5
Orthognathic Surgery
INTRODUCTION
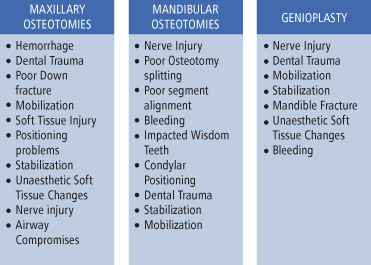
Complications may occur at any point in time along the course of treating the patient undergoing orthognathic surgery. From diagnosis to discharge, the list is extensive, and, for the most part, preventable. Preparation is the key. Careful treatment planning and excellent technical training to manage these potential risks are paramount to the success of orthognathic surgery. Multiple reviews of the incidence and types of complications have been reported in the literature.1–10 A Medline search in early 2011 of “orthognathic surgery complications” revealed 479 articles. The majority of these articles focus on the incidence of complications related to a specific osteotomy (Fig. 5.1).
Fig. 5.1. Complications by osteotomy location.
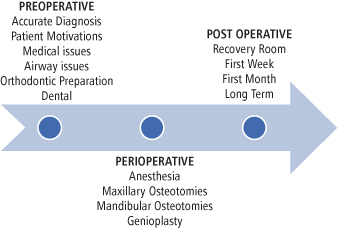
A list of complications from orthognathic surgery can be divided into three main sections: preoperative complications, perioperative complications, and postoperative complications. For the purposes of this chapter, the preoperative complications will be considered if they have occurred before the actual surgery has started. Perioperative complications are those that take place in the operating room during the surgical procedure, and postoperative complications occur anytime after the surgery is completed until patient discharge from the practice (see Fig. 5.2).
Fig. 5.2. Preoperative, perioperative, and postoperative complication time frames.
PREOPERATIVE COMPLICATIONS
Diagnosis
Accurate diagnosis of the skeletal facial deformity is the beginning of the time line for the orthognathic surgical patient. The diagnosis will dictate which osteotomies will be necessary to align the facial skeletal components into a functional, aesthetic, and orthognathic position. Cephalometric analysis, face-bow mounted dental models and/or computer generated models, photographs, and clinical measurements must be accurate and reproducible.
The accurate gathering of this data is essential to the outcome of the surgical plan.11 If the patient’s head position is not correct during record taking, the dental models not mounted with the right occlusion, or the facial measurement not correct, the skeletal components will not be surgically moved into the correct predicted position. To insure that data collection is consistent, protocols must be established by the practitioner so that the information can be consistently utilized with minimal margin of error while transferring the data from the patient to the laboratory and the computer, and then the operating room. From the use of light-cured acrylic splints to stereolithographic biomodeling generated splints from computer tomography technology, the accuracy of obtaining the predicted occlusion continues to improve.12–14
Patient Motivation
During the initial phases of treatment, finding out the reason why a patient is motivated to seek treatment is another key component to successful outcome.15–18 If patient expectations cannot be met or if they are unrealistic, then no matter what type of accuracy is obtained with the workup or surgery, the patient will not be satisfied. This is not only a disappointment to the surgeon but a true failure to the patient. The use of patient preoperative questionnaires may elucidate the patient’s initial motivation and understanding of why they are seeking surgical consultation. If the patient’s expectations are not realistic and cannot be met then it may be best to defer treatment.
Time spent educating the patient and family until they are able to understand what the surgery can realistically accomplish will enable for better emotional and physical outcomes. There are many resources available to help the surgeon in this regard from written materials to Web-based teaching tools to video imaging of the surgical procedures. The type of teaching tools can be customized for each patient and family. This is the beginning of the informed consent process.
Medical Issues
Medical issues that may be associated with or create skeletal facial deformities may also be an undiagnosed “monster in the closet.” Diseases such as pituitary adenomas; bleeding dyscrasias; sleep apnea; myotonias; temporomandibuar joint disorders, including tumors; idiopathic condylar lysis; arthritis; and psychological diseases are to name a few. The majority of these problems not only affect the intraoperative anesthesia and medical management of patients but the long-term function and stability of the results as well. The impact of several medical conditions on perioperative planning can be found in other texts and is not the focus of this work.
Airway Issues
The initial airway evaluation of the orthognathic patient includes not only looking at the anatomic issues that the patient has preoperatively, but how the postoperative changes in the skeletal support of the airway will affect the airway patency.19,20 The presence of large tonsillar tissues, deviated nasal septum, chronic sinus disease, large tongue, or even pulmonary diseases such as asthma will affect the patient’s perioperative airway and postoperative management. Therefore, patients who are undergoing orthognathic surgery should be screened for signs of airway issues as well as possible obstructive sleep apnea (OSA). This includes excessive daytime somnolence, snoring, increased body mass index (BMI), and medical conditions related to OSA. If these findings are positive then further investigation for sleep disorders with appropriate studies including a polysomnography (PFG) should be undertaken. If sleep apnea is diagnosed, then the proposed treatment plan may require modifications according to the risk of potential airway compromise from moving the skeletal bases and a plan can be developed instead to improve the airway.21,22
Speech may also be affected by movement of the jaws.23,24 Changes in speech are best managed by involving a specialist in speech therapy from the beginning of treatment planning. Those patients that present with large skeletal discrepancies, especially those with apertognathia, may have learned to compensate with lip and tongue habits that will need to be addressed in the pre- and postoperative periods. Having a formal speech evaluation preoperatively will help the team provide good speech therapy in the postoperative period.
Another area where a speech pathologist’s evaluation will be valuable is velopharyngeal incompetence pre- and postoperatively.25,26 A formal nasopharyngoscopy is necessary to document the movement of the posterior pharyngeal walls and soft palate when evaluating for velopharyngeal incompetence. Special consideration and careful planning during intubation for orthognathic surgery are required for patients who had correction of velopharyngeal incompetence with pharyngeal flaps. Flap release and secondary reconstruction at a later time once tissue revascularization is complete may be required.
Orthodontic Preparation
Communication mishaps with the orthodontist are also an area where complications may occur preoperatively. Once the initial diagnosis and treatment plan is established, it is important for the surgeon to follow along as the orthodontic preparation of these patients is progressing. Taking periodic study models will enable the treating team to discuss progression and identify potential problems that may impact on the ability to execute the planned surgical movements and achieve the desirable results.27–32
Accurate diagnosis of the skeletal discrepancy to be corrected is paramount for appropriate orthodontic preparation and avoidance of perioperative complications and future relapses. Such is the case of transverse deficiencies that will lead to relapse if not recognized and addressed appropriately early in the treatment. When segmental osteotomies are required, their position should be clearly communicated so adequate spaces between the roots can be created orthodontically and the bony cuts can be safely performed. Furthermore, appropriate leveling and alignment of the dentition will allow for spaces to be created accommodating both the surgical movements and the postoperative final orthodontic manipulations for case completion. Finally, details such as the position of the orthodontic appliances, utilization of the appropriate arch wire, and no manipulation whatsoever once impressions for surgical planning are obtained require clear understanding.
Dental Issues
For many dental issues such as the extraction of impacted thirds, space preparation for congenitally missing teeth must be addressed in the preoperative period.
The presence of impacted mandibular third molars, for example, increases the risk of an unfavorable osteotomy (bad split). It appears that this may be an age-dependent event. The younger the patient the more likely that the split will be “bad” if the tooth is taken at the time of the split. It has been recommended that if the teeth are going to be removed prior to surgery, extractions should be performed between 6 and 9 months prior to the osteotomy. This may decrease the risk of a “bad split” due to an impacted tooth in the osteotomy site.33–36
If the patient is missing teeth that are to be replaced with dental implants, the timing of when implants and bone grafting to prepare implant sites is of importance.37–39 Soft tissue grafting and bone grafting require flap designs that may compromise the blood supply to the alveolus of the maxilla if a Le Fort I osteotomy is expected. Adequate time should be allowed for these tissues to revascularize. Typically, at least 6 months should be allowed before Le Fort I surgery to insure adequate revasculariztion.
Congenitally missing teeth pose a problem related to arch length and also the prosthetic rehabilitation of these cases. If the congenitally missing tooth is going to be replaced with a dental implant then two issues must be addressed. First, how will enough room be achieved in three dimensions to place the fixture? Is there a need to expand the arch surgically to gain length? Or can simple orthodontic movement create enough room?
Second, once spacing is achieved, is there enough bone there to support an implant? If not, then when should bone grafting be done? For instance, the incisions that are created to access the osteotomies may impact on local soft tissue healing when placing onlay grafts to the alveolus and potentially lead to vascularity issues and wound healing problems. It is also possible to graft at the time of orthognathic surgical positioning. However, care at these alveolar sites related to the ability to maintain vascularity of the soft tissues over these grafts is important. Modifying the incisions to provide maximum coverage of these grafts and thus vascularity is essential to survival of these grafts.
INTRAOPERATIVE COMPLICATIONS
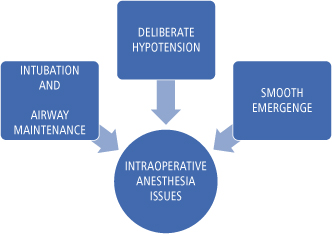
Proper communication between the surgeon, nursing, and anesthesia staff is essential (Fig. 5.3).
Fig. 5.3. Possible intraoperative anesthesia-related complications.
It is essential to control blood loss with an excellent technique and understanding of surgical anatomy; however, using hypotensive anesthetic techniques may also help.40 The most common use of this technique is during the Le Fort I osteotomy downfracture. This process is not without its own potential complications of circulatory and vascularity issues to the maxilla. Return to a normotensive stage should be accomplished as soon as the downfracture is completed.40–43
MAXILLARY SURGERY: INTRAOPERATIVE COMPLICATIONS
The work horse of maxillary orthognathic surgery is the Le Fort I osteotomy. Hemorrhage is the most well known complication and has been well documented as a complication of this osteotomy.44–47 However, errors in execution of this procedure can lead to compromises in the dentition, bone healing, and soft tissue healing. Other issues that have been reported as a result of poor intraoperative technique include neural deficits; nasal airway obstruction; ocular issues, including blindness; and sinus pathology.48–54
Dental Trauma
Dental trauma from Le Fort osteotomy is usually a result of improper osteotomy placement. For example, if the horizontal maxillary osteotomy is positioned too inferiorly there is a risk of transection of the root apices.55 It is generally recommended that these osteotomies are planned at least 5 mm above the apices of the maxillary roots.56–58 Other complications that arise are related to maxillary segmental osteotomies that are used to either level the occlusal plane or for correction of transverse discrepancies.59,60 Adequate space is required between the roots of the teeth at the sites of the planned vertical osteotomies to allow for bony coverage of the roots. When preparing the space orthodontically care should be taken to not tip the teeth but rather achieve bodily movement. Careful radiographic examination of the root length and adequacy of space in cases of segmental osteotomies are essential in avoiding dental injuries perioperatively. Drawing the root surfaces on the casts or utilization of three-dimensional software for osteotomy planning may also help in decreasing these potential complications.
Although pulp necrosis post Le Fort osteotomy is unusual, it does occur. The pulp tissues will heal spontaneously despite an impaired blood supply.61 Vitality testing is not a reliable indicator of pulpal necrosis because between 6% and 29% of all teeth remain insensate up to 54 months post osteotomy.62 Endodontic treatment should only be indicated once the clinical symptoms or radiographic evidence is demonstrated that it is clearly necessary. One may notice a darkening of the maxillary incisor or pink color. It is best at the initial postoperative visits to wait for at least 8 weeks before embarking on endodontic treatment. This will allow for possible revascularization and vitalization that is often the case with these teeth. However, if the teeth remain nonvital then endodontic treatment is essential.
Intraoperative complications specific to the maxillary bone itself include poor fracture of the maxilla, inability to mobilize the segments to gain anterior movement or width, and difficulty posteriorly or superiorly positioning the maxilla.
Soft Tissue Issues
The gingival and palatal tissues at these sites can also be injured by lacerating it from sharp instruments or rotary burs and during the osteotomies as well as by crushing of the tissues when the segments are collapsed during a segmental osteotomy. Attention to these details will prevent injury in these sites and the use of segmental surgery can be done in a predictable manner with good results.63
Lacerations to the soft tissues of the hard palate or alveolar mucosa may also occur with improper use of cutting instruments. This soft tissue injury may lead to necrosis of the soft tissues and possibly vascular compromise of the bone in these areas (Fig. 5.4).64 Clinically, the vascular compromise may lead to the formation of oral-antral or oro-nasal fistula formation or sequestrum formation (Fig. 5.5). The patient may even lose an entire segment of teeth. These soft tissue injuries are best managed very conservatively in the operating room. Raising flaps to close these defects may further compromise the blood supply to the underlying maxillary bone and lead to avascular necrosis. In the postoperative period these communications are best managed conservatively with irrigation and covering the tissues with a noncompressive splint to allow for mucosal healing. Consideration must be given toward adjunctive hyperbaric oxygen therapy to limit the extent and degree of necrosis. Formal closure, if required, may be achieved at a later time with local or distant flaps once vascularization of the maxilla and healing of the bone segments has occurred.
Fig. 5.4. (a) Segmental maxillary osteotomy. (b) Intraoperative dusky appearance of anterior maxillary gingiva indicating vascular compromise. (c) 1-week appearance of necrotic gingival tissues. (d) 1-week appearance of palate without significant vascular compromise. (e) 3-week appearance prior to HBO therapy. (f) 2-month appearance after HBO therapy. Tooth loss and bone grafting is required.

Fig. 5.5. Persistent oronasal fistula following segmental maxillary surgery.

Fixation Issues
Other complications arise when there is either instability from the fixation used in the operating room or inherent problems with dysplastic or hypoplastic bone. Since the most unstable movement of the maxilla is downward and forward simultaneously, rigid fixation, along with bone grafting, may theoretically help increase stability and allow the bone heal.65,66 However, direct bone contact seems to be the key to maintaining stability. This has been reported to be accomplished by modifying the osteotomy design to ensure bone contact. However, the downward movement is limited by the length of vertical cuts made to approximately a total of 6 mm.67
The Downfracture
Downfracture of the maxilla will occur predictably only if the osteotomies are properly executed. The process of downfracturing the maxilla should require minimal force if all osteotomies are complete. Inadequate osteotomies will lead to atypical fracture patterns and can create unfavorable fracture lines that can lead up to the skull base or the orbit (Fig. 5.6).68 These unfavorable fractures may also create tears in the soft tissues and lead to bleeding and hematoma formation within the orbit or posterior maxilla.
Fig. 5.6. (a) Inadvertent maxillary fracture of the palatal shelf during Le Fort osteotomy. (b) Pterygoid plate fracture during Le Fort osteotomy. (c) Pyramidal fracture of maxillary extending to inferior orbital fissure.
If the maxilla is not separated properly, incomplete osteotomies when forced can also create unfavorable fractures across the palatal shelves. Fracture at the junction of the horizontal process of the palatine bone with the palatal process of the maxilla occurs when the plates are not separated. High horizontal fracture of the pyramidal process of the palatine bone occurs when the medial osteotomy is not completed to the pyramidal process. Horizontal fracture of the pterygoid plates with or without separation of the tuberosity is also due to incomplete separation along with a horizontal cut into the plates from the saw or chisels. The palatal shelves remain attached to the pterygoid plates, and it may then be difficult to mobilize, advance, or position the maxilla.
Intraoperative attempts to correct these problems predispose the patient to possible damage to adjacent vascular or neural structures and if not released in the long term, relapse may occur.
Another issue that may arise with improper osteotomy is damage to the nasolacrimal duct as it exits the inferior meatus area causing scarring thus leading to epiphora. The nacolacrimal duct is approximately 11–14 mm posterior to the pyriform rim and 11–17 mm superior to the nasal floor.69–71
Maxillary Mobilization and Positioning
Mobilizing the maxilla and getting it into its final position may also be a challenge if the patient has had multiple surgeries in the past. This would include patients with cleft lip and palate or those with history of trauma. The scar tissues may inhibit the maxilla from anterior or inferior positioning, especially over a large distance. The scar tissue will put strain on the rigid fixation and possibly have a higher potential to relapse. In cases where the maxilla may have to move more than its “biologic soft tissue envelope” will allow, consideration to using tissue expansion with distraction osteogenesis or palatal expansion should be considered.72
Positioning issues arise intraoperatively during the movement of the maxilla in the superior, posterior, or inferior directions. Superior movement must take into account the upper airway structures that may inhibit the required or planned movements. The nasal septum and the inferior turbinate may prevent planned maxillary impaction. These structures in turn may be damaged, torqued, or bent, resulting in aesthetic and functional problems. Obstruction of the opening of the nasolacrimal ducts when manipulating and recontouring tissues in this region may also occur. Posterior positioning issues arise when the bone contact is not relieved either from a thick tuberosity/pterygoid plate region or poorly downfractured Le Fort I, leaving multiple bone interferences.
Intraoperative attention to possible unaesthetic soft tissue changes that may occur from the proposed movements is also important. As the maxilla is moved in any direction, the nasal tip and the nasal apertures will change shape and position. Poor aesthetic results frequently occur from anterior and superior maxillary movement, creating excessive tip rise and widening of the alar bases. Poor nasal function results from septal deviation, changing the nasal valves and thus increasing the potential for obstruction of the airway.73–76 The upper lip will also change shape and shorten after movement of the maxilla and closure of the incisions should be planned to address these alterations. The V to Y closure technique and its modifications is the commonest way of controlling for these changes. Although this may help preventing unaesthetic results, the V to Y closure will also thin the lateral aspects of the upper lip and should be taken into consideration.77
The final position of the maxilla must be verified once it is stabilized.78–80 If the model surgery was accurate, this is accomplished by checking the occlusion and evaluating the patient’s vertical incisor position. To properly hold the maxilla while applying rigid fixation requires special attention. Excess force while rotating the maxillomandibular complex or inappropriate direction of the force can displace the condyles. This will result in an open bite once maxillomandibular fixation is released and will require removal and replacement of fixation. In addition, if the complex does not move smoothly into its new position, either soft tissue or bony interferences exist and should be addressed.
Inability to stabilize the maxilla with current rigid fixation is rare. If stability is not obtained, the osteotomies will heal with fibrous union formation.81 Alternative means of fixation need to be utilized when current bone plating systems cannot be employed effectively. Older techniques of wire suspension and external fixation must not be forgotten as well as the “newer” techniques with intermaxillary fixation screws.
BLEEDING AND HEMORRHAGE
Bleeding is a part of any operation; hemorrhage is not. The causes of hemorrhage from Le Fort I surgery arise from multiple etiologies. Improper use of osteotomes, chisels, the reciprocating saw or retracting instruments can create tears in the vasculature around the osteotomy site.82 Excessive force may lead to poor fractures and possible bone fragments that may create lacerations in blood vessels and bleeding. Previously operated maxillas and patients with traumatic injuries to the midface may be at higher risk for bleeding perioperatively. Patients with unusual skeletal deformities and severe maxillary hypoplasia with anomalous anatomy are also at risk if the altered anatomy is not considered. Decisions as to how alter the approach to the suture line for disjunction must be considered in these special cases, such as directing the osteotomies into the tuberosity region thus avoiding inadvertent injury to the vasculature.83
The blood vessels most likely to be injured during the downfracture process are the lateral and medial pterygoid vessels, the posterior superior alveolar artery, the greater palatine artery, the terminal branches of the maxillary artery, the pterygoid venous plexus, and the internal carotid artery. The internal maxillary artery is normally positioned approximately 23–25 mm superior to the base of the junction of the maxilla with the ptyergoid plates, and its average diameter is 2.5 mm. When appropriately placing a pterygoid osteotome (average 10 mm wide) into the fissure, which is on average 14.5 mm in length, and directing it anteriorly, medially, and inferiorly the vessel can be easily avoided. These average measurements allow for a 10-mm space between the instrument and the vessel. The greater palatine artery is located approximately 20–25 mm posterior to the pyriform rim. It can be avoided by utilizing the measurements usually present on the lateral nasal wall osteotomes and stopping the osteotomies, thus not severing the vessel.
If brisk bleeding does occur, it will most likely originate in order of frequency from the posterior superior alveolar artery, the greater palatine, the pterygoid plexus, pterygoid muscles, or in rare occasions, the terminal branches of the maxillary and/or internal carotid. Completion of the osteotomies and downfracture of the maxilla is required in order to visualize the source and control brisk arterial bleeding.
If the source is identified, ligation with hemoclips (or sutures) is required, especially for the descending palatine artery, as the vessel can retract into the bony canal and become a source of delayed bleeding. Alternatively, bleeding of venous or muscular origin may be controlled with careful use of electrocautery. Packing the wound, using microfibrillar collagen or a similar material, and reassessing may help with establishing a clot, especially in cases of venous origin bleeding or when the source is not easily identifiable. Hypotensive anesthesia can also assist in reducing bleeding and enabling visualization until control is achieved. Ligation of the external carotid artery has not been proven to be a successful way of achieving hemostasis due to collateral circulation in the head and neck. Additionally, there is the risk of injury to adjacent cranial nerves, accidental ligation of the internal carotid or delay in accessing the vessel while brisk bleeding continuous, all associated with serious consequences. By far the most effective means of controlling severe hemorrhage from the high pressure vessels of the head and neck is through interventional radiology and angiographic embolization (Fig. 5.7).84–88
Fig. 5.7. (a) Postoperative persistent ecchymosis and bleeding requiring angiographic diagnosis and embolization. (b) Maxillary artery angiogram showing extravasation prior to embolization.

Nerve Injury During Le Fort Osteotomy
Cranial nerves II, III, IV, V, VI, and VII may all be traumatized by the Le Fort I osteotomy. Essentially, these nerves are found in the pterygomaxillary fissure and the inferior or superior orbital fissure. Most of the nerves mentioned, if injured, will go unnoticed until the postoperative period. However, during surgical manipulation of the maxilla at the time of downfracture, if a decrease in the pulse rate is noted this may be due to the effect of pressure on the cranial nerve V. The trigeminocardiac reflex will cause sudden bradycardia that may be severe and even lead to asystole if not corrected. If sudden bradycardia is noted during manipulation or downfracture of the maxilla, the procedure should be stopped and the jaw returned to its original position until the heart rate returns to normal. Consultation with the anesthesiologists for use of atropine or glycopyrolate in cases of persistent or severe bradycardia may be needed to allow for completion of the procedure. In addition, use of local anesthetic in the soft tissues to decrease the sensitivity of the nerve to manipulation in this area maybe beneficial.87,88
Airway Compromise
Laceration of the endotracheal tube may occur as sharp instruments are being used for the maxillary osteotomies.89–92 If this occurs and adequate ventilation cannot be maintained, the tube must be exchanged. Appropriate measurements are necessary to ensure that this will be done safe and atraumatically. Ideally, bleeding should be controlled first and fiberoptic instruments should be readily available in case difficulties with visualization arise during the process. The surgeon should be prepared to establish a surgical airway should attempts to reintubate or maintain a patent airway fail.93
GENIOPLASTY
Preoperative
The choices of genial augmentation are to use the sliding genioplasty or an alloplastic implant. The aesthetic results desired and amount of bone stock available will dictate the procedure of choice for genial augmentation.94–98
The relationship of the lower lip to soft tissue pogonion in the horizontal plane should be carefully evaluated when treatment planning the correction of the chin position. Advancement beyond the soft tissue envelope tolerance could result in unacceptable aesthetics. The chin may appear too big or even create a “witch’s” chin with a very deep mentolabial groove. Facial balance in the vertical dimension is also important. The height of the lower incisor to menton must be addressed so that the lower facial third is in harmony with the remainder of the face. It is imperative to recognize that occasionally a chin deficit that is due to mandibular position, retrognathia, or apertognathia may be corrected once these deformities are addressed. In cases of inadequate bone stock, an appropriate size alloplastic chin implant should be considered instead.
Perioperative
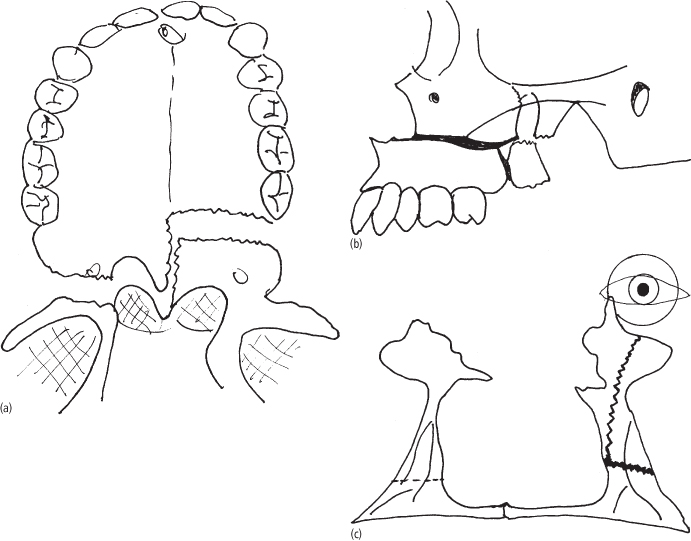
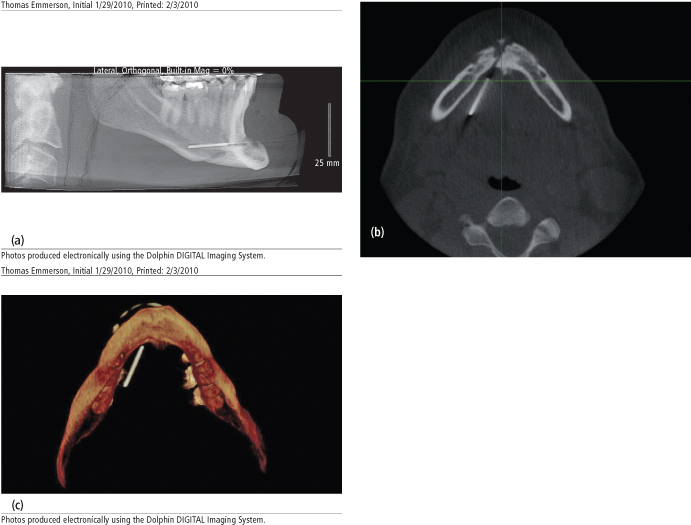
Perioperatively, the most common complication is injury to the mental nerve or of less importance the mylohyoid nerve. Identification of the mental foramen and keeping the osteotomies at least 5–6 mm below the foramen decreases the risk of nerve damage by avoiding the nerve as it loops in the mandible in this region.99 Laceration of the soft tissues and blood vessels in the floor of the mouth is also a possibility, either from the drill or saw used for the osteotomy, or from the hardware used for fixation of the genial segment (Fig. 5.8). This can lead to hematoma formation in the floor of mouth and possible airway compromise. The inability to advance the genial segment, inability to stabilize the genial segment, and inadvertent asymmetrical placement of the segment are also possible complications. Fracture of the mandible can be a potential complication of the genioplasty osteotomy if inadequate bone is maintained superiorly or if sharp angles create weak points. Damage to the teeth is another potential complication, and careful evaluation of the root lengths in preoperative radiographs is essential.
Fig. 5.8. (a) Lateral cephalograph showing overpenetration of genioplasty pins. (b) CT scan showing genioplasty pins beyond the lingual plate of the mandible. (c) 3D CT showing genioplasty pin overpenetration into the floor of the mouth.
Postoperative
Postoperative complications are related to wound healing issues at the incision site, instability of the segments and hardware failure, infection, numbness of the lower lip and unaesthetic result due to poor positioning.100–102 Necrosis of the genial segment “wings” with formation of deep depressions at the junction with the native mandible distally can occur. This is usually the result of poorly planned and executed osteotomies with inadequate bone stock. Finally, improper handling of the soft tissues and failure to approximate the mentalis muscle will cause lip ptosis.
MANDIBLE: INTRAOPERATIVE COMPLICATIONS
Whereas the work horse of the maxilla is the Le Fort I osteotomy, the mandible can be moved into position with many different types of osteotomy designs. These include the vertical ramus osteotomy, sagittal split ramus osteotomy, inverted L osteotomies, midline osteotomies, and various anterior segmental osteotomies. Choices depend upon bone stock, movement required, effect on the temporomandibular joint, and anatomic vital structures. The various complications associated with these osteotomies vary from poor osteotomy design to vascular and neural issues to wound healing problems.103
INTRAORAL VERTICAL RAMUS OSTEOTOMY (IVRO)
Complications with intraoral vertical ramus osteotomies arise when this procedure is employed for mandibular advancement or lengthening of posterior facial height. Bone healing, without grafting, at the osteotomy site is not possible due to lack of bony contact between the proximal and distal segments. The pterygomasseteric sling will interfere with planned movements, especially in cases of advancement, even if the muscles are stripped from the mandible. Stable occlusion may not be possible and will result in an anterior open bite once maxillomandibular fixation is released.
The intraoral vertical ramus osteotomy is performed under limited visibility and special instrumentation is designed to assist in overcoming this problem.104–109 Special retractors that engage the posterior border of the mandible, the sigmoid, and the antegonial notch can be utilized to improve exposure. In addition, the instruments can accommodate fiberoptic cables and thus improve visibility in the field.
Trauma to the tissues, however, such as laceration of periosteum and risk of injury to surrounding vessels, is possible from inappropriate or careless use of these retractors. The masseteric vessels in the sigmoid notch, the facial vessels in the antegonial notch, and the retromandibular vein at the posterior border are at risk from the misuse of the instruments. Furthermore, these vessels are at risk from the micro-oscillating saw during the osteotomy if not appropriately protected.
Appropriate positioning of the osteotomy at the ramus is essential to avoid injury to the inferior alveolar neurovascular bundle while ensuring that the proximal segment is of appropriate size to avoid condylar sag. The micro-oscillating saw blade specially designed for execution of the IVRO osteotomy is available in two lengths: short and long. Using the appropriate size blade based on the width of the ramus is essential to avoid injury to the lingual tissues or create incomplete osteotomies. It is essential when performing the osteotomy to avoid excess force that may cause breakage of the saw blade. The blade is difficult to retrieve from the medial surface of the mandible once it is lost in the cut. Endoscopic surgical techniques to better visualize the osteotomy during this procedure have been described. In addition, with the endoscopic ap/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


