CHAPTER 5 Oral Disease
Introduction
Plaque is a film containing bacteria (a biofilm) that builds up rapidly and is usually removed by toothbrushing and other mechanical oral hygiene aids. If plaque is not removed it eventually hardens into calculus because of the deposition of calcium salts. Chemicals in certain mouthwashes and toothpastes can inhibit the build up of plaque, and some inhibit calculus (tartar) formation. These oral healthcare products are discussed in Chapter 8.
Diseases of the teeth
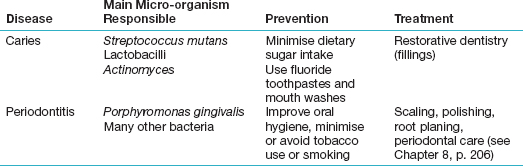
Table 5.1 shows the main dental diseases.
Dental Caries (Tooth Decay)
Dental caries is a very common disease. The main plaque micro-organism that causes dental caries is the bacterium Streptococcus mutans (also called viridans streptococci). Other bacteria such as Lactobacillus and Actinomyces may also play a role. The bacteria act by converting the sugars in the diet to acids (especially lactic acid). The acids destroy (decalcify) the enamel and dentine of the teeth (Figure 5.1).
The non-milk sugars include the common table or cane sugar (sucrose), glucose, and fruit sugar (fructose). Sugars are also added to many foods and drinks, in particular to refined carbohydrates such as starch and foods such as cakes and biscuits. Non-milk sugars (Table 5.2) are the most cariogenic. Dietary starch is also broken down slowly by salivary enzymes to glucose and maltose. Concentrated fruit juices and dried fruits also have a high concentration of sugars such as fructose and are therefore also cariogenic. Fresh fruits and vegetables are not cariogenic.
| Pure Sugars | Mixtures |
|---|---|
| Dextrose | Brown sugar |
| Fructose (except in fresh fruits and vegetables) | Golden syrup |
| Glucose | Honey |
| Hydrolysed starch | Maple syrup |
| Invert sugar | Treacle |
| Maltose | |
| Sucrose |
Caries prevention
The caries disease process
The least tooth damage is done by:
Table 5.3 summarises the key points you need to know about dental caries.
| Cause | Plaque bacteria, especially Streptococcus mutans, which acts on sugars to produce lactic acid, which decalcifies (demineralises) the teeth |
| Plaque | This biofilm tends to form in pits and fissures, interproximally at contact areas; and at the cervical margins (sites where caries begins) |
| Main sugars implicated in caries | Sucrose, glucose |
| Sugars and sweeteners rarely implicated in caries | Fructose, lactose, sorbitol, aspartame |
| Acidity (critical pH) below which enamel decalcification occurs | 5.5 |
| Methods of detection | Visual examination |
| Bitewing radiographs (see Chapter 14) | |
| Transillumination (shining a light through the tooth) | |
| Electronic caries detectors | |
| Using a probe (but this may cause further damage; see Chapter 7) | |
| Preventive measures | Consuming less sugars in the diet |
| Using fluorides, e.g. fluoridated toothpastes | |
| Using amorphous calcium phosphate |
If caries is not treated
If the carious process is allowed to progress, it destroys the enamel, causing a cavity to form in the tooth. Eventually it reaches the dentine. Once caries reaches the dentine, the carious process speeds up. Also, the patient may feel pain on stimulation with sweet/sour or hot/cold. This pain is similar to the pain that occurs when dentine is exposed due to loss of enamel for other reasons such as trauma, erosion or abrasion (see p. 141). The pain subsides within seconds of removing the stimulus. The pain may be poorly ‘localised’, that is, it may be difficult for the patient to say where exactly it is. Often pain is localised only to an approximate area within two to three teeth of the affected tooth.
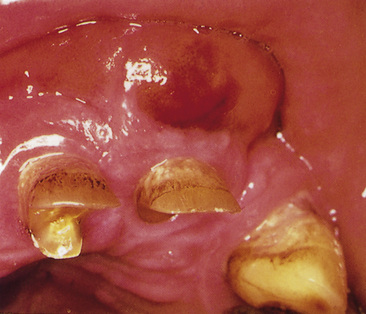
The inflammation causes swelling of the pulp but, since the pulp is confined within the rigid pulp chamber, the pressure builds up. Thus there is severe and persistent pain in the tooth. The swelling also stops the blood flow into the pulp – which then dies. The pain may then subside for a while. However, the dead pulp is infected with bacteria from the mouth. So the infection can then spread through the tooth root apex and cause apical periodontitis. This is very painful, especially when the tooth is touched or the patient bites on it. Such a tooth must be root treated (endodontics) or extracted (exodontics) in a timely fashion. Otherwise a dental abscess (Figure 5.1B), granuloma or cyst (see below) will eventually form.
Periapical Abscess (Dental Abscess)
A dental abscess often follows pulpitis caused by caries or trauma. The pulp, and so the affected tooth, is dead (non-vital). Therefore although the tooth cannot itself cause pain, the inflammation travels to the bone surrounding the tooth apex. This is called apical periodontitis. If the inflammation persists, it may cause an abscess (apical or dental abscess) both of which produce pain. A dental abscess will cause pain and also result in a swelling, typically in the labial or buccal gingiva (Figure 5.2). Sometimes the face can swell up too (Figure 5.3) and the patient may also develop lymph node swelling and a fever.
If the tooth is not correctly treated, a cyst (periapical, radicular or dental cyst) can develop. Again, either root canal treatment or root end surgery (apicoectomy or apicectomy) will then be needed (see Chapter 9).
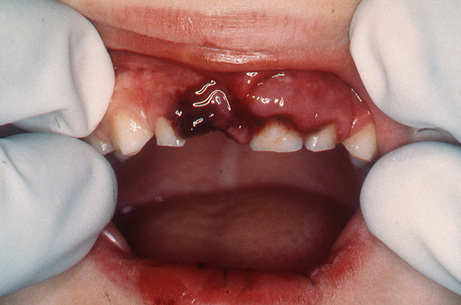
Trauma
Trauma to the teeth is commonly seen in sports, road accidents, violence, epilepsy, and in restorative dentistry! Tooth trauma is seen mainly in boys or young men. It usually affects the maxillary incisors. Because of the impact of trauma, a tooth can be lost from the mouth or dislodged within its socket (Figure 5.4), fractured (the crown or root), or it can die. (See also Chapter 16). Dental trauma is also seen in children who have been abused. In all forms of trauma, there can also be damage to the jaws or soft tissues. Thus it is important for the clinician to take a careful history and do a thorough examination to ensure there are no injuries elsewhere in the body, especially head or chest injuries (which can be fatal), or damage to the neck – which can lead to paralysis or death.
Attrition
Attrition is a form of tooth surface loss. It is the wearing away of a tooth’s biting (occlusal) surfaces due to chewing (mastication). It is most obvious in people who have a coarse diet. Attrition can also occur in people with a habit such as bruxism (grinding of teeth). The incisal edges of the anterior teeth and the cusps on the occlusal surfaces of the premolars and molars wear down. Once the enamel is breached, the softer dentine is lost faster than the enamel, which results into a flat or hollowed surface (Figure 5.5). The tooth may need a restoration (see Chapter 9).
Abrasion
Abrasion is another form of tooth surface loss – the wearing away of the hard tissues at the neck of the tooth by a habit such as toothbrushing with a hard brush and coarse toothpaste. The gingiva recedes but is otherwise healthy. The cementum and dentine wear down but the harder enamel survives, resulting in a notch (Figure 5.6). The exposure of dentine also means the tooth may become sensitive to hot and cold. There may also eventually be tooth fracture. The tooth may need a restoration (see Chapter 9). Use of desensitising toothpastes and fluoride application may also help.
Erosion
Erosion is tooth surface loss caused by dissolution of the tooth minerals by acids other than those produced in caries. Fruits or fruit drinks, cola (and other carbonated drinks) and stomach (gastric) acid are the main causes of erosion. In most patients there is little more than a loss of normal enamel contour but, in more severe cases, dentine or pulp may be involved. Patients who have a habit that causes erosion should be counselled to stop the habit. The teeth may need to be restored (see Chapter 9).
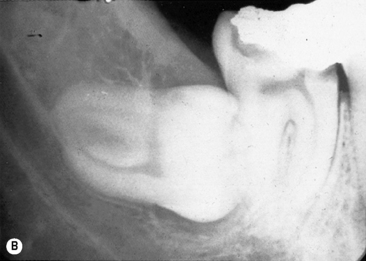
Impacted Teeth
Teeth can fail to erupt fully because of insufficient space in the dental arch. The teeth most commonly affected are the third molars (wisdom teeth, lower third molars most common), second premolars and canines (Figure 5.7).
Variations in Tooth Number
Hyperdontia (too many teeth)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses