CHAPTER 5 MASTER PLANNING OF THE IMPLANT CASE
Over the past three decades implant dentistry has become the leading and most dynamic discipline in the dental field. Oral reconstruction with dental implants has gone from just single-tooth replacements and over-dentures to encompass sophisticated surgical and prosthetic techniques and principles. Every specialty within dentistry plays an important part in the successful outcomes of these very rewarding cases. This chapter describes the interdisciplinary approach to comprehensive treatment planning and the many facets involved in quality, long-standing aesthetic and functional treatment.1,2
 Initial Consultation
Initial Consultation
The patient’s health status should be evaluated in a way similar to the screening admissions procedure conducted with patients entering the hospital.3–5 The main components to be considered are:
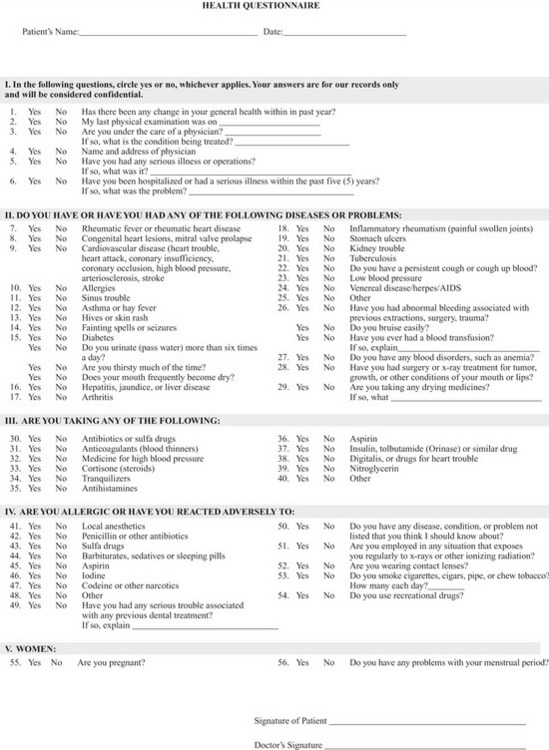
Medical History
In gathering the patient’s medical history, special attention should be given to whether the patient has the ability to physically and emotionally sustain all the procedures that may be required in implant therapy, including surgery, a variety of anesthetics and pain-control drugs, and prosthetic rehabilitation.6–8 The American Dental Association provides a long-form health questionnaire on their website that is an excellent tool for gathering this information, available at https://siebel.ada.org/ecustomer_enu/start.swe?SWECmd=Start.9 Figure 5-1 shows an example of a typical health history questionnaire.
In addition to obtaining the patient’s health history, the doctor must assess vital signs (blood pressure, pulse, and respiration) and record these assessments in the patient’s chart. When a patient has not had a comprehensive medical work-up for several years or when findings are positive on the health questionnaire, additional laboratory testing may be advisable. These tests may include complete blood count, urinalysis, or sequential multiple analysis of the blood chemistry (SMAC). The results can contribute to the patient’s medical profile (Table 5-1).2,3
| Test procedure | Units | Reference range |
|---|---|---|
| Sodium | mmol/L | 135-146 |
| Potassium | mmol/L | 3.5-5.3 |
| Chloride | mmol/L | 98-110 |
| Carbon dioxide | mmol/L | 21-33 |
| Calcium | mg/dL | 8.6-10.2 |
| Alkaline phosphate | Units/L | 33-130 |
| AST | Units/L | 10-35 |
| ALT | Units/L | 6-40 |
| Bilirubin, total | mg/dL | 0.2-1.2 |
| Glucose | mg/dL | 65-99 |
| Urea nitrogen | mg/dL | 7-25 |
| Creatinine | mg/dL | 0.60-1.18 |
| BUN/creatinine ratio | 6-22 | |
| Protein, total | g/dL | 6.2-8.3 |
| Albumin | g/dL | 3.6-5.1 |
| Globulin, calculated | g/dL | 2.2-3.9 |
| A/G ratio | 1.0-2.1 | |
| Egfr non-African American | mL/min/ | 1.73 m2 > or = 60 |
| Egfr African American | mL/min/ | 1/73 m2 > or = 60 |
Combining the information from the health questionnaire, the vital signs, and the laboratory test results will enable the doctor to categorize each patient into one of the five classifications of presurgical risk formulated by the American Society of Anesthesiology (Box 5-1).8 According to this scheme, a Class I category includes the patient who is physiologically normal, has no medical diseases, and lives a normal daily lifestyle. The Class II category includes the patient who has some type of medical disease, but the disorder is controlled with medications. The patient can thus engage in normal daily activity. An example of this category of patient is one with hypertension who has been placed on antihypertensive medication and, as a result, has normal blood pressure and no other impairments. The Class III category includes the patient who has multiple medical problems, such as advanced-stage hypertensive cardiovascular disease or insulin-dependent diabetes, with impaired normal activity. Patients in the Class IV and V categories have advanced states of disease. Class VI is a patient who is considered brain dead and is a potential organ donor. For example, a patient in the Class IV category has a serious medical condition requiring immediate attention, such as the person with acute gallbladder disease who needs immediate treatment. The patient in the Class V category is usually moribund and will not survive the next 24 hours. Most patients who seek implant reconstruction fall into the Class I or II categories and sometimes Class III. For obvious reasons, patients in Classes IV and V are not appropriate candidates for implant procedures. However, consideration of whether a patient falls into Class I, II, or III will enable the implant practitioner to more effectively decide what kinds of procedures should be undertaken, where the surgery should be performed, and what kind of anesthesia is appropriate. Furthermore, cases with patients categorized as Class III may require preparatory measures such as stabilizing or controlling a diabetic patient before implant surgery can be considered.
BOX 5-1 The American Society of Anesthesiologists’ classification of presurgical risk
Dental Status
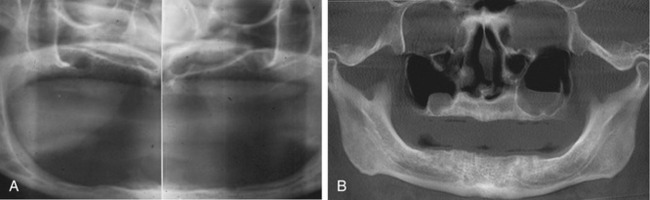
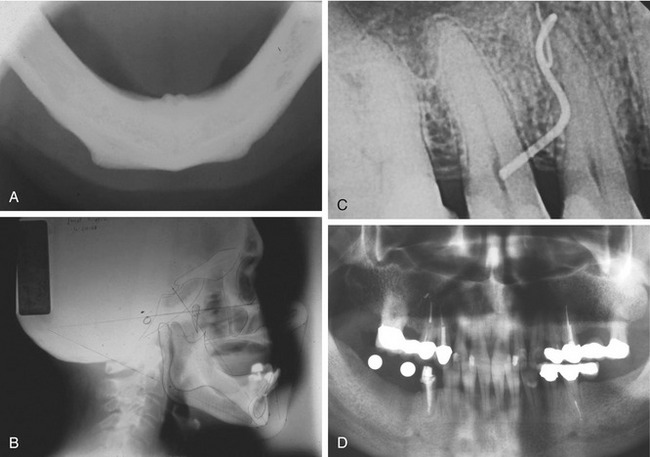
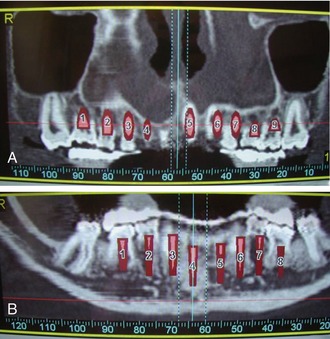
Today’s modern dental offices can provide a host of radiographic information through digital and computer analog equipment that allows unprecedented detail and data applications never available before. Digital panoramic and office-based cone beam CT scanners (Figure 5-2) are now readily available. These devices can give studies that accurately define the full scope of the maxilla and mandible, as well as the accompanying vital structures (i.e., sinus, floor of the nose, position of the mandibular canal, mental foramen) (Figure 5-3). In addition, information about the thickness of cortical plates, bone densities, and soft tissue contours is easily obtained. Chapter 8, Contemporary Radiographic Evaluation of the Implant Candidate, and Chapter 18, An Introduction to Guided Surgery, expand on this technology. There still is a place for conventional film-based radiographs because much valuable information can be learned from them. These might include occlusal films, lateral cephalometric images, and periapical or panoramic images (Figure 5-4).10 However, with the advent of digital referenced planning software our ability to diagnose and plan procedures virtually takes radiographic diagnosis and treatment planning to a new level (Figures 5-5 and 5-6).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses