Chapter 5
Cardiac Arrhythmias
Cardiac arrhythmia, which refers to any variation in the normal heartbeat, includes disturbances in rhythm, rate, or the conduction pattern of the heart. Cardiac arrhythmias are present in a significant percentage of the population, many of whom will seek dental treatment. Most arrhythmias are of little clinical concern, for either the patient or the dentist; however, some can produce symptoms, and a few may be life-threatening. Potentially fatal arrhythmias can be precipitated by strong emotion such as anxiety or anger,< ?xml:namespace prefix = "mbp" />
General Description
Incidence and Prevalence
Cardiac arrhythmias are relatively common in the general population; and their prevalence increases with age. They occur more frequently in elderly persons, people with a long history of smoking, patients with underlying ischemic heart disease, and patients taking certain drugs or have various systemic diseases.
Little and associates
Etiology
Cardiac contractions are controlled by a complex system of specialized excitatory and conductive neuronal circuitry (
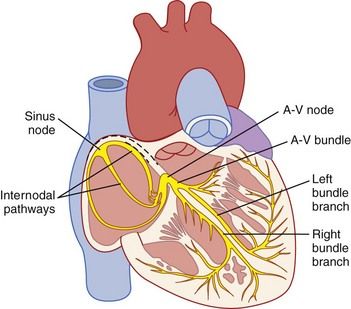
FIGURE 5-1 The electrical conduction system of the heart.
(From Hall JE: Guyton and Hall textbook of medical physiology, ed 12, Philadelphia, 2011, Saunders.)
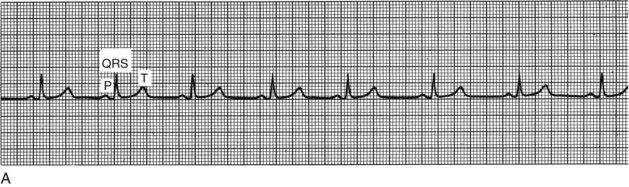
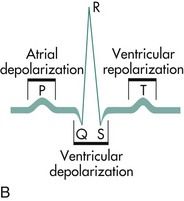
FIGURE 5-2 A, Electrocardiographic tracing of the cardiac cycle. B, Normal electrocardiographic deflections. The normal electrocardiogram consists of a P wave, representing atrial depolarization; a QRS complex, representing ventricular depolarization; and a T wave, representing rapid repolarization of the ventricles.
(A, From Goldberger AL, Goldberger E: Clinical electrocardiography: a simplified approach, ed 4, St. Louis, 1990, Mosby. B, From Pagana KD, Pagana TJ: Mosby’s manual of diagnostic and laboratory tests, ed 4, St. Louis, 2010, Mosby.)
Normal cardiac function depends on cellular automaticity (impulse formation), conductivity, excitability, and contractility. Disorders in automaticity and conductivity constitute the underlying cause of the vast majority of cardiac arrhythmias. Under normal conditions, the SA node is responsible for impulse formation, resulting in a sinus rhythm with a normal rate of 60 to 100 beats per minute.
Disorders of conductivity (block or delay) paradoxically may lead to rapid cardiac rhythm through the mechanisms of reentry. Reentry arrhythmias occur when accessory or ectopic pacemakers reexcite previously depolarized fibers before they would become depolarized in the normal sequential impulse pathway, typically producing tachyarrhythmias. The type of arrhythmia may suggest the nature of its cause. For example, paroxysmal atrial tachycardia with block suggests digitalis toxicity.
TABLE 5-1 Cardiac Arrhythmias Associated with Various Systemic Diseases
| Arrhythmia | Associated Systemic Conditions |
|---|---|
| Sinus bradycardia | Infectious diseases, hypothermia, myxedema, obstructive jaundice, increased intracranial pressure, myocardial infarction |
| Atrial extrasystoles | Congestive heart failure, coronary insufficiency, myocardial infarction |
| Sinoatrial block | Rheumatic heart disease, myocardial infarction, acute infection |
| Sinus tachycardia | Febrile illness, infection, anemia, hyperthyroidism |
| Atrial tachycardia | Obstructive lung disease, pneumonia, myocardial infarction |
| Atrial flutter | Ischemic heart disease, mitral stenosis, myocardial infarction, open heart surgery |
| Atrial fibrillation | Myocardial infarction, mitral stenosis, ischemic heart disease, thyrotoxicosis, hypertension |
| Atrioventricular block | Rheumatic heart disease, ischemic heart disease, myocardial infarction, hyperthyroidism, Hodgkin disease, myeloma, open heart surgery |
| Ventricular extrasystole | Ischemic heart disease, congestive heart failure, mitral valve prolapse |
| Ventricular tachycardia | Mitral valve prolapse, myocardial infarction, coronary atherosclerotic heart disease |
| Ventricular fibrillation | Blunt cardiac trauma, mitral valve prolapse, anaphylaxis, cardiac surgery, rheumatic heart disease, cardiomyopathy, coronary atherosclerotic heart disease |
TABLE 5-2 Drugs/Foods that Can Induce Cardiac Arrhythmias
| Cardiac Arrhythmia | Precipitating Drugs/Food Substance |
|---|---|
| Bradycardia | |
| Tachycardia | |
| Premature atrial beats | |
| Ventricular extrasystoles | |
| Ventricular tachycardia |
Pathophysiology and Complications
The outcome of an arrhythmia often depends on the nature of the arrhythmia and the physical condition of the patient. For example, a young healthy person with paroxysmal atrial tachycardia may have minimal symptoms, whereas an elderly patient who has heart disease with the same arrhythmia is at risk for developing shock, congestive heart failure, or myocardial ischemia. Furthermore, evidence suggests that patients with certain types of cardiac arrhythmias (e.g., AF) are susceptible to ischemic events within the dental office.
Arrhythmias are classified by site of origin (

Box 5-1 Classification of Common Cardiac Arrhythmias
Supraventricular Arrhythmias

Supraventricular Arrhythmias
Sinus Nodal Disturbances
• Sinus arrhythmia. Sinus arrhythmia is characterized by phasic variation in sinus cycle length.
• Sinus tachycardia. Tachycardia in an adult is defined as a heart rate greater than 100 beats per minute, with otherwise normal findings on the ECG.
• Sinus bradycardia. Bradycardia is defined as a heart rate less than 60 beats per minute, with an otherwise normal ECG tracing.
Disturbances of Atrial Rhythm
• Premature atrial complexes. Impulses arising from ectopic foci anywhere in the atrium may result in premature atrial beats. Premature atrial complexes, or contractions, occur frequently in otherwise healthy people but often occur during infection, inflammation, or myocardial ischemia.
• Atrial flutter. Atrial flutter is characterized by a rapid, regular atrial rate of 250 to 350 beats per minute. It is rare in healthy persons and most often occurs in association with septal defects, pulmonary emboli, mitral or tricuspid valve stenosis or regurgitation, or chronic ventricular failure.
• Atrial fibrillation. AF is the most common sustained arrhythmia in adults.
• Atrial tachycardias. Any tachycardia arising above the AV junction for which the ECG shows a P wave configuration different from that for sinus rhythm is called atrial tachycardia.
Tachycardias Involving the AV Junction
• Preexcitation syndrome (e.g., Wolff-Parkinson-White syndrome). The atria and ventricles are electrically insulated from each other by fibrous tissue that forms the anatomic AV junction. Normally, impulses are transmitted from atria to ventricles across this electrical bridge; however, in some persons, additional electrical bridges connect the atria and ventricles, bypassing the normal pathways and forming the basis for preexcitation syndromes such as Wolff-Parkinson-White syndrome.
Heart Block
• AV block. Heart block is a disturbance of impulse conduction that may be permanent or transient, depending on the underlying anatomic or functional impairment. Conduction impairment in heart block is classified by severity, with the various forms divided into three categories.
Ventricular Arrhythmias
• Premature ventricular complexes. Premature ventricular complexes (PVCs) (or contractions) are very common arrhythmias that are characterized by the premature occurrence of an abnormally shaped QRS complex (ventricular contraction), followed by a pause. PVCs may occur alone, as bigeminy (every other beat is a PVC), as trigeminy (every third beat is a PVC), or with higher periodicity. The combination of two consecutive PVCs is called a couplet; three or more in a row at a rate of 100 beats per minute are referred to as ventricular tachycardia.
• Ventricular tachycardia. The occurrence of three or more ectopic ventricular beats (PVCs) at a rate of 100 or more per minute is defined as ventricular tachycardia (VT). VT may be sustained or episodic. Sustained VT that persists for 30 seconds or longer may require termination because of hemodynamic instability. VT can quickly degenerate into ventricular fibrillation. A variant of VT called torsades de pointes is characterized by QRS complexes of changing amplitude that appear to twist around the isoelectrical line; this rhythm occurs at rates of 200 to 250 beats per minute.
• Ventricular flutter and fibrillation. Ventricular flutter and ventricular fibrillation (VF) are lethal arrhythmias characterized by chaotic, disorganized electrical activity that results in failure of sequential cardiac contraction and inability to maintain cardiac output.
Disorders of Repolarization
• Long QT syndrome. Long QT syndrome is a disorder of the conduction system in which the recharging of the heart during repolarization (i.e., the QT interval) is delayed. It is caused by a genetic mutation in myocardial ion channels and by certain drugs, or may be the result of a stroke. The condition can lead to fast, chaotic heartbeats, which can trigger unexplained syncope, a seizure, or sudden death.
Clinical Presentation
Signs and Symptoms
Arrhythmias may be symptomatic or asymptomatic; however, symptoms alone cannot be relied on to determine the seriousness of an arrhythmia. Some arrhythmias such as PVCs may be highly symptomatic, yet are not associated with an adverse outcome, whereas some patients with atrial fibrillation have no symptoms at all but may be at significant risk for stroke.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


