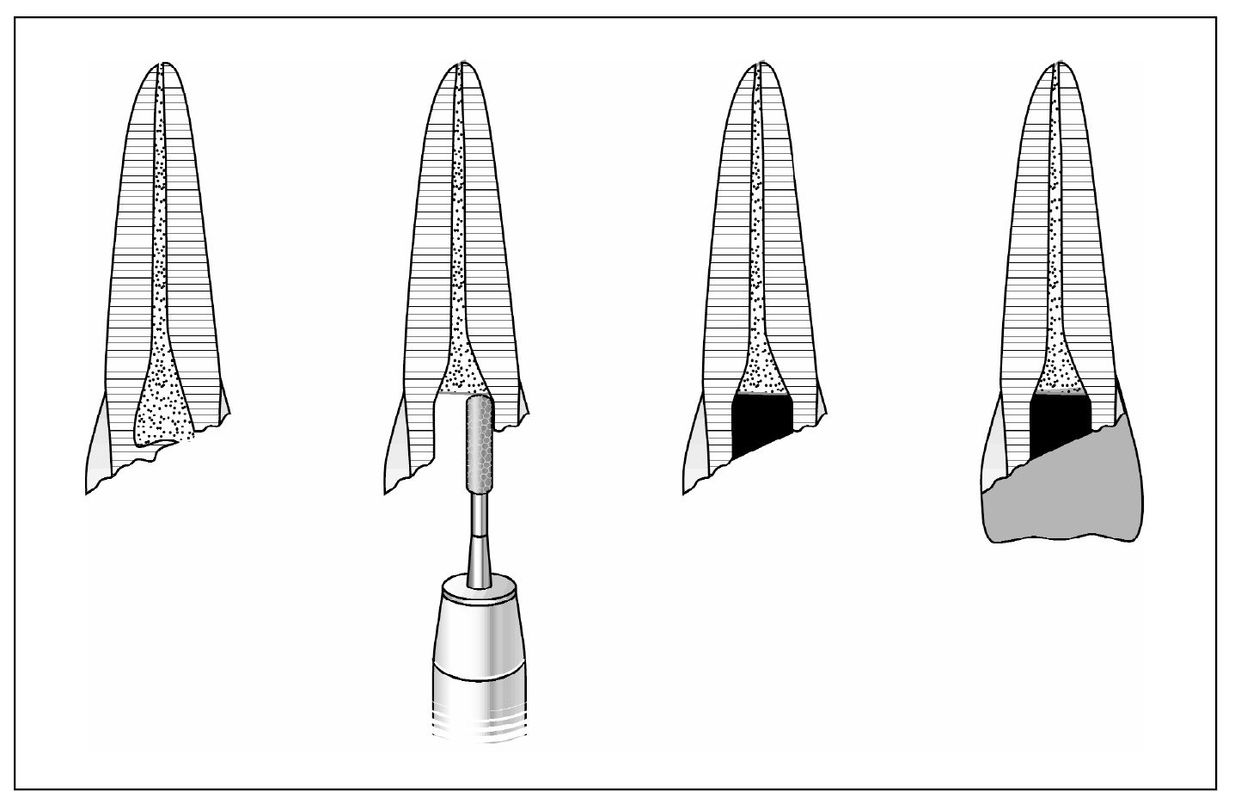
Crown fractures are typically caused by concussive contact from falls, sports, auto accidents, and altercations. The anterior teeth are most frequently involved. The fractures may be associated with other injuries, such as soft tissue laceration and subluxation. The force of a blow severe enough to cause fracture may also have caused displacement that can affect pulpal and periodontal status. The pain or discomfort reported immediately is usually the result of concussive injury. Fractures limited to the anatomic crown can be placed in three categories. Infraction is an incomplete fracture of enamel without loss of tooth structure (Fig 5-1). Uncomplicated fracture may involve loss of structure limited to enamel or including both enamel and dentin (Fig 5-2). A fracture large enough to expose the pulp is called a complicated crown fracture (Fig 5-3).
Infraction
In the case of infraction the crown is intact. Crack lines in vertical, horizontal, or oblique directions may or may not be visible in direct light. The patient may have pain on function.
Complicated Crown Fracture
Evidence of pulpal exposure will be a visible bleeding site on the fractured surface. The patient may experience pain with exposure to air, thermal change, or function. Sharp edges and poor esthetics may also be reported by the patient.
Treatment
Treatment decisions will vary depending on the size of the exposure, the amount of time since the injury, the evidence of luxation injury, the stage of root development, and the potential restorative need for a post.
For teeth with immature root development, the goal of treatment should be to preserve the vital pulp tissue despite injury and contamination so that root development may proceed to completion (Fig 5-5). For teeth with mature root development, preservation of pulpal vitality may not be possible if there has been a displacement injury, due to disruption of vascular supply to the fractured tooth (Fig 5-6).
| Step 1 | Pulp capping with calcium hydroxide is indicated only for small exposures with minimum time since injury. Because microleakage will compromise pulp vitality, the restoration placed over the calcium hydroxide must achieve an effective seal. A composite resin, when properly bonded, will resist microleakage. For temporary restoration, zinc oxide-eugenol (ZnOE) cement will provide the best seal, but will interfere with the polymerization of subsequently placed composite resin materials. |
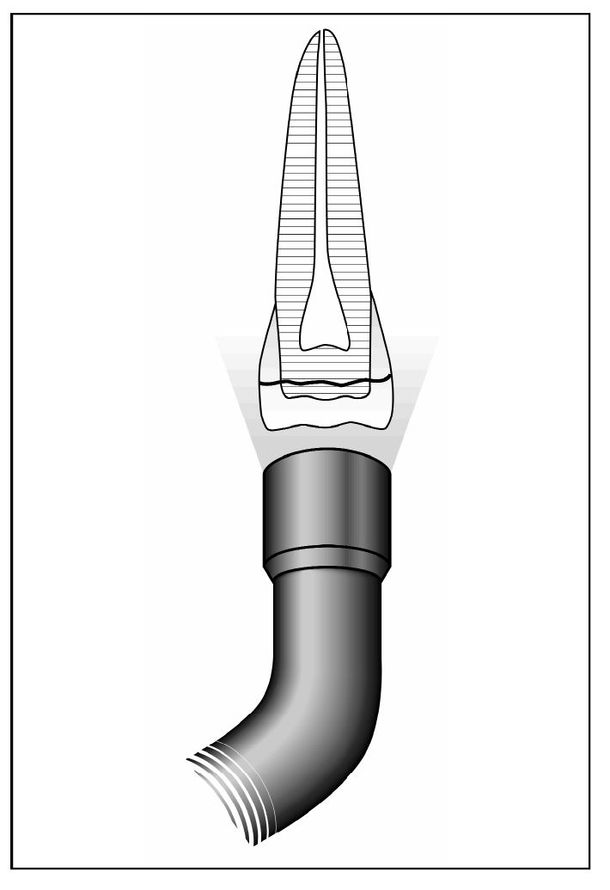
| Step 2 | A pulpotomy is indicated when contaminated and inflamed pulpal tissue is limited to the most coronal area of the pulp and can be removed to expose vital tissue capable of repair. The extent of inflamed tissue that must be removed will vary depending on the length of time since the injury, size of exposure, and patient response to the trauma. Usually an exposure of less than 24 hours can be successfully treated by a partial pulpotomy to a depth of 2 mm apical to the fracture site (Fig 5-7). |
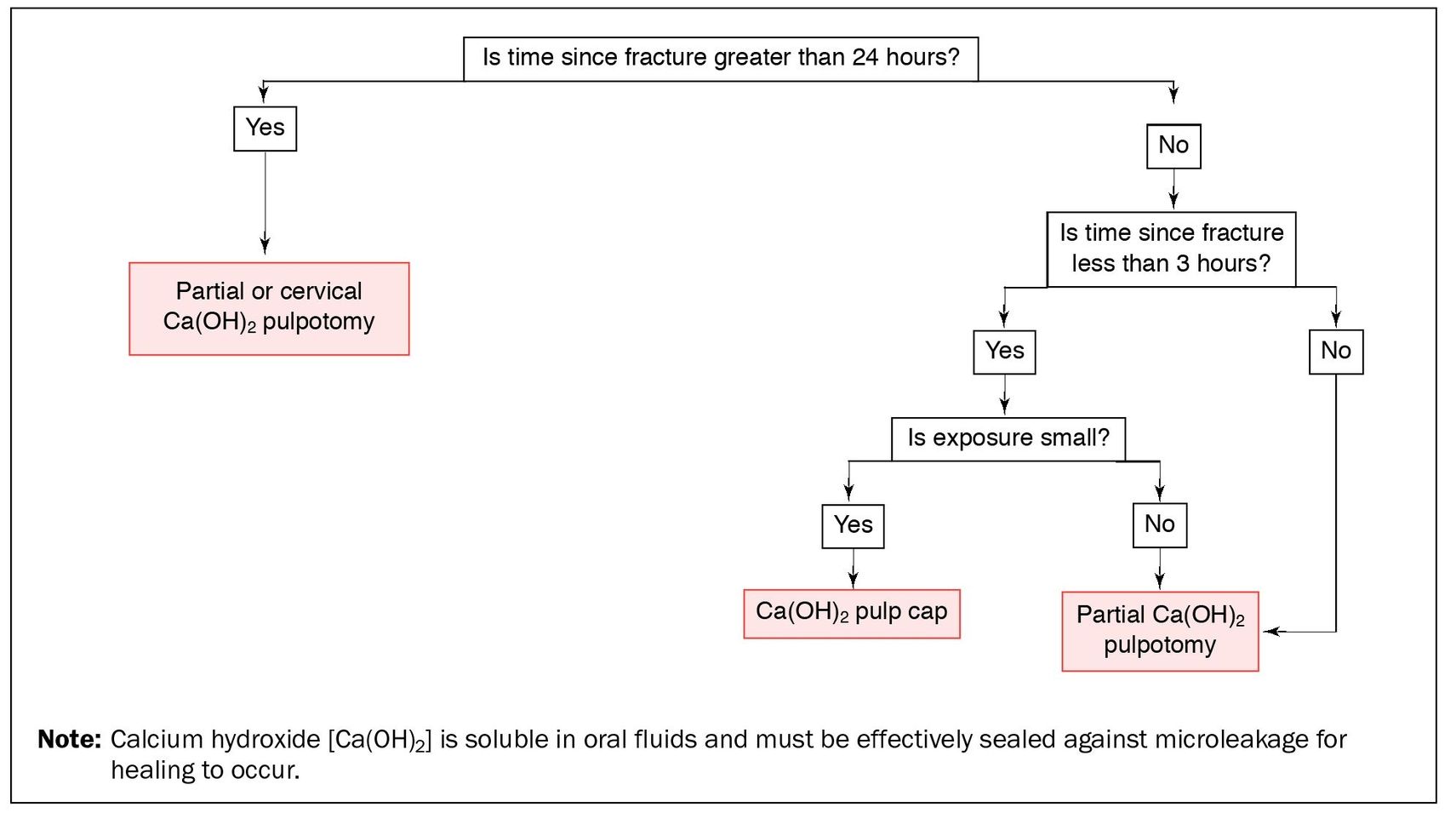
Fig 5-5 Treatment decisions for complicated crown fractures on teeth with immature roots.
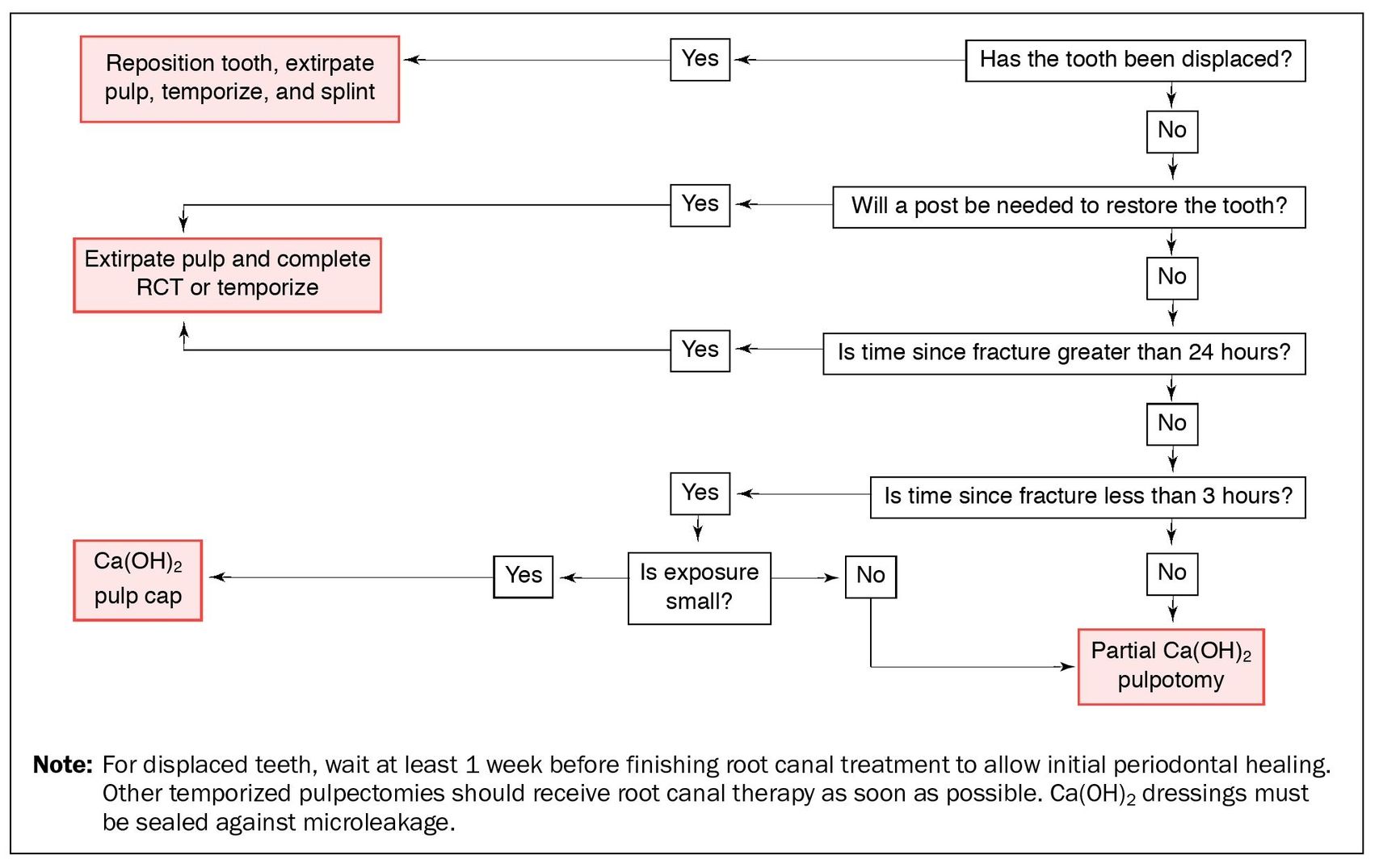
Fig 5-6 Treatment decisions for complicated crown fractures on teeth with mature roots.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses