Chapter 5
Optimizing Dental Implant Aesthetics
Since the commercialization of dental implants over 30 years ago, implants have become a popular and predictable way to restore partial or complete edentulism. In the early development and use of implants, however, more focus was placed on functional restoration rather than the esthetic results. With the advancement of the science of dental implantology, it is now possible to restore patients to optimal aesthetic and functional results. The cosmetic outcome of an implant restoration is a cumulative result of three distinct phases of the implant process: recognizing the aesthetic deficiency or preserving the current norm; correcting the preexisting aesthetic deficiency; and adjusting of gingival contours. These areas will be explored in detail.
The treatment planning phase of implant aesthetics is clearly the most important part of the care to be rendered. The ability of a clinician to diagnose and recognize potential problems and decrease their possibility of occurrence, or at the least prepare the patient for their existence, usually results in a better outcome for patient and doctor. In treatment planning for dental implants, there are three main areas to evaluate for aesthetic and functional deficiencies: the bony ridge height and width; gingival contour and aesthetics; and pathological and anatomical variations. These factors will guide the implant insertion process and possible need for enhancement.
Several methods for classifying the edentulous area have been described.1–4 One such system, described by Kent et al., describes the edentulous ridge by shape and the amount of hydroxyapatite (HA) graft material needed to correct the deficiency. Type I deficiencies have adequate height but inadequate width that usually present with lateral defects or undercut areas and that require 2–4 g of HA to correct. Type II abnormalities display deficiencies in both height and width and have a knife-edge appearance requiring 3–5 g of HA to reconstruct. Type III deficiencies display moderate to severe resorption with preservation of basilar bone and require 6–10 g of HA with or without autogenous supplementation. Finally, Class IV edentulous ridges display resorption of the basilar bone producing a pencil-thin, flat mandible or maxilla that require autogenous grafting to fully restore to adequate dimensions.1,2
Branemark denotes a system of whole jaw resorption that is less descriptive, ranging from “minimal” resorption in Class I cases to “extreme” resorption in Class V.3 There is also a commonly used classification by Jensen that describes the residual bone in both quantity and quality as well as proximity to vital structures.4 In this classification, Class I through IV is based on the typical amount of bone available, and its quality of use. Typically, the posterior maxilla is labeled as Type IV bone due to its poor quality and proximity to the maxillary sinus.
Whichever system is used, it is important to note the amount of ridge resorption and inform the patient of the possible need for bone grafting during or prior to the implant surgery.
In addition to looking at the ridge form, an evaluation of the gingival form and adjacent teeth must also be made to ensure acceptable esthetic outcomes. The patient must be evaluated for the height of the lip line at smile and at rest, the amount of keratinized gingiva, the amount of gingival recession on adjacent teeth, and the height of the adjacent dental papilla. Diagnostic wax-ups can be used to evaluate tooth length and the potential for vertical grafting to avoid the overly long restoration. Placement of implants into areas with diminished ridge height as well as minimal keratinized gingiva will lead to excessive crown lengths and poor esthetic results, especially when the patient smiles.
Papilla regeneration is determined by the distance from the contact point of the restoration to the residual interproximal alveolar bone. If that gap is kept to within 5 mm, the papilla can be expected to regenerate.5 If that interval is extended to 6 or 7 mm, the papilla only regenerates in 56% and 27% of cases, respectively.
Keratinized gingiva can also be expected to regenerate from surrounding areas of attached gingiva. In addition, this gum tissue can be reconstructed using grafting procedures or guided tissue regeneration (GTR) to optimize the esthetic outcome.
The gingival esthetic evaluation must be three-dimensional since inadequate bulk of soft tissue in certain areas may hinder the desired cosmetic result. For example, if adequate bone quantity exists for the placement of a dental implant in the maxillary canine region, the canine prominence may be reconstructed with soft tissue procedures rather than via bone grafting to achieve a more pleasing esthetic conclusion.
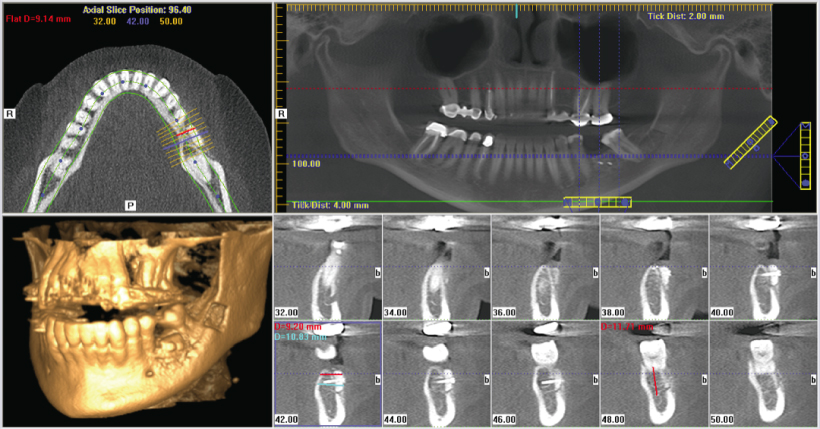
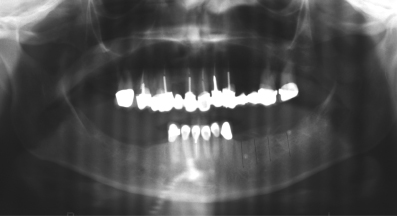
Radiographic evaluation for planned implant placement is part of thorough treatment planning for esthetic outcomes. The presence of anatomical variations such as a bony undercut or narrow alveolar ridge can be identified via computed tomography or classic tomograms.
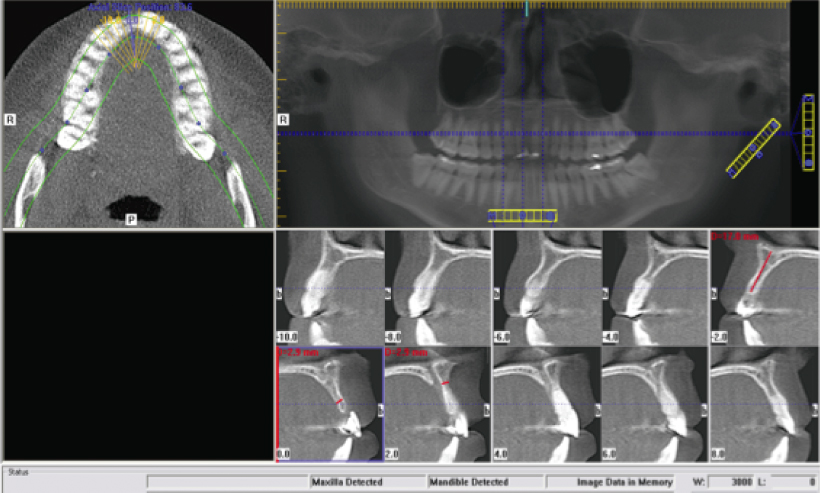
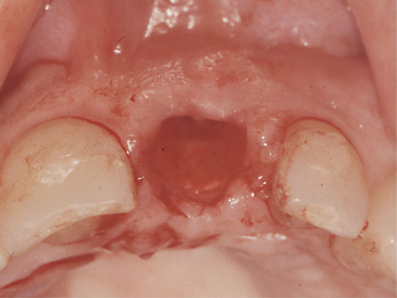
Lateral cephalometric evaluation may help guide esthetic outcomes in patients with skeletal abnormalities and a need to restore functional occlusion. In fact, it may be necessary in these cases to create a more normal skeletal relationship prior to the placement of dental implants. The majority of these cases can still be diagnosed and treatment planned with the standard panoramic and periapical radiographs. Computed tomography scanning and the advent of in-office cone beam computed tomography technology, in particular, have increased the use of tomography for routine evaluations for dental implants (Figure 5.1). The radiographic modality of choice at this time is based on physician preference. However, it should be noted that all X-ray examinations should follow the ALARA (as low as reasonably achievable) principle for diagnosis and treatment planning. Patients should undergo a thorough clinical examination to determine the appropriate diagnostic radiograph for each situation.6 Once the patient has been thoroughly evaluated, the treatment options should be explained to the patient. There are two broad categories of implant surgeries: immediate placement at the time of tooth extraction, and delayed placement. Each treatment option has its own basic algorithm to use as a guide. With the immediate placement at the time of extraction, the area should be free of infection and surrounding pathology with adequate residual bone for implant stability. It is important to inform the patient that it may be necessary to convert to the delayed placement option if either of these criteria cannot be met. The majority of immediate placement cases will require some amount of bone grafting with or without GTR. Ideally, immediate placement should be considered when the level of the surrounding alveolar bone would allow for esthetic implant positioning and restoration. If extensive grafting procedures are required, the delayed placement option will usually result in a more esthetic outcome.7 If the tooth has existing pathology, an esthetic deficiency, or was previously removed, insertion of the implant follows a distinct pattern. If extensive grafting or tissue regeneration is required, a staged approach is appropriate. Correction of the underlying deficiency will allow for easier implant placement and control of aesthetics. If minimal or no grafting is necessary, the implant may be placed in a one-stage procedure and may be immediately restored if primary stability can be obtained.8–10 If bony wall defects are present at the time of extraction, or if the patient is considering implants but has not committed to implant therapy, bone grafting at the time of extraction may aid in future implant placement and enhance restorative aesthetics. The so-called socket preservation graft allows for decreased bone resorption after extractions, which in turn allows maintenance of alveolar bone levels and minimizes height and width discrepancies, resulting in more cosmetic implant crowns.11–13 Once a soft or hard tissue deficiency has been identified, the method of correction must be chosen. Three methods currently exist: bone grafting, GTR, and soft tissue grafting. A discussion of bone grafting procedures must begin with the materials available for use. The major categories consist of autogenous bone, allografts, alloplasts, xenografts, and chemically mediated grafts (bone morphogenetic protein or BMP). Autogenous grafting continues to be the gold standard for bone graft harvest and several sites have been used successfully in conjunction with the placement of dental implants. Iliac crest and cranial bone grafts are generally reserved for cases where large amounts of osseous material is required or in situations where other harvest sites have proved inadequate. Tibial cancellous marrow can be used for intermediate levels of bone grafting such as unilateral sinus lifts and ridge augmentation. Intraoral graft sites such as the maxillary tuberosities and the rami and genial tubercles of the mandible have become common sources of autogenous grafting in implant surgery.14–16 Utilizing autogenous bone provides living cells and minimizes the risk of foreign body reactions and infections.
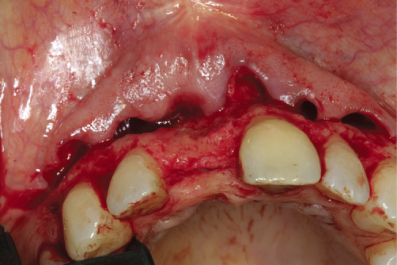
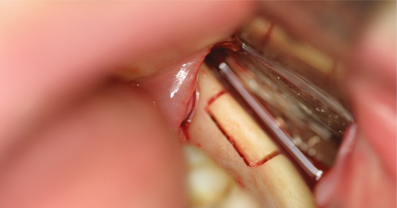
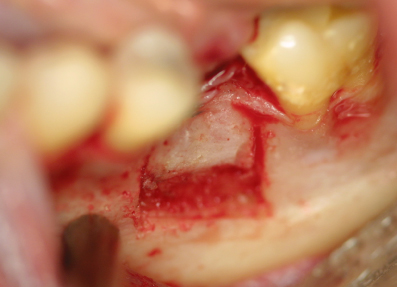
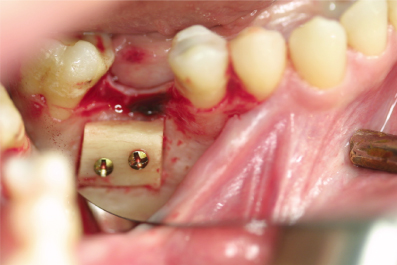
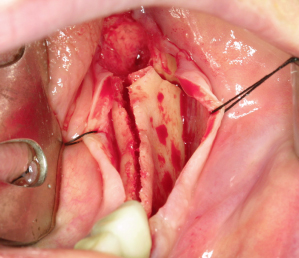
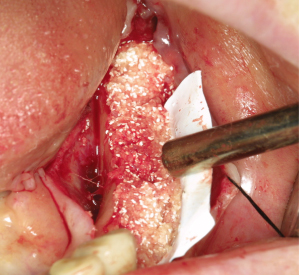
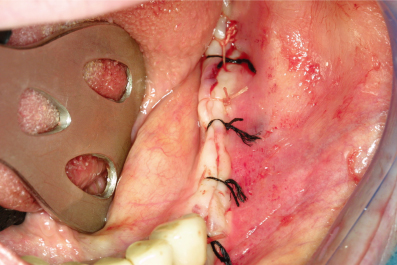
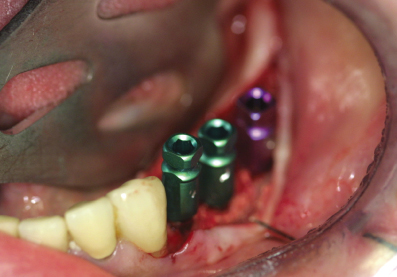
Many companies now exist with the ability to supply allograft and xenograft bone material to be used with dental implants. The material is produced in many forms including block and particulate grafts, as well as putty emulsions. They range from irradiated human bone to bovine bone matrix. Some grafting materials are not bone at all but a resorbable matrix to aid in de novo bone formation by acting as a scaffold for autogenous bone growth. Materials such as beta-tricalcium phosphate and HA have been used with good success.1,2,17 They may be used alone or in combination with autogenous bone. The newest advancement in bone grafting has been the commercial availability of recombinant human bone morphogenetic protein (rhBMP) that is manufactured utilizing genetic engineering of ovary cell lines to create human BMP-2. It is then lyophilized into powder form and reconstituted at the time of surgery and spread on a bovine collagen carrier. The collagen carrier then serves as the delivery mechanism so that osseoinduction occurs only in the area of intended placement of the rhBMP. It is currently approved for use during sinus lift grafts and socket preservation grafts and is in trial for use in general maxillofacial bone grafting.18 Each grafting material has its own set of indications, advantages, and disadvantages. The techniques common to surgery aimed at enhancing and maintaining the aesthetics of an implant site include block, sandwich, and particulate bone grafting as well as alveolar ridge splitting. Autogenous block grafts may be harvested from the iliac crest, calvarium, mandibular ramus, and chin regions. In addition, allograft and alloplast block materials are available for use. The technique for block graft recipient application involves elevation of a flap with or without releasing incisions and subperisoteal dissection. Once the area of deficiency has been thoroughly exposed, a template may be created and the block graft carved to match the deficient space in three dimensions (Figures 5.2–5.7). The graft material is then secured in position with a minimum of two miniscrews or bone tacks to prevent movement of the graft. Particulate graft material may then be packed around the block graft and the gingiva is closed primarily in a tension-free fashion with 3-0 or 4-0 silk or nylon sutures. The graft is allowed to consolidate for 4–9 months prior to implant placement and the screws may be removed at the time of surgery. Block grafting can be used to increase both width- and height-deficient alveolar ridges to improve the esthetic outcome.19 Vestibuloplasty or other soft tissue procedures is often required to supplement extensive or large block grafts. Advantages of block grafting include the fixation and precision of the graft to the recipient site and ease of use for large defects. Disadvantages include increased integration time, possible need for additional soft tissue procedures, and donor site harvest complications. Ridge split techniques can be utilized for deficiencies of width with a minimum of 3 mm of residual ridge. The ridge split technique or “book flap” can be used to place dental implants or may be used in combination with a sandwich graft technique to increase both width and height of the residual alveolus. The ridge split technique described is a composite of available techniques used by the authors.20–22 The initial exposure is made with bilateral releasing incisions beveled away from the alveolar ridge, if grafting to increase alveolar height in the coronal direction is planned, and a subperisoteal dissection is performed exposing the deficient ridge. A thin disk, bur, piezo-knife, saw, or osteotome is then used to score the narrow ridge through the middle of the deficiency. This is followed by vertical scoring of the buccal or labial plate to allow for outfracture of the ridge to increase its width. A thin spatula osteotome is then used to start the widening procedure by displacing the facial bone laterally. The technique can be modified if immediate implant placement is desired by making a crestal incision only, avoiding stripping the periosteum, and blind osteotomies and outfracture of the buccal plate, which remains attached to the blood supply of the periosteum. If the ridge is sufficiently wide for implant placement and the buccal plate remains intact, the implant sites are then prepared for implant placement utilizing the osteotome technique or traditional rotary implant drills. Implants are then seated and the ridge dehiscence is grafted with particulate material and the site closed primarily or with membrane application (Figures 5.8–5.12). If the buccal plate fractures at the time of attempted ridge split or vertical augmentation is also required, a cortical graft harvested from the posterior ramus or mental region may be inserted into the dehiscence and either secured with a lag screw or left in position if stable.
Particulate graft material may also be used to fill the bony separation to augment the width of the residual ridge in a “sandwich” graft technique, and may be used to fill out the cortical graft’s vertical augmentation. Advantages to this technique are the possibility for implant placement at the time of ridge split grafting, decreased healing time, and potential lack of need for donor site harves/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses