CHAPTER 2 Medical Emergencies and First Aid in the Dental Surgery
Introduction
A medical emergency is an injury or illness that poses an immediate threat to a person’s life or long-term health. Box 2.1 lists the warning signs of a medical emergency that you may encounter as a dental nurse.
Risk assessment
Healthcare aims to improve the health of patients but can itself carry risks, so the first principle must be to do no harm (‘primum non nocere’ – from the Latin). Dentists and dental nurses can be involved in using local anaesthesia (LA) and conscious sedation, procedures that are safer than general anaesthesia (GA), which is now only carried out in hospitals with critical care facilities. Most dental procedures are safe, although surgical procedures may be less safe. Patients with medical problems are generally more likely to have complications, including emergencies, than are healthy individuals. Thus a non-invasive procedure such as applying a fissure sealant on a healthy child, is likely to be far safer than, for example, a surgical operation in an older person with a heart by-pass who is being treated with anticoagulants (Box 2.2).
The taking of a medical history aims to elicit such risks, following which steps are then taken to reduce the risks (Table 2.1).
| Risks Increased by | Risks Reduced by |
|---|---|
| Increasing age | Planning treatment properly |
| Medical treatments | Non-invasive procedures |
| Surgical treatments | Monitoring |
| Lengthy dental procedures | Reassurance |
| Drug use – medication or recreational |
Medical history
The relevance of many common medical conditions is discussed in Chapter 17. An easy to recall alphabetical list for the RMH is shown in Table 2.2.
| Condition | Relevance in Dentistry |
|---|---|
| Allergies | These range in severity from a localised rash to collapse from anaphylaxis. Common allergies are to LIED (see p. 7). Anaesthetics, analgesics (e.g. aspirin or codeine) and antibiotics (e.g. penicillin) and latex are the main offending agents |
| Bleeding disorders | Bleeding and/or bruising are a significant hazard to any surgery |
| Cardio-respiratory disorders | Wheezing, cough, shortness of breath (dyspnoea), chest pain, swelling of ankles, palpitations, hypertension may be a contraindication to GA or conscious sedation |
| Drug treatment | Drug use may be the only indication of serious underlying disease. Treatment will need to be deferred until the drugs are identified. |
| Most serious interactions with drugs or herbal medicines are with GA or conscious sedation agents. | |
| Aspirin and other similar drugs may be a hazard in anticoagulated, asthmatic, diabetic or pregnant patients, those with peptic ulcers, or children under 16 years. | |
| Recreational drugs may cause behavioural problems. | |
| Endocrine disorders | Diabetes mellitus may lead to collapse. Hypoglycaemia (low blood sugar) is the main problem |
| Fits or faints | Fainting and epilepsy may result in injury to the patient |
| Gastro-intestinal disorders | Crohn’s disease or coeliac disease may have oral complications such as ulceration, and gastric disorders may increase the risk of vomiting during GA or conscious sedation |
| Hospital admissions and attendances | Hospital admissions may indicate presence of a disease |
| A history of operations may provide knowledge of possible reactions to GA, sedation and surgery | |
| Operations on the retina (part of the eye) may use intraocular gases and such history would be a contraindication to GA or conscious sedation, which may cause rapid expansion of the ocular gas, leading to blindness | |
| Infections | The transmissibility of infections must be considered. People who have attended a clinic for sexually transmitted infections (STI), or been admitted to hospital for an infection, or who have been refused for blood donation may be at risk. Carriers of meticillin-resistant Staphylococcus aureus (MRSA), tuberculosis, or of Neisseria meningitidis may be a particular hazard to others |
| Jaundice and liver disorders | A history of jaundice or other liver disease may mean the patient is prone to prolonged bleeding or impaired drug metabolism, and may imply carriage of hepatitis viruses |
| Kidney and genitourinary disorders | Excretion of some drugs may be impaired. Tetracyclines should be avoided or given in lower doses |
| Likelihood of pregnancy | Any essential procedures involving drugs (even aspirin), elective operative dentistry (restorative or surgical), radiography or GA should be arranged during the middle trimester |
| Mental state | Anxiety is common before dental treatment. Anxious patients may sometimes react aggressively, and anxiety may limit extent of dental treatment that can be provided under LA |
| Neurological | Movement disorders can significantly disrupt operative procedures |
Managing a medical emergency
Role of the dental nurse in a medical emergency
According to the General Dental Council (p. 71), dental nurses should be:
The emergency kit
The emergency kit should consist of the equipment and drugs listed in Table 2.3. Where possible all emergency equipment should be meant for single use only and latex-free to avoid allergies. Note that the recommended kit includes only drugs meant for injecting into the muscles (intramuscular, short form: IM) and not into veins (intravenous, short form: IV).
TABLE 2.3 Suggested Minimal Equipment and Drugs for Emergency Use in Dentistry
| Equipment | Comments |
|---|---|
| Portable apparatus for administering oxygen | Portable oxygen cylinder (D size) with pressure reduction valve and flow meter. The cylinder should be of sufficient size to be easily portable and also to allow for adequate flow rates, e.g. 10 litres per minute, until the arrival of an ambulance or the patient fully recovers. A full D size cylinder contains 340 litres of oxygen and should allow a flow rate of 10 litres per minute for up to 30 minutes. Two such cylinders may be necessary to ensure oxygen supply does not fail |
| Oxygen face mask with tube | |
| Basic set of oropharyngeal airways (sizes 1, 2, 3 and 4) | |
| Pocket mask with oxygen port | |
| Self-inflating bag valve mask (1 litre size bag) for use by staff who have been appropriately trained | |
| Variety of well-fitting adult and child face masks for attaching to self-inflating bag | |
| Portable suction | Portable suction with appropriate suction catheters and tubing, e.g. the Yankauer sucker |
| Spacer device for inhalation of bronchodilators | |
| Automated external defibrillator (AED) | |
| Automated blood glucose measuring device | |
| Equipment for administering drugs intramuscularly | Single-use sterile syringes (2 ml and 10 ml sizes) and needles (19 and 21 gauge) |
| Drugs as below | |
| Emergency | Drugs Required (Dosage Given is for Adults) |
| Anaphylaxis | Intramuscular adrenaline (0.5 ml of 1 in 1000 solution; repeat at five minutes if needed) |
| Hypoglycaemia | Oral glucose solution/tablets/gel/powder (proprietary non-diet drink or 5 g glucose powder dissolved in water) – for example, GlucoGel, formerly known as Hypostop gel (40% dextrose) |
| Glucagon injection (intramuscular 1 mg) – for example, GlucoGel, GlucaGen, HypoKit | |
| Acute exacerbation of asthma | Beta 2 agonist – for example salbutamol aerosol inhaler (100 micrograms/activation, activations directly or up to six into a spacer) |
| Status epilepticus | Midazolam (10 mg) (buccal or intranasal use) |
| Angina | Glyceryl trinitrate (GTN)* (two sprays of 400 micrograms/metered activation) |
| Myocardial infarction | Dispersible aspirin (300 mg chewed) |
No corticosteroid is included.
Other agents (e.g. flumazenil) and equipment (e.g. pulse oximeter) are needed if conscious sedation is administered in the surgery.
* Do not use nitrates to relieve an angina attack if the patient has recently taken sildenafil (e.g. Viagra or Cialis) as there may be an abrupt fall in blood pressure; analgesics should be used.
This is because IM injections are generally easier and safer to give. IM injections are best given into the side of the thigh.
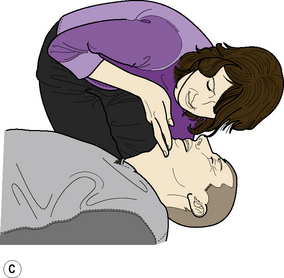
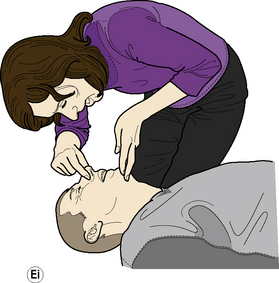
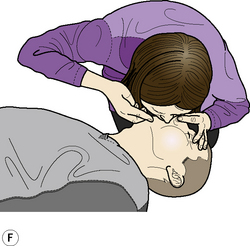
Basic life support
In the UK, the Resuscitation Council is responsible for providing guidelines for how to carry out CPR. The BLS sequence described below is based on the UK Resuscitation Council Resuscitation Guidelines (2005). Box 2.3 provides an aide mémoire for adult BLS.
As a dental nurse you should be aware of the most up-to-date guidelines issued by the Resuscitation Council. You can find these at the council’s website (http://www.resus.org.uk).
Adult BLS Sequence (Figure 2.1)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses