5
Infant Oral Health
Case 1
Perinatal Oral Pathology
Figure 5.1.1. Intra-oral photo showing natal teeth

A. Presenting Patient
- 7-day-old male
- Consultative visit requested by neonatologist
B. Chief Complaint
- Neonatologist requests “evaluation of what appear to be teeth erupting on bottom jaw”
C. Social History
- First child
- 21-year-old single, immigrant mother
- Qualified for public assistance
D. Medical History
- Born two weeks prematurely
- On ventilator for two days
- Currently in pediatric intensive care unit (PICU)
- Obtain a thorough history of the pregnancy and birth
- Obtain a thorough understanding of the child’s natal teeth, including when first observed, associated complications with ventilator tubing, or infections
Cunha et al. (2001), Amini and Casamassimo (2010)
E. Medical Consult
- N/A
F. Dental History
- Teeth present at birth
G. Extra-oral Exam
- Head misshapen
- Sparse hair
H. Intra-oral Exam
- Edentulous maxillary arch
- High maxillary frenum
- Palate intact
- Mandibular arch with teeth in O and P positions, partially erupted, brownish in color, rotated and firm to manipulation
- Determine if the teeth present a problem for nursing due to irritation of child or mother. Also determine the potential risk of aspiration if teeth are mobile
- If removal is contemplated, use radiographic examination to determine whether teeth are supernumerary or prematurely erupting normal teeth
I. Diagnostic Tools
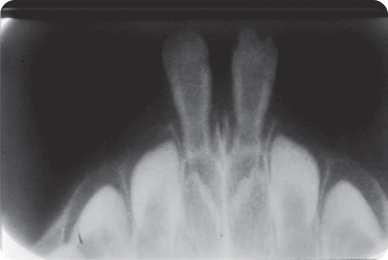
- Occlusal radiograph of mandibular anterior region
- Teeth can be present at birth (natal teeth) or erupt shortly after birth (neonatal teeth)
- Most natal teeth are members of the normal complement of primary teeth
- Most natal teeth appear in the mandibular anterior region
- Natal teeth may be associated with other disorders, usually those involving the skin, bones, or ectoderm, such as chondroectodermal dysplasia. Therefore, careful systemic evaluation of children with natal teeth is necessary
Figure 5.1.2. Mandibular occlusal radiograph showing natal teeth
J. Differential Diagnosis
- Other congenital neonatal pathology including Bohn’s nodules, Epstein’s pearls, and other retention phenomena
K. Diagnosis and Problem List
Diagnosis
- Natal teeth
Problem List
- Potential for nursing difficulty
- Potential for aspiration
- Potential for traumatic ulcer of the ventral surface of the tongue (Riga-Fede). See Figure 5.1.3 for an example of Riga-Fede
- Potential for trauma to the mucosa of the opposing arch
Figure 5.1.3. Traumatic ulcer (arrow) on the ventral surface of the tongue

L. Treatment Plan
- Observe for mobility, ulcerations, nursing difficulty
- Extraction as indicated
M. Prognosis and Discussion
- No literature describes the risk of aspiration of natal teeth, so removal should be based primarily on the appearance, firmness, and likelihood of function of the tooth
- In the event the tooth is a member of the normal complement of primary teeth, parents should be made aware that the loss might result in alteration of spacing and alignment of the remaining primary teeth
N. Complications and Alternative Treatment Plan
- How would the treatment plan change if breastfeeding were negatively affected?
- How would the treatment plan change if the infant developed a ventral tongue surface ulcer?
Self-study Questions
1. What is the probability that natal teeth are members of the normal complement of primary teeth?
2. Where do natal teeth most often occur in the mouth?
3. What are reasons for removal of a natal tooth?
4. What is the difference between a natal and neonatal tooth?
5. What are characteristics of other neonatal oral lesions that would help differentiate a natal tooth?
Answers are located at the end of the case.
Bibliography
Amini H, Casamassimo PS. 2010. Prenatal dental care: a review. General Dentistry 58(3):176–80.
Cunha RF, Boe FAC, Torriani DD, Frossard WTG. 2001. Natal and neonatal teeth: review of the literature. Pediatric Dentistry 23:158–62.
Oral health care during pregnancy and early childhood. Practice guidelines. http://www.health.state.ny.us/publications/0824.pdf.
SELF-STUDY ANSWERS
1. The overwhelming probability is that a natal or neonatal tooth is a member of the 10 primary teeth in the arch, with fewer than 10% in most surveys being supernumeraries.
2. Most natal teeth occur in the mandibular arch in the incisor region, and more than half the time they occur in pairs.
3. Natal or neonatal teeth are removed if they present a risk of aspiration, are determined not to have functional integrity, if they present problems for the child in nursing, or if they are supernumerary teeth.
4. For definitional purposes, a natal tooth is one present at birth and a neonatal tooth is one that erupts after birth within the first 30 days of life.
5. The other congenital oral abnormalities, which might be mistaken for a natal tooth, include a keratin-filled body such as a Bohn’s nodule or a mucous retention cyst. These are softer in consistency.
Case 2
First Dental Visit, Acquired Pathology
Figure 5.2.1. Knee-to-knee exam position

A. Presenting Patient
- 16-month-old Caucasian female
B. Chief Complaint
- Mom states, “My pediatrician said I should take my baby to a dentist to look at her teeth.”
C. Social History
- First child
- Stay-at-home mother
- Medicaid coverage for medical and dental care
D. Medical History
- Allergies to nuts
- Gastroesophageal reflux (GERD)
- Medications: Pepcid AC
- Contact physician about nature of allergy: When it was first observed, intensity, therapy, how well controlled it is
- Note possible cross reactivity of various substances in patients with nut allergy, including some kinds of fluoride varnish
- Be aware of heightened risk of allergic responses to other materials used in dentistry, such as latex
- Determine the cause and extent of Gastroesophageal reflux (GERD) and efficacy of Pepcid therapy
E. Medical Consult
- Contact allergist or primary care medical provider
- Food allergies occur in the first two years of life and are IgE-mediated
- Cow’s milk, hen’s eggs, soy, peanuts, tree nuts, wheat, fish, and shellfish account for 90% of food allergies
- Management is based on identification of the antigen and then avoidance of the food
- Children often outgrow milk, soy, egg, and wheat allergies, but have lifelong problems with nuts and shellfish
Allen, Hill, and Heine (2006)
- Gastroesophageal reflux disease (GERD) causes dental erosion in most afflicted dental patients to some degree
- Drug treatments include acid-neutralizers (milk of magnesia), histamine-2 blockers (ranitidine/Zantac), prokinetic agents (cisapride/Propulsid), and proton pump inhibitors (omeprazole/Prilosec)
- Surgical treatment may involve fundoplication (Nissan procedure)
- Soft tissue involvement can include chronic laryngitis, laryngeal ulcers, chronic sore throat
Barron, et al. (2003)
F. Dental History
- Child has never been to a dentist
- Mother receives regular dental care
- Unfluoridated water system (private well)
- Oral hygiene is not performed
- Child is still on the bottle
- Child sucks thumb or pacifier when desired
- In the dental history assessment, cover the six major areas of anticipatory guidance: stage of development, oral hygiene, fluorides, diet, habits, and injury prevention
AAPD (2011–12), Nowak and Casamassimo (1995)
G. Extra-oral Exam
- Normal weight and height for age
- Head and neck exam within normal limits
H. Intra-oral Exam
- Intra-oral soft tissues normal, with minor gingivitis
- Fourteen teeth present and within normal range for age
- Plaque on teeth with areas of cervical decalcification (Figure 5.2.2.)
- Incisal edges rounded and worn but not carious
Figure 5.2.2. Intra-oral photo showing cervical decalcification

- Plaque on teeth at this age and the surrogate measure of gingivitis are strong predictors of future dental caries (Alaluusua and Malmivirta 1994)
- Loss of anatomical definition is one indicator of dental erosion and at this age should be a warning sign (Barron et al. 2003)
- Oral erythema and gingivitis also may accompany GERD (Barron et al. 2003)
I. Diagnostic Tools
- Caries Risk Assessment Tool
- Fluoride assessment of drinking water
- Caries risk: Use the AAPD Caries Risk Assessment Tool (CAT) in assigning a patient’s risk category:
http://www.aapd.org/media/Policies_Guidelines/P_CariesRiskAssess.pdf. - Fluoride Assessment and Prescribing: Use the AAPD Guideline on Fluoride Therapy to determine amount and vehicle:
http://www.aapd.org/media/Policies_Guidelines/G_FluorideTherapy.pdf.
J. Differential Diagnosis
- N/A
K. Diagnosis and Problem List
Diagnosis
- Normally developing child, with age appropriate oral development
- GERD
- High risk for dental caries
Problem List
- Still feeding from bottle, including at bedtime
- Indeterminate fluoride status
- No oral hygiene being practiced
- Dental erosion from GERD
L. Comprehensive Treatment Plan
- Provide parents with alternatives to bottle use and ways to eliminate sleeping with the bottle at night
- Perform an assessment of the fluoride content of the family’s main source of drinking water and prescribe supplementation as needed
- Instruct parent on methods of oral hygiene with attention to frequency and use of a “smear” of fluoridated dentifrice since this child is at increased caries risk as well as the susceptibility of acid-exposed enamel to wear
- Include recommendation for next health supervision visit to determine compliance and outcomes of preventive anticipatory guidance and progress of erosion
- Apply office-based fluoride
- Consider recommending a product containing amorphous calcium phosphate (ACP) to aid in remineralizing the teeth
M. Prognosis and Discussion
- Cessation of bottle feeding will hinge on providing the family with workable alternatives and strategies that fit into their lifestyle. Culture, family dietary habits, and stresses of daily life all need to be considered in recommendations because these are often listed as reasons why parents keep children on the bottle
- Fluoride assessment can be done through use of kits or by involving the local health department if it provides that service. The measure obtained must be from the main source of drinking water, but the clinician must also assess dietary habits and lifestyle issues, such as daycare, that may affect supplementation level. For example, a low-caries-risk child with other daily sources of optimally fluoridated water may not need supplementation
- Oral hygiene instruction requires consideration of location, timing, parents’ manual skills, use of dentifrice, devices, and positioning. Each of these affect success and outcomes
- The decalcification and erosive effects on teeth must be monitored closely and treated with full-coverage restoration if they progress to cavitation
- Establish a more frequent recall schedule for the next health supervision visit to assess success and provide the next phase of anticipatory guidance
N. Common Complications and Alternative Treatment Plans
- Allergy to nuts may also include reaction to some fluoride varnish formulations. Care should be taken to check with manufactuers before applied in the office
- Should a fluoride supplement be prescribed, proper dosing and storage should be covered to prevent overuse or poisoning
- A careful distinction should be made between erosion and cavitation from caries. These two separate entities are sometimes confused, especially on posterior teeth
- One school of thought would be to immediately crown the affected teeth, but if erosion of enamel or cavitation occurs on other teeth, this would require a second procedure
Self-study Questions
1. What are historical risk factors believed to be indicative of an elevated susceptibility to dental caries?
2. What are clinical risk factors believed to be indicative of an elevated susceptibility to denta/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


