5
Maxillary Central Incisors
Aetiology
Diagnosis
Treatment timing
Attitudes to treatment
Treatment of impacted central incisors
Prognosis
Aetiology
At the age of about 6 years, in most children, a sudden and dramatic change occurs in the anterior part of the dentition, with the shedding of the deciduous incisor teeth and the appearance of the permanent incisor teeth. As has been described in Chapter 1, the first to erupt in the young child are usually the mandibular central incisors, although the first permanent molars may sometimes precede them. The mandibular lateral and the maxillary central incisors then erupt shortly after, at 6.5–7 years. Under normal circumstances, the maxillary lateral incisors are the last of the incisors to erupt, completing the anterior dentition with their appearance about a year after the eruption of the adjacent central incisors. Further changes in the dentition, in terms of shedding of deciduous teeth and eruption of their permanent successors, do not occur until approximately the age of 9.5–10 years. This means that there is a two-year period of relative stability, which is known as the mixed dentition stage.
The spectacle of erupted lateral incisors associated with the non-appearance of one or both of the central incisors should always be deemed abnormal, whether or not a deciduous central incisor is still present, and further investigation should be undertaken to ascertain the reason for the aberration.
Congenital absence of a maxillary permanent central incisor, given the presence of permanent lateral incisors, is exceptionally rare, although it has been reported. In this situation, the shape of the single central incisor makes it impossible to distinguish whether it belongs to the right or left side. The patient’s appearance is abnormal (Figure 5.1a–c) and rather reminiscent of a ‘dental cyclops’! However, the abnormality in the appearance is also due to other clinical features and malformation of other elements of the craniofacial complex. The patients have other midline anomalies, including an indistinct philtrum of the upper lip, with an absence of the typical Cupid’s bow and no midline frenulum, a mid-palatal ridge, and nasal obstruction or septum deviation. They exhibit a short anterior cranial base and maxilla, together with retrognathic and posteriorly inclined maxilla and mandible. The sella turcica also has an abnormal shape. Accordingly, the condition should not be treated as a simple, local and isolated congenital absence, as would be the case in relation to a missing maxillary lateral incisor or mandibular second premolar. This patient exhibits a mild form of holoprosencephaly (Figure 5.1).
Fig. 5.1 (a) Abnormal lip morphology, absence of philtrum and midline position of single central incisor, in a case of holoprosencephaly. (b) Intra-oral view of same patient to show ‘square’ anatomy of incisor and indeterminate right/left designation. The lateral incisors are laterally flared as part of an otherwise normal ‘ugly duckling’ stage of development. (c) A view of the palate to show bilateral submucous clefting.
(Courtesy of Dr S. Geron.)

At 5–6 weeks of human embryonic development, the forebrain is formed and the face begins to take shape. In holoprosencephaly, the forebrain fails to develop into two cerebral hemispheres and the structures that are normally paired into identical right and left units are allowed to merge. This causes defects in the development of the face and in brain structure and function which, in less severe cases, may result in normal or near-normal brain development and facial deformities that may affect the eyes, nose and upper lip. However, in most cases of holoprosencephaly, the malformations are so severe that the foetus dies in utero [1].
Trauma to the anterior maxilla in a young patient is probably an almost daily occurrence in many schools, playgrounds and sports activities. Trauma at home should not be forgotten and may occasionally be the first clue of child abuse. By and large, the incidents are trivial and characterized by much bleeding from lacerations of the lip and gingivae which may occasionally divert attention from underlying damage to the incisor teeth. These may have been traumatically intruded and lost from sight or even completely avulsed.
A careful history should be elicited to eliminate the remote possibility of avulsion of the permanent central incisor which may have been completely overlooked. This may happen if the tooth had been in the very earliest stages of its eruption and, therefore, its absence went unnoticed at the time. A newly erupting central incisor is invested with a rudimentary, underdeveloped periodontal ligament (PDL) such that a relatively light and unfortunately well-directed blow may easily bring about its loss.
Obstructive Causes
Supernumerary Teeth
When an existing permanent central incisor does not erupt and the diagnosis of impaction is made, the most common aetiological factor is the presence of one or more midline supernumerary teeth [2–4] (see Figures 1.10 and 1.11). In a study of a sample of schoolchildren [5] the prevalence of supernumerary teeth was found to be between 1.5% and 3.5%. It has also been shown in a different sample group [6] that between 28% and 60% of cases with supernumerary teeth will have resultant eruption disturbances of the adjacent teeth. By arbitrarily integrating these two studies and assuming that they represented random samples of patients attending a children’s hospital dental department, it would seem that between 0.42% and 2.1% of child dental patients suffer from impacted central incisor teeth from this cause. For the most part, supernumerary teeth develop on the palatal side of the permanent incisors and as such occupy space within the narrow alveolar ridge. This results in a labial and superior displacement of the permanent incisors, which includes their roots.
Odontome
Among the other and rarer causes of obstruction, which may equally prevent the eruption of a normal central incisor, are odontomes. These are very variable in size and type, but, whether they are of the complex or the composite type, they usually have a broader and wider cross-section and their presence will be more likely to impede the eruption of an incisor than a supernumerary tooth.
Ectopic Position of the Tooth Bud
The development of a tooth bud in an abnormal position or in an abnormal angulation may have no apparent cause and may thus be attributed to traumatic or genetic factors (Figure 5.2). As a result of the displacement, normally placed adjacent teeth may provide the physical obstacle to the normal eruption of such a tooth. Alternatively, other physical obstacles, such as the above-mentioned supernumerary teeth or odontomes, may be the more likely reason for a secondary displacement of this tooth. While the early removal of this obvious aetiological factor may be strongly indicated, this will not necessarily affect the position of the tooth bud, which will probably continue to develop in its existing location.
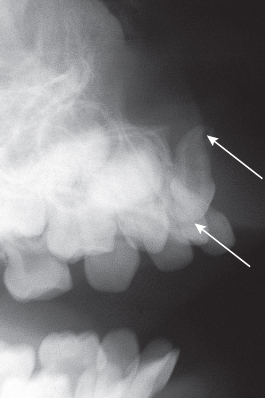
Fig. 5.2 An abnormally sited central incisor, whose root apex is close to the canine area. The shape of the root also appears to be abnormal.

Variation in the position of a developing tooth will produce a concomitant variation in its eruption path. When the eruption path is very slightly deflected, the tooth will usually erupt, but with an abnormal angulation of its long axis, indicating the path along which it will have travelled. As its vertical development proceeds, its relationship to the deciduous predecessor is more lateral, medial, palatal or labial to it. This will bring about a partial and oblique resorption along one side of the root of the deciduous incisor. In due time, the further progress of the permanent incisor and the oblique resorption pattern bring it into contact with the crown of the deciduous tooth on that side.
The permanent tooth may remain impacted if insufficient space exists. Alternatively, the tooth may finally erupt adjacent to the over-retained deciduous tooth and many months later than expected, possibly into a cross-bite relationship, or it may be proclined labially, or a diastema may be produced in the midline. This situation may not be self-correcting after the belated shedding or extraction of the stubborn deciduous tooth.
Should the position of the developing tooth be more markedly displaced, which is unusual, its potential eruption path will be in a more obtuse direction and little or no resorption of the deciduous tooth will occur. In these circumstances, eruptive movements are minimal and the permanent tooth remains in a more or less unchanged position over a long period. Finally, when positive intervention is undertaken, removal of the cause will need to be supplemented with active appliance therapy for its resolution.
Traumatic Causes
Obstruction Due to Soft Tissue Repair
The traumatic, sudden and very early loss of the deciduous incisor teeth is most often the result of an accident that delivered a blow to dislodge the tooth, usually while the child was at play. The possibility also exists for this to have been caused by a dental extraction, prompted by the presence of deep caries or following the sequelae of an earlier trauma. This typically happens at the age of 3 or 4 years, at a time when the permanent incisor is not ready to erupt and a healing-over of the macerated gingival tissue occurs without the early eruption of the tooth. In time, changes take place in the connective tissue overlying the developing permanent incisor, which prevent the tooth from penetrating the mucosa [7, 8]. By the age of 7 or 8 years, one may see and be able to palpate the bulging profile of the central incisor (see Figure 3.2a).
Dilaceration
In the early stages of their development, high in the anterior part of the maxilla, the permanent central incisors are situated lingual and superior to the apices of the deciduous incisors. Their positions change as the result of their labially and inferiorly directed migration, which is part of their normal further development and, as they do so, an oblique resorption of the roots of their deciduous predecessors is initiated.
During this critical period, children are frequently involved in traumatic episodes of various degrees of intensity and a blow may be inflicted on the deciduous maxillary incisors from the front. A blow of sufficient magnitude will produce a lingual avulsion of the crowns of the incisors and a concomitant labial displacement of the roots, which will sometimes cause a fracture of the labial plate (Figure 5.3). In this situation, the roots of the teeth and the sharp edge of bone will be palpable in the labial sulcus, although the overlying mucosa will usually remain intact. Since the unerupted permanent incisors are superiorly and lingually placed in relation to the resorbing root ends of the deciduous incisors, the successional teeth will usually not be displaced and will often continue unhindered in their normal developmental path.
Fig. 5.3 The tangential view shows severe labial displacement of the root of the deciduous incisor.
(Courtesy of Professor J. Lustmann.)
The roots of incisor teeth are tapered apically, which means that a blow directed along their long axis from below will drive the tooth upwards into a similarly tapered socket. It follows that the alveolar process fracture that may occur will cause a part of the labial plate of bone to become displaced labially and the teeth to be displaced superiorly (intruded). Under these circumstances, trauma to the anterior part of the deciduous dentition may cause damage to the growing tooth buds of the permanent dentition, and this may alter the further development of the permanent teeth in many ways. The anomalies that may occur vary from a discoloured hypoplastic mark on the enamel, through anatomic malformations of the crown or root, to non-proliferation of the root, to pulp death and sequestration of the tooth bud [8]. The alterations in the form of the crown and the root of these teeth are collectively referred to as dilacerations. These are the result of recovery from the blow that will have disturbed the natural development, resulting in a variable combination of a hypocalcified, altered, attenuated and directionally reoriented form of the crown and/or root. The final shape and appearance of the injured tooth will be dictated by the direction and force of the blow and by the particular stage of development of the unerupted permanent tooth. Each these anomalies will be unique in its form and no two trauma incidents will produce the same result.
In direct contrast, there is one type of dilaceration, which we shall refer to here as the ‘classic’ dilaceration, which consistently reproduces an almost identically shaped tooth (Figure 5.4), whose unerupted location is always the same. Its causation has, over the past six or more decades, been the subject of much discussion among paediatric dentists and orthodontists.
When the trauma is directed in the long axis of the deciduous tooth, it may be transmitted superiorly to the developing permanent tooth. According to this hypothesis, the force delivered by the violent blow to the deciduous incisor is transmitted to the resorbing root apex, which momentarily establishes a point of impact with the palatal side of the crown of the permanent incisor. This has been believed to cause the partially developed and unerupted permanent incisor tooth an immediate upward and labial rotation, in its crypt. It is then assumed that any further root development that occurs in the post-trauma period will continue in the same direction as before, producing a bizarre angle between the pre- and post-trauma portions of the tooth – the ‘classic’ dilacerated central incisor – with labial displacement of the crown portion. The site of this junction will depend on the stage of development of the root at the time of trauma, and with it the prognosis of any proposed orthodontic treatment for the tooth. This reconstructed scenario for the causation of this classic form of dilaceration is extremely well known and probably represents a majority opinion, if not consensus, within the profession.
Palatal, rather than labial, displacement of the crown vis-à-vis the post-traumatic root portion may occur in rare instances as a variation of the above theme and is due to a more palatal position of the tip of the developing permanent incisor and the apex of the deciduous incisor root, at impact. This is a more likely variation in the very young, during the early calcification of the tooth crown when its palatal location is normal (Figure 5.5).
Fig. 5.5 A palatally-oriented dilaceration of the central incisor. (a) Anterior section of the panoramic film to show the impacted dilacerate left central incisor with its labial surface facing inferiorly. The unerupted permanent left canine, which is transposed with the mesially-tipped lateral incisor, is seen to be directly above it. The deciduous canine with an intact root is seen distal to the lateral incisor. From this view, it is impossible to tell whether the crown of the central incisor points labially or palatally. (b) The lateral cephalometric view shows the outline of a screw post in the restored right central incisor. Above it, the profile of the palatally directed crown of the central incisor can be clearly seen, with its root portion curving labially and superiorly in a tight quarter-circle, encompassing the more superiorly placed and labially directed permanent canine. (c) The anterior occlusal view shows the typical form of the canine superimposed and largely masking the crown of the incisor. The apical portion of the incisor root is viewed in its cross-section anterior to the tip of the canine crown. (d) The periapical view provides a separation of the two teeth although, taken in isolation, it may give the inexperienced diagnostician the misleading impression that the crown of the incisor is labial.
In an attempt to determine whether there was an evidence base for accepting the above hypothesis, a protocol was instituted some years ago in the emergency clinic of the Department of Paediatric Dentistry at the Hebrew University–Hadassah School of Dental Medicine, Jerusalem. Children who attended the clinic having suffered trauma to their anterior deciduous teeth were subjected to routine clinical and radiographic examination, vitality testing and emergency pulpal and restorative treatments, as indicated. Until the new protocol was established, the radiographic examination had generally been limited to a periapical film of the area. It is obvious that this radiographic view is not suitable for showing any labial and superior displacement of the crown of the unerupted permanent central incisor within the crypt. Accordingly, the new protocol included a tangential radiographic view of the anterior maxilla, which has been described in Chapter 2 as being a view taken from the side, across the occlusal plane, and identical to a restricted area of a lateral cephalometric radiograph. It is obtained on a small, occlusal-sized film by holding the film vertically against the cheek and parallel to the mid-sagittal plane of the skull. Any alteration in the labio-lingual and vertical orientation of the crown of an incisor will be immediately discernible on this film.
The protocol was run for several years and did not discover a single case where the crown of the tooth had been displaced in the immediate post-trauma period in this way. However, in the succeeding years among the small but significant number of patients who turned up in the Department of Orthodontics with a fully developed, classic, dilacerated central incisor, several had been seen in the emergency clinic of the Department of Paediatric Dentistry following trauma in their earlier years. Since records existed from that time, the radiographs that had been taken when the protocol was in force were re-examined with specific regard to these patients. No displacement of the crowns of the unerupted permanent central incisors could be discerned on the immediate post-trauma films, effectively discrediting immediate tooth germ displacement as a cogent explanation for the aetiology of the phenomenon.
A developmental origin has been suggested as an alternative cause for the classic dilacerations [9], with the contention that the active process of the development of cysts, odontomes or supernumerary teeth may produce this phenomenon by displacement of the crown of the tooth or by interference and redirection of its root. In a retrospective study of the phenomenon [10] no history of trauma could be elicited in 70% of the patients in the sample, nor was there macroscopic or microsopic evidence of trauma, or the existence of a cyst, odontome or extra tooth in these patients. No case was found with both central incisors affected and there had been no damage to neighbouring teeth, which could be expected to occur in at least a few instances had trauma been the cause.
These cases also failed to show two distinct and angulated portions to the root, but rather a continuous and tight curve (Figure 5.4), quite different from those in which trauma, as an aetiological factor, had resulted in any of the other forms of dilaceration. The conclusion of the study was that a fairly high proportion of dilacerations occur due to an ectopic siting of the tooth germ, whose root development is deformed by its proximity to and the anatomy of the palatal vault in the immediate vicinity.
These explanations are unsatisfactory on several counts. Different cases show an almost identical and very typical anatomy of the tooth, which affects maxillary central incisors exclusively – no case of bilateral occurrence or parallel incidence in lateral incisors has been reported in the literature. As if to illustrate the exception that proves the rule, the records of a single case of bilateral occurrence were sent to the author (Figure 5.6) a few years ago and it remains the sole case that the author has seen. The morphology of the crown of the affected tooth is normal and is an exact mirror-image of its erupted antimere and the coronal portion of the root shows initial normal development. The remainder of the root develops strictly in the labio-lingual plane along a tight and continuous circular path, rather than two straight portions of root at an angle to one another. The crown is grossly displaced in the bucco-lingual and vertical planes, while exhibiting minimal or no mesio-distal rotation.
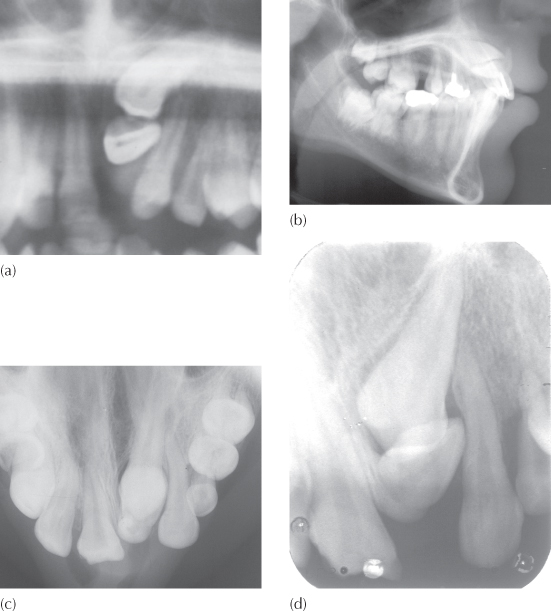
Fig. 5.6 An extreme rarity: bilateral classic dilacerations of the central incisors.
(Courtesy of Dr. Srdan Marelic.)
(a) Mesial drifting of the erupted lateral incisors has largely closed off the space for the unerupted central incisors. The intra-oral anterior view of the dentition.
(b) The intra-oral occlusal view.
(c) The cephalogram.
(d) Panoramic view.
Not only is the anatomy typical, but the position and orientation of the tooth are also unique. The crown of the tooth is upturned and displaced high in the sulcus on the labial side of the alveolus, with its palatal aspect palpable on the labial side of the sulcus close to the root of the nose. Often, the root apex of the tooth is palpable on the palatal side of the alveolus (Figure 5.5) and may be the sign that influences an unwary surgeon to mistakenly approach exposure of the tooth on the wrong side (see Figure 12.12).
It has been suggested that the loss of a deciduous incisor may lead to scarring along the eruption path of the permanent incisor, which deflects the developing tooth labially [8]. This runs counter to Stewart’s observation that no history of early traumatic loss of the deciduous tooth had occurred in 70% of the cases in his series.
The Jerusalem Hypothesis
It is possible to read a completely different aetiological interpretation into these very constantly occurring features, and it is pertinent to begin by questioning the reliability of a child’s or parent’s memory regarding traumatic injury of the front teeth. Severe trauma is rare and always remembered, but non-disfiguring trauma (i.e. trauma that causes no loss, fracture or displacement of the deciduous anterior teeth) occurs quite frequently in young children, is rarely noted and almost never remembered in later years. Indeed, following a relatively minor blow, the child may have come home in tears, but the incident will often have been forgotten the next day, at most with some minor, residual, temporary soreness or tenderness.
Abrupt and vertically directed force through the long axis of the deciduous tooth will bring about the transference of the impact to the intimately related, unerupted, permanent central incisor. Because the long axis of the permanent incisor has a more labially tipped orientation, the force will be transmitted in an oblique line which runs through the incisal edge and the most superior point on the labial side of the newly forming root, close to or at the root-mineralization interface (Figure 5.7). This most recently formed extremity of the partially developed root has a circular knife edge of calcified dentine. Thus, the intrusive blow will be delivered directly to the sensitive cells of Hertwig’s root sheath at this narrow rim. The intrusive force is thus concentrated along the knife edge root extremity and will inflict considerable damage on cells of the formative root sheath, with relatively low force values. It will be appreciated that precision in direction may be more critical than force magnitude.
Fig. 5.7 A diagram to show how a vertically directed force through the deciduous incisor is transmitted to the labial aspect of the mineralizing root of the unerupted permanent incisor.
Reproduced from previous edition with the kind permission of Informa Healthcare – Books.
Image not available in this digital edition
It is entirely possible that the root sheath may only partly recover from the blow, which may result in an attenuated rate of production of dentine on the labial side of the tooth. With the remainder of the root-forming system continuing to produce dentine unscathed, undeterred and unabated, it follows that the final shape of the root of this tooth will conform to a continuous labially directed curve (Figure 5.8), until apexification is achieved. Furthermore, since the dental papilla base of Hertwig’s root sheath maintains its position within the alveolar process fairly constantly – against the eruptive force of the developing tooth – and provides the platform from which the downward development of the root is normally directed, the crown of the incisor moves labially and superiorly for as long as this bucco-lingually unequal mineralization gradient of the developing root continues. In other words, dilaceration of this classic type is an anomaly which is traumatic in origin but developmental in its expression.
Fig. 5.8 A diagrammatic illustration of the progressive alteration in the orientation of a dilacerated incisor, during the disturbed root formation. Note that the position of Hertwig’s proliferating root sheath remains unaltered.
Reproduced from previous edition with the kind permission of Informa Healthcare – Books.
Image not available in this digital edition
This hypothesis provides an explanation for the typical appearance of the dilacerated tooth, as well as its final unerupted position under the nose. Furthermore, since it may occur with a relatively minor trauma, this could account for the high proportion of cases with no apparent history of trauma experience and no premature loss of or damage to the adjacent teeth. Its relative rarity may be due to the positional relationship between the deciduous and permanent incisor at the time of injury and a very specific directional relationship with the traumatic force vector. This may account for an absence of bilaterally affected cases, for its non-occurrence among lateral incisors and for an absence of any association with supernumerary teeth, cysts and odontomes. It also provides an explanation as to why there is no obvious displacement visible on the tangential radiographs that were taken immediately following the traumatic episode (Figure 5.9) and why the tooth is never rotated in the horizontal plane.
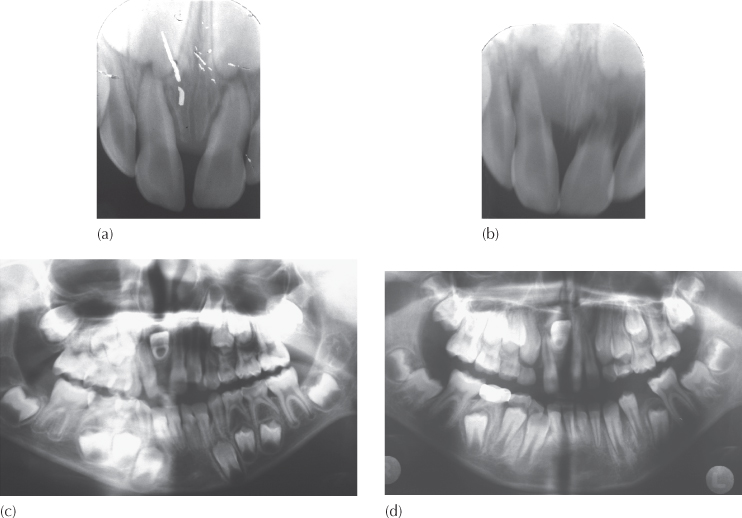
Fig. 5.9 Dynamic development of a ‘classic’ dilaceration. (a) A periapical view of the maxillary incisor area of a 3.11-year-old child taken in the emergency room on the day that trauma had occurred. Note there is no apparent displacement of either central incisor. The left side appears to be the worst affected by the trauma. (b) A six-month follow-up film shows considerable inflammatory resorption of the root of the left deciduous central incisor and less on the right side, but there is a concomitant subtle change in the relative positions of the unerupted permanent incisors. On the right side, the incisal edge is more superiorly located in relation to the left incisor and to the root of its deciduous predecessor. (c) The initial diagnosis of dilaceration of the right central incisor was made on the basis of this panoramic view, taken at age 7.6 years (i.e. 3.7 years post-trauma). Note the anatomical labial surface of the crown faces superiorly, with the orientation of the crown portion being slightly above the horizontal. The pulp chamber is very large, indicating that root development is continuing. (d) A new panoramic view taken 2.4 years later shows the tooth to be higher still, to one side of the anteriorly nasal spine and tipped further posteriorly. Its palatal surface is now facing anteriorly and its pulp chamber is much smaller.
Arrested Root Development
When a pre-school child suffers a very severe blow to the maxillary anterior dentition, it is likely to result in the loss of the deciduous incisors, but it may also cause fracture of one or both jaws. The root-producing ring of cells that comprises Hertwig’s sheath may have been so seriously damaged as to have effectively caused serious disruption or actual cessation of any further root development. These teeth may lose their eruption potential, while the adjacent teeth will continue to erupt, bringing with them vertical proliferation of alveolar bone. Only at a much later stage will this phenomenon be discovered when the affected tooth or teeth do not erupt and an area of vertically deficient and bucco-palatally narrow, edentulous alveolar ridge becomes evident.
Radiographs will usually reveal a normal axial inclination and an undisturbed sagittal and lateral location of the crown of the tooth. In the vertical plane, it will be situated very high up in the premaxilla, with minimal or no root formation, depending on how much root had already developed at the time of the accident (Figure 5.10).
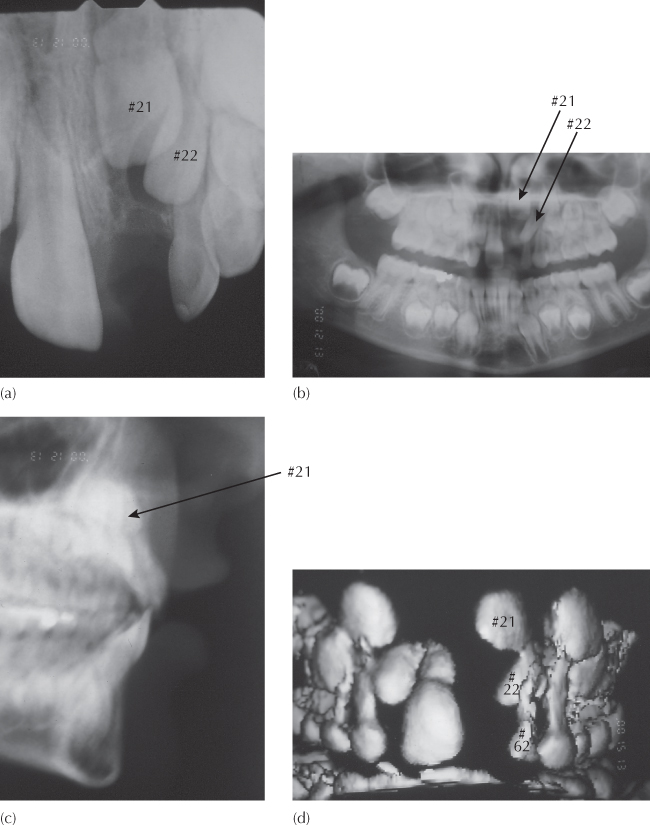
Fig. 5.10 Arrested root development due to severe trauma at age 3 years. Records taken at age 7.4 years. (a) A periapical view of the unerupted, but normally oriented, left central incisor (#21) shows a marked height discrepancy compared to the erupting right incisor. Note the late developing lateral incisor (#22) is inferiorly placed, tipping mesially and more advanced in terms of its eruption status. The affected incisor shows little or no root development. (b, c) The panoramic and cephalometric views show the incisor to be close to the floor of the nose and a normal crown orientation. (d) The anterior view seen in this three-dimensional image from the cone beam computerized tomography (CT) scan. (e, f) Two paraxial (vertical) cuts from the CT scan illustrate the vertical relationship between the unerupted central and lateral incisors and the deciduous lateral incisor (#62). They also show the labial cervical area of the crown coming to an abrupt step where cessation of crown formation occurred and where the minimal root development is almost at a right-angle to the general orientation of the crown and in close relation with the floor of the nose.
Acute Traumatic Intrusion (Intrusive Luxation)
Traumatic injury occurs in young children as the result of play-related activities in school or at home, in accidents involving a fall or, occasionally, as the result of deliberate physical violence [8]. The effects on the teeth range from a transitory pulp inflammation, through the various types of fracture of the crown of the tooth or of its root, to, in the severest cases, avulsion of the entire tooth. Intrusion of one or more of the incisor teeth is often associated with a fracture or comminution of the labial plate of bone and a tearing of the periodontal fibres.
A child may present at the emergency clinic with what gives the appearance of a total avulsion, since the tooth is not visible in its former place, the gingivae are lacerated and there is a considerable amount of blood clot. A periapical radiograph of the area will reveal a superior displacement of the tooth into the alveolar bone, without necessarily producing a fracture of either the crown or the root. The labial plate is displaced labially, although it is most often held closed by the injured but uninterrupted band of labial gingiva and oral mucosa. The integrity of the blood supply to the soft tissues is usually intact, and this allows good and rapid soft tissue healing.
In a sense this tooth has been totally avulsed, but in an atypical manner. It is completely displaced from its socket, with total severance of its attachment apparatus and disruption of its vital supply lines. When compared with the typical avulsed case, however, it has one enormous advantage, and that is that the tooth has not been allowed to dry; it has not usually been in contact with any form of contaminated material and it is not necessary to store it in saliva or milk or other recommended isotonic medium, before restoring it to its rightful place. It is situated in an area initially surrounded by a coagulating haematoma and later by organizing blood clot, and it must be assumed that the damaged periodontal fibres in this situation fare considerably better than do those of the replanted tooth, which has spent some time out of the mouth. This is dealt with in detail in Chapter 13.
Diagnosis
History
A missing permanent central incisor is likely to be the presenting symptom of a child when the contralateral central incisor has been present in the mouth for several months. Urgency on the part of the parent may be sharpened when the lateral incisor of the same side erupts and clearly reduces the size of the place for the absent tooth. Ideally, many children will have been seen by the paediatric dentist for routine dental checks in the past and will have been referred by the dentist for the orthodontic opinion, but many others may be self-referred directly to the orthodontist. With the notable exception of the acute traumatic impaction cases referred to above, urgency does not exist in the present context in contrast to most other forms of presenting symptom, such as pain and swelling.
When seeing a patient who attends for the first time exhibiting absence of an erupted permanent central incisor, the general medical history should be recorded carefully. It must be borne in mind that surgical intervention is very likely to be needed as an essential part of the treatment that is to be provided. Accordingly, such aspects as previous illnesses, particularly rheumatic heart disease, drugs being taken and bleeding tendencies, together with any other important and relevant items of information, require to be elicited at the outset.
Questions should be asked, with particular emphasis placed on the possibility of an episode of past trauma. The parent should be questioned carefully to discover whether the child is generally accident-prone. Direct mention of bicycle accidents, falling from a chair, ladder or tree, or being hit in the mouth during play should be made and all relevant answers should be carefully recorded, together with the approximate dates of their occurrence. The possibility of well-hidden child abuse should be considered and, when there is suspicion of this, a report should be made to the local police.
Clinical Examination
Much of the patient’s dental experience and history is possible to ascertain from a glance at the dentition itself. The existence of sealants and restorations, the absence of teeth, gingival inflammation and the level of oral hygiene will often tell a great deal about past attitudes of both the patient and the attending dentist to prevention and to restorative procedures. At the time the patient attends for treatment, the presence or absence of the deciduous incisor is generally irrelevant. The central incisor of the opposite side and the lateral incisor of the same side will usually be seen to be tipped towards one another, and there will usually be insufficient space at the occlusal level for the placement of the unerupted tooth. Widely apically divergent long axes of the two adjacent teeth will suggest the presence of an unseen and undiagnosed space-occupying physical obstruction.
Palpation
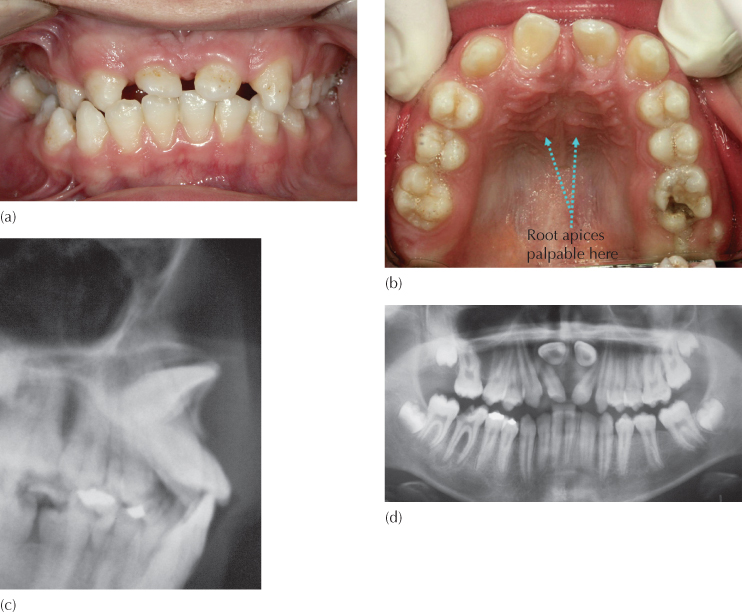
In the obstructed cases, the unerupted tooth itself is often high on the labial side of the alveolar ridge and there may be additional and smaller irregularities bulging the alveolus more inferiorly. These are best identified by palpation. There will almost always be a labio-lingual widening of the ridge (Figure 5.11). If the ridge area is relatively thin inferiorly, it will indicate that teeth are not present at this level (Figure 5.12).
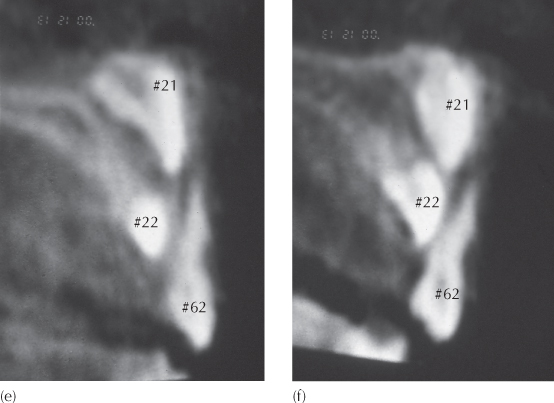
Fig. 5.11 (a–c) Clinical views of a patient with a bulging ridge form due to obstructive impaction of the central incisors. Three deciduous incisors are over-retained and the permanent lateral incisors are erupting rotated and with a mesio-labial angulation. The ridge bulges due to the presence of dental obstruction. (d) Periapical views of the anterior region show displaced long axis orientation of the central incisors and the existence of several supernumerary teeth.
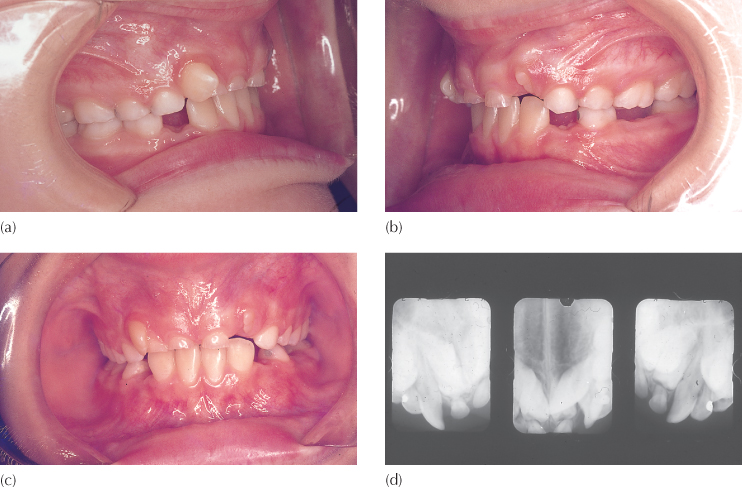
Fig. 5.12 (a, b) Frontal and occlusal clinical views of a patient with a dilacerate central incisor, illustrating a bucco-lingually and vertically deficient ridge, due to the absence of teeth in the immediate area – the ‘hourglass’ ridge.
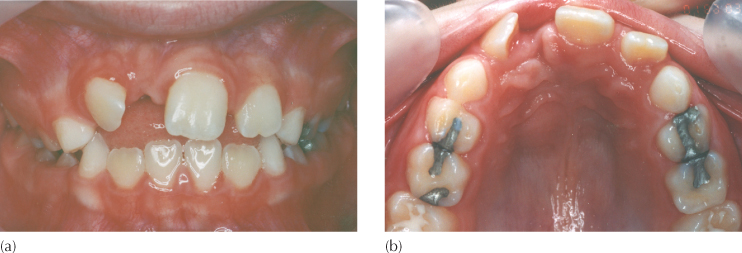
The importance of palpation of the area is not to be underestimated since, if it is not performed sufficiently thoroughly, an important diagnosis may be missed. The presence of a dilacerated central incisor will only be revealed by clinical examination if palpation is made very high in the labial sulcus. Normally, the superior midline area is delineated by the prominence of the anterior nasal spine, on each side of which a shallow depression will be felt. The palatal surface of a dilacerated incisor crown faces forwards and produces a hard swelling in the place where the shallow depression is expected. By superiorly retracting the upper lip, the oral mucosa may be seen to move freely over the stretched area, which will emphasize the outline of the cingulum of the tooth.
Palpation of a dilacerated central incisor may often be made in two places. With the abnormal position of the coronal portion of the tooth, the further development of the root portion may be along an axis which is tipped more lingually and, in the later stages of root closure, the apex may become palpable as a small, hard lump in the palate. This is a feature which few clinicians seem to look for and is a more consistent finding than may be realized [11]. Mistaken diagnosis of crown location is an unusual event since both the orthodontist and the oral surgeon need to undertake a clinical examination and review the radiographs before treatment and it is difficult to imagine that the same mistake could be made twice. Notwithstanding, as we shall see in Chapter 12, such occurrences are seen from time to time (Figure 12.12).
Radiographic Examination
In Chapter 2, the different methods of radiographically viewing unerupted teeth were discussed in general and it was pointed out that a periapical view provides essential qualitative information and as such, should be the first step in this part of the examination.
In the case of an unerupted central incisor, this view will generally show associated pathology with great clarity, including hard tissue obstructions (supernumerary teeth of the carious types, odontomes), soft tissue lesions (cysts, tumours), and abnormal root and crown morphology of the unerupted tooth. From this alone, it will usually be possible to establish the reason for the failure of the tooth to erupt.
If supernumerary teeth or odontomes are seen on the film, the information that will then be required relates to their size, number and mesio-distal relationship to the midline and the incisor teeth, all of which will be obvious from this view. However, their labio-lingual orientation in relation to the adjacent erupted teeth will not be obvious from this one film. Since the periapical view is obliquely angled to the horizontal plane, a labial supernumerary tooth will appear lower in the vertical plane than a palatal supernumerary which is situated at the same height. Accordingly, the assessment of height is directly related to the labio-lingual position of the tooth, and this provides the basis for the vertical tube shift method of locating the bucco-lingual relationship of an impacted tooth to an erupted tooth, described in Chapter 2.
For patients in whom the aetiology is the presence of unerupted supernumerary teeth and at the age at which most patients will attend for treatment, a true lateral, tangential view is not helpful, due to the superimposition of central and lateral incisors, deciduous and unerupted permanent canines, and the supernumerary teeth. A second periapical view, directed from a more distal vantage point, will usual/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



