CHAPTER 5 Radiographic Techniques
RADIATION SAFETY AND PROTECTION
Still, dental health professionals must be concerned about any risk that the patient may encounter during therapy. Concern is focused on three primary biologic effects of low-level radiation: (1) carcinogenesis, (2) teratogenesis (malformations), and (3) mutagenesis. Carcinogenesis and malformations are a response of somatic tissues and in most instances are believed to have a threshold response; that is, a certain amount of radiation is necessary before the response is seen. Mutation may occur as a response of genetic tissue (gonads) to x-radiation and is believed to have no threshold. In general, younger tissues and organs are more sensitive to radiation, with the sensitivity decreasing from the period before birth until maturity. It must also be recognized that far higher doses of radiation can be withstood by localized areas than by the whole body. We know that we live in a world that exposes us to natural background radiation averaging 360 mrem per year (3.60 millisievert) in the United States. Medical and dental radiographic examinations add to that exposure and so must be ordered judiciously.
The practitioner and staff can physically protect the patient and indirectly protect themselves from unnecessary exposure to radiation by using correct technique. The most obvious method of protecting the patient is to shield those areas not being evaluated. This is easily accomplished using a lead apron and thyroid collar (Fig. 5-1).
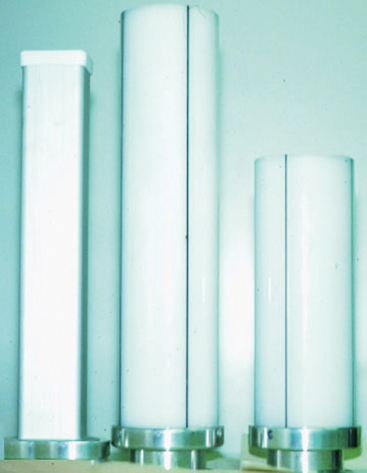
Faster film speeds have contributed most significantly to the reduction in radiation to the patient. Film speeds of the D and F groups are available for intraoral radiography. Faster film also reduces error from patient movement, a consideration with the pediatric patient. Extraoral (panoramic) radiography uses film-screen combinations that also have reduced exposure times. Recently, there has been an increased use of beam-positioning devices (Fig. 5-2), which virtually eliminate some of the technical errors, particularly film cone cuts. Using different lengths and shapes of the cone (Fig. 5-3) has also aided in the reduction of patient radiation exposure. Use of a long rectangular collimator reduces the area unnecessarily exposed to radiation by almost 4 square inches compared with a round collimator. The use of higher kilovolt peak techniques reduces patient exposure to radiation and lowers contrast, thus increasing the number of shades of gray on the film. An additional benefit of using high kilovolt peak technique is that the exposure time is shortened, which potentially reduces retakes caused by patient movement.
SELECTION CRITERIA AND RADIOGRAPHIC EXAMINATIONS
The decision to make radiographs is based on a thorough evaluation and examination of the patient. Radiographs should be made only when there is an expectation that disease is present or when an undetected condition left untreated could adversely affect the patient’s dental health. Therefore the decision to use ionizing radiation is based on professional judgment (Table 5-1).
| Patient Category | Child | |
|---|---|---|
| Primary Dentition (before eruption of first permanent tooth) | Transitional Dentition (after eruption of first permanent tooth) | |
| New Patient* | ||
| All new patients to assess dental diseases and growth and development | Posterior bite-wing examination if proximal surfaces of primary teeth cannot be visualized or probed | Individualized radiographic examination consisting of periapical/occlusal views and posterior bite-wings or panoramic examination and posterior bite-wings |
| Recall Patient* | ||
| Clinical caries or high-risk factors for caries† | Posterior bite-wing examination 6-month intervals or until no carious lesions are evident | |
| No clinical caries and no high-risk factors for caries† | Posterior bite-wing examination at 12- to 14-month intervals if proximal surfaces of primary teeth cannot be visualized or probed | Posterior bite-wing examination at 12- to 24-month intervals |
| Periodontal disease or a history of periodontal treatment | Individualized radiographic examination consisting of selected periapical and/or bite-wing radiographs for areas where periodontal disease (other than nonspecific gingivitis) can be demonstrated clinically | |
| Growth and development assessment | Usually not indicated | Individualized radiographic examination consisting of a periapical/occlusal or panoramic examination |
| Adolescent | Adult | |
|---|---|---|
| Permanent Dentition (before eruption of third molars) | Dentulous | Edentulous |
| Individualized radiographic examination consisting of posterior bite-wings and selected periapicals. A full mouth intraoral radiographic examination is appropriate when the patient presents with clinical evidence of generalized dental disease or a history of extensive dental treatment. | Full mouth intraoral radiographic examination or panoramic examination | |
| Posterior bite-wing examination at 6- to 12-month intervals or until no carious lesions are evident | Posterior bite-wing examination at 12- to 18-month intervals | Not applicable |
| Posterior bite-wing examination at 18- to 36-month intervals | Posterior bite-wing examination at 24- to 36-month intervals | Not applicable |
| Individualized radiographic examination consisting of selected periapical and/or bite-wing radiographs for areas where periodontal disease (other than nonspecific gingivitis) can be demonstrated clinically | Not applicable | |
| Periapical or panoramic examination to assess developing third molars | Usually not indicated | Usually not indicated |
The recommendations contained in this table were developed by an expert dental panel comprised of representatives from the Academy of General Dentistry, American Academy of Dental Radiology, American Academy of Oral Medicine, American Academy of Pediatric Dentistry, American Academy of Periodontology, and American Dental Association under the sponsorship of the Food and Drug Administration (FDA).
* Clinical situations for which radiographs may be indicated include the following:
† Patients at high risk for caries may demonstrate any of the following:
Courtesy Carestream Health, Inc.
The criteria for making radiographs, developed in part by the Conference on Radiation Exposure in Pediatric Dentistry, were summarized by Nowak and colleagues1 as follows.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses