5
How to Talk to Patients about Implant Dentistry: Risks, Benefits, and Alternatives
What are the risks, benefits, and alternatives to replacing missing teeth?
More than 3 million Americans have dental implants, only 3–5% of the target population. General dentists only recommend implants to their patients on an average of 25–35% on a daily basis. Therefore, there is a huge opportunity and responsibility for us as dental professionals to have a conversation with our edentulous or partially edentulous patients on how implant dentistry could benefit them and improve their quality of life.
Hygienists, on an average, spend 40–60 minutes of one-on-one time with their patients, more than any other team member in the office. It is imperative that you as a hygienist attain the verbal skills to talk with patients about the risks, benefits, and alternatives (RBAs) to replacing missing teeth with dental implants. An understanding of the RBAs and being able to pass this information on to patients will truly help patients to have a better understanding of their role, responsibility, and treatment options to make informed decisions about their long-term oral health.
Hygienists, how and when do you talk to patients about implant dentistry? The best candidates for implants are your existing patients of record. Identify which of your existing patients are missing one or more teeth with no replacement, patients with a fixed bridge, or currently wear a removable partial or denture. Patients with existing fixed bridges are at risk for decay, bone loss, or poor esthetics, and periodontal patients have the potential for future tooth or bone loss. Also, patients with congenitally missing teeth are patients in whom to plant the seed on the technological advancements in implant dentistry. Refer to Table 5.1 for a comparision of treatment options.
Table 5.1 Comparison treatment options for missing teeth.
| Treatment Option | Advantages | Disadvantages |
|---|---|---|
| Implants |
|
|
| Permanent bridge |
|
|
| Partial denture |
|
|
| Denture |
|
|
Branemark refers to edentulism as “a serious handicap, to be treated with the upmost respect.” The Surgeon General’s NIDCR Stategic Plan 2010 outlines the psychological issues of the fully edentulous patient as an oral disease that affects the most basic human needs: “the ability to eat and drink, swallow, maintain proper nutrition, smile, and communicate” (1).
Risks
The ultimate consequence or risk of not replacing the missing tooth with an implant is bone loss. More than 44 million people in the United States have at least one quadrant of posterior missing teeth and are potential implant therapy candidates (2). It is the dental professional’s responsibility to discuss the options of replacing missing teeth with every patient.
As a hygienist, one of the first questions that a patient will ask you after an extraction is, “What if nothing is done to replace it?” The patient can chose to do nothing, it is a viable option; but there will be consequences. Often, when a tooth is removed, the alignment of the teeth next to the missing tooth starts to shift. As the bite shifts, it can become very difficult, time-consuming, and expensive to repair, and over time atrophy or shrinkage of the jawbone can occur. Remember that the primary job of the jawbone is to retain the teeth, and when teeth are lost and the bone is not stimulated, it melts away.
Traditional dentistry can provide replacements for missing teeth using bridges, removable partials, and/or dentures; however, each of these has disadvantages. If a tooth is lost or needs to be taken out due to infection, fracture, or bone loss from periodontal disease, it can cause ramifications that extend far beyond that one tooth. Bridgework usually involves altering natural teeth to provide a stable foundation for support of replacement teeth. Partials and dentures can, at times, be very unstable, leading to denture sores or speech difficulties. All of these options potentially need to be replaced every 6–10 years.
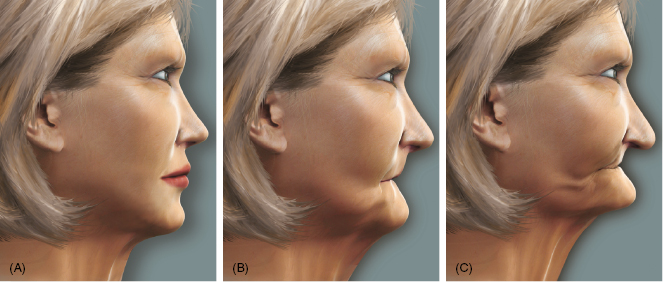
The ideal treatment is to replace the missing teeth at the time of extraction, before the shifting or jaw atrophy occurs. The longer the patient waits, the more involved and expensive the final solution becomes. Bone atrophy not only affects jaw function, but also facial esthetics. Esthetics starts with the integrity of the facial bone structures, so if the teeth are lost and not replaced, the bone melts away and the facial structures sag inward, causing a premature aging appearance.
The consequences to facial appearance illustrated in Figure 5.1 can be a very dramatic visual to show your patients! Make it visual and real to your patients when discussing the risks of not replacing missing teeth. Also give the patient the statistics of the risks of not replacing the missing tooth with an implant: bone loss of 25% in width of the ridge and an overall 4 mm of bone height during the first year after an extraction (3). These are important statistics that help the patient understand the urgency of replacing missing teeth before bone loss can occur.
Figure 5.1 Progressive bone loss affects appearance. Courtesy of BioHorizons.
The literature reports that only 60% of patients with partial dentures wear them in 4 years, and after 10 years only 35% are still wearing their partials (8). Oral hygiene can also be affected for patients wearing clasp-retained partials, and this includes an increase in plaque, bleeding on probing, and inflammation leading to periodontal concerns (4, 9, 10). The dental health complications created by increased stress on the attachment teeth leads to mobility, caries, and eventually to loss of the attachment teeth (10–12). The statistics for loss of abutment/attachment teeth range from 23% in 5 years, to 38% in 8 years, to 44% in 10 years (13). Clearly, there are demonstrated risks to not replacing missing teeth and obvious benefits to replacement with dental implants.
Benefits
The Surgeon General’s report highlights that “25% of people without teeth reported that they avoided close relationships because of fear of rejection when their toothlessness was discovered” (1). To simply be able to chew without pain or laugh without the embarrassment of losing your denture in pubic and have the confidence to start new romantic relationships is priceless to the edentulous patient. Replacing patients’ teeth and preserving the bone not only changes patients’ smiles, but also improves their quality of life.
Edentulous patients are truly the real winners in the age of implant dentistry. Many edentulous patients have worn dentures since they were 30 years old and now are oral invalids, unable to even wear their dentures except to weddings and funerals. More than 80% of edentulous patients have difficulty with speech and have to continue to spend money on denture adhesives to hold their dentures in place. Without it these patients could not wear their dentures due to ill fit from serious bone loss that has occurred over time, which can lead to serious quality of life issues (14).
Hygienists, have a conversation with your patients about the options for tooth replacement. Talk about all the benefits of dental implants compared with the alternatives: bridges and partial and full dentures.
Hygienists, share the benefits of dental implants (Box 5.1) with your patients. Explain how it is possible to restore their smile and function to its most natural state; this is highly motivational to patients. Esthetics is the number one reason patients say “yes” to treatment; improved function in terms of chewing and tasting food ranks a close second. The nutritional health benefit of being able to chew more healthy foods, such as raw vegetables, opens up a variety of food options that the edentulous patient has had to give up and could not taste because everything tasted like plastic.
- Improved health through nutrition, digestion, taste, and appetite
- Implants look, feel, and function like natural teeth
- Increased bone density and facial structure preservation
- Improved esthetic appearance
- Improved ability to function without pain or gum irritation
- Improved retention for implant-retained removable denture
- Improved quality of life and increases life expectancy
What patient would not want the cosmetic effect of looking younger as an added benefit to function? Relate the benefits of maintaining and increasing the bone density for an “internal face lift,” preserving the patient’s facial structure. Functionally explain the benefits of better digestion and how ability to chew food enriches the patient’s quality of life and can extend the patient’s life expectancy (14–16). Other benefits include improved taste, appetite, and that dental implants are not susceptible to decay. This makes implants a very good option for a stable diabetic patients or other immune-compromised patients who are also at risk for dental decay.
The choice of dental implant allows the patient the most conservative option that does not compromise adjacent teeth. Once the adjacent teeth are prepped, tooth structure is removed to sustain a crown, and a bridge is fabricated, the failure rate and the risk of root canal treatment increase (17–18).
Bridgework and dentures address the cosmetic problem of missing teeth, but do not prevent bone loss in the long term. Dental implants maintain proper chewing function, stimulating the bone to keep it functional and healthy. The primary benefit is that implants look, feel, and function like natural teeth and help preserve the jaw structure by preventing atrophy from bone loss. Implant therapy is also the number one choice for improved quality of life. Many times there are several options with implant dentistry and the patient’s financial and lifestyle choices can be important factors in the final treatment plan.
Hygienists need to address and listen to the patient’s expectations for both esthetic appearance and choice of removable or nonremovable prosthesis. The dentist and surgeon will also make suggestions that hold a higher success rate and it may be necessary to compromise, but ultimately it is what the patient wants that is important. What are the alternatives and why should patients consider dental implants?
Alternatives
Understanding the alternatives and the options of implant tooth replacement therapy is essential for hygienists to be able to “plant the seed” with patients. There are many considerations in implant tooth replacement therapy: to maintain and increase bone density, preserving facial structure, and implant-supported prosthesis’ enhance appearance, restore normal eating, and improve removable denture retention.
The patient may not accept implant therapy the first time you have the conversation on the RBAs. It may be months, but one day the patient will be ready to move forward with the recommended treatment.
As a hygienist, you should familiarize yourself with the restorative options for tooth replacement therapy. Be able to explain the restorative options for implants and explain the alternatives of traditional tooth replacement therapy bridge, partial or traditional denture. These alternatives do not compare with the longevity, improved function, and most of all patient psychological results that implants can offer.
Bridges
The main advantage of a bridge for the patient is less treatment time to complete. It does fill in the space for esthetic purposes when it is seated, but over time the bone under the pontic will melt away (see Figure 5.2). When explaining this to a patient, refer to Box 5.2 on key points of tooth replacement with implants; the bone width decreases 25% and the height of the ridge decreases 4 mm just in the first year (4, 19). For the patient this will create a higher sense of urgency to have the implant placed as soon as possible after extraction.
Figure 5.2 Bridge; note the bone loss. Courtesy of Dr. Kevin Frawley.

Key points for hygienist to remember and quote to patients when having a conversation on tooth replacement with implants
- Bone width decreases 25% in the first year after a tooth is lost or extracted (4, 5).
- Bone height decreases 4 mm in the first year (4, 5).
- 40–60% of ridge width can be lost in first 2–3 years (6).
- 0.5–1% bone continues to resorb yearly for the patient’s life (7).
Of patients who were asked if they had known about the bone loss with missing teeth, and that implants basically stop the bone loss, most would have had an implant. When talking to patients about implants, refer to the point of having to cut into the healthy adjacent teeth for crowns to support the bridge, as well as the fact that tooth decay and endodontic failures can occur in the abutment teeth and cause the bridge to fail (17, 18). It is estimated that 15% of abutment teeth will require endodontic treatment, compared with natural teeth of 3% single crowns. The abutment teeth are also at greater risk for periodontal disease and bone loss complications. These complications have resulted in loss of abutment teeth at 30% in 14 years (5).
One of the key factors to compare a three unit bridge to an implant for single tooth replacement is cost over time. At first the bridge may seem like the better deal to the patient, with faster treatment and on average slightly lower cost than a single restored implant. However, if the patient presents f/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


