Sonic and Ultrasonic Instrumentation and Irrigation
Mechanism of Action of Power Scalers
Water contributes to three physiologic effects that play a role in the efficacy. These are acoustic streaming, acoustic turbulence, and cavitation. Acoustic steaming is the unidirectional fluid flow caused by ultrasound waves. Acoustic turbulence is created when the movement of the tip causes the coolant to accelerate, producing an intensified swirling effect. This turbulence continues until cavitation occurs. Cavitation is the formation of bubbles in water caused by the high turbulence. The bubbles implode and produce shock waves in the liquid, creating further shock waves throughout the water. In vitro, the combination of acoustic streaming, acoustic turbulence, and cavitation has been shown to disrupt microflora.52,83–85
Type and Benefit of Power Instruments
Sonic units work at a frequency of 2000 to 6500 cycles per second and use a high- or low-speed air source from the dental unit. Water is delivered via the same tubing used to deliver water to a dental handpiece. Sonic scaler tips are large in diameter and universal in design. A sonic scaler tip travels in an elliptical or orbital stroke pattern. This stroke pattern allows the instrument to be adapted to all tooth surfaces. Box 47-1 outlines the advantages and disadvantages of mechanized instruments as compared to manual instruments.
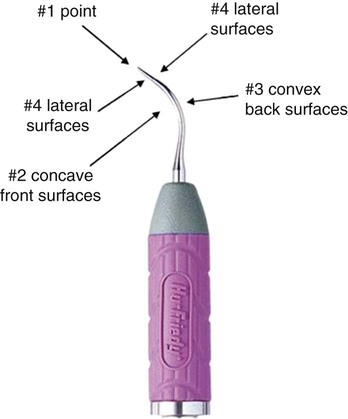
Magnetostrictive ultrasonic devices work in a frequency range of 18,000 to 50,000 cycles per second (Figures 47-1 and 47-2). Metal stacks that change dimension when electrical energy is applied power magnetostrictive technology. Vibrations travel from the metal stack to a connecting body that causes the vibration of the working tip. Tips move in an elliptical or orbital stroke pattern. This allows the tip four active working surfaces (Figure 47-3).
Piezoelectric ultrasonic units work in a frequency range of 18,000 to 50,000 cycles per second (Figure 47-4). They have ceramic discs that are located in the handpiece power piezoelectric technology. They change in dimension as electrical energy is applied to the tip. Piezoelectric tips move in a linear pattern, giving the tip two active surfaces (Figure 47-5). A variety of insert tip designs and shapes are available for use.
Tip Designs
There are tips designed to remove heavy supragingival calculus or to definitively debride periodontal pockets. Large diameter tips are created in a universal design and are indicated for the removal of large, tenacious deposits. A high power setting is generally recommended. Thinner diameter tips may be site specific in design. The straight tip design is ideal for use in treating patients with gingivitis and deplaquing maintenance patients (Figure 47-6). The right and left contra-angled instruments allow for greater access and adaptation to root morphology. These inserts are designed to work in a low power setting. They can be used for exploration. The amount of water delivered for lavage can be controlled through the selection of either traditional flow or a focused tip delivery flow. Contra-angled designs and larger, ergonomic grips enhance comfort and ergonomics (Figures 47-7 and 47-8).
Clinical Outcomes of Power-Driven Instruments
Numerous clinical outcomes have been evaluated from the use of power-driven instruments. A systematic review of the literature on the treatment of chronic periodontitis found no difference in the efficacy of subgingival debridement using ultrasonic/sonic scalers versus hand instruments in the treatment of single-rooted teeth. A benefit for multirooted teeth could not be determined because of a lack of clinical data.81 Likewise, a review by the American Academy of Periodontology found no differences in outcomes between sonic, magnetostrictive, and piezoelectric scalers.28
It is well established that power-driven instruments remove biofilms, bacteria, and calculus through mechanical action.* With the advent of new designs and thinner tips, deplaquing of root surfaces may be effectively accomplished by power-scalers.2,28,80 Both sonic and ultrasonic instruments have been shown to be effective in removing calculus similar to hand instrumentation.* Ultrasonic instruments through high-speed action produce a cavitational activity and acoustic microstreaming that some believe may help enhance the disruption of the bacteria in subgingival biofilms.
The primary expected clinical outcomes from scaling and root planing are a reduction in bleeding and probing depth and a gain in clinical attachment. In comparing power scalers to hand instruments, both types demonstrate similar outcomes for reductions in bleeding on probing and probing depth and gains in clinical attachment (see Table 47-1).†
TABLE 47-1
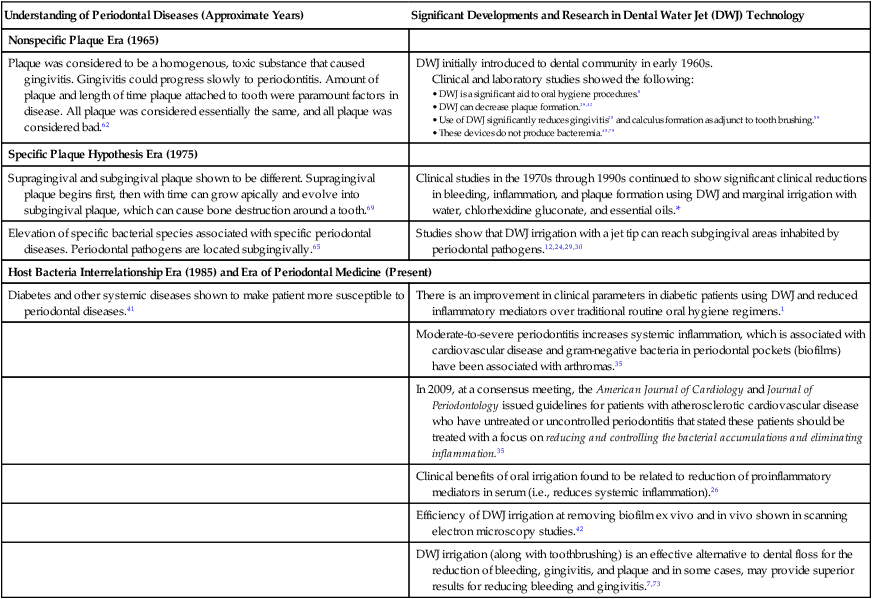
Increased Understanding of the Benefits of a Dental Water Jet
| Understanding of Periodontal Diseases (Approximate Years) | Significant Developments and Research in Dental Water Jet (DWJ) Technology |
| Nonspecific Plaque Era (1965) | |
| Plaque was considered to be a homogenous, toxic substance that caused gingivitis. Gingivitis could progress slowly to periodontitis. Amount of plaque and length of time plaque attached to tooth were paramount factors in disease. All plaque was considered essentially the same, and all plaque was considered bad.62 | DWJ initially introduced to dental community in early 1960s. Clinical and laboratory studies showed the following: • DWJ is a significant aid to oral hygiene procedures.8 • DWJ can decrease plaque formation.39,42 • Use of DWJ significantly reduces gingivitis20 and calculus formation as adjunct to tooth brushing.59 |
| Specific Plaque Hypothesis Era (1975) | |
| Supragingival and subgingival plaque shown to be different. Supragingival plaque begins first, then with time can grow apically and evolve into subgingival plaque, which can cause bone destruction around a tooth.69 | Clinical studies in the 1970s through 1990s continued to show significant clinical reductions in bleeding, inflammation, and plaque formation using DWJ and marginal irrigation with water, chlorhexidine gluconate, and essential oils.* |
| Elevation of specific bacterial species associated with specific periodontal diseases. Periodontal pathogens are located subgingivally.65 | Studies show that DWJ irrigation with a jet tip can reach subgingival areas inhabited by periodontal pathogens.12,24,29,30 |
| Host Bacteria Interrelationship Era (1985) and Era of Periodontal Medicine (Present) | |
| Diabetes and other systemic diseases shown to make patient more susceptible to periodontal diseases.41 | There is an improvement in clinical parameters in diabetic patients using DWJ and reduced inflammatory mediators over traditional routine oral hygiene regimens.1 |
| Moderate-to-severe periodontitis increases systemic inflammation, which is associated with cardiovascular disease and gram-negative bacteria in periodontal pockets (biofilms) have been associated with arthromas.35 | |
| In 2009, at a consensus meeting, the American Journal of Cardiology and Journal of Periodontology issued guidelines for patients with atherosclerotic cardiovascular disease who have untreated or uncontrolled periodontitis that stated these patients should be treated with a focus on reducing and controlling the bacterial accumulations and eliminating inflammation.35 | |
| Clinical benefits of oral irrigation found to be related to reduction of proinflammatory mediators in serum (i.e., reduces systemic inflammation).26 | |
| Efficiency of DWJ irrigation at removing biofilm ex vivo and in vivo shown in scanning electron microscopy studies.42 | |
| DWJ irrigation (along with toothbrushing) is an effective alternative to dental floss for the reduction of bleeding, gingivitis, and plaque and in some cases, may provide superior results for reducing bleeding and gingivitis.7,73 | |
Special Considerations
Furcations present one of the greatest scaling challenges. In many instances, the opening of the furcation is narrower than the conventional hand instrument. For this reason, power scalers may be recommended as a means to improve access when scaling furcations (see Table 47-2).
TABLE 47-2
Reduction of Inflammation and Plaque Biofilm
| Study | Duration | N | Agent Used | % Bleeding Reduction | % Gingivitis Reduction | % Plaque Biofilm Reduction |
| Al-Mubarak et al1 | 3 months | 50 | Water | 43.8 | 66.9 | 64.9 |
| Barnes et al8 | 4 weeks | 105 | Water | 36.2-59.2 | 10.8-15.1 | 8.8-17.3 |
| Brownstein et al16 | 8 weeks | 44 | CHX (0.06%) | 52-59 | 25.4-31.1* | 14.3-19* |
| Water | NR | NR | ||||
| Burch et al17 | 2 months | 47 | Water | 57.1-76.6 | NR | 52-55.7 |
| Chaves et al20 | 6 months | 105 | CHX (0.04%) | 54 | 26 | 35 |
| Water | 50 | 26 | 16 | |||
| Ciancio et al21 | 6 weeks | 61 | Essential oils† | 27.6 | 54-55.7 | 23-24 |
| Water and alcohol 5% | 13.6-31.2 | 59.8-61.9 | 9/6-13.3 | |||
| Cutler et al26 | 2 weeks | 52 | Water | 56 | 50 | 40 |
| Flemmig et al34 | 6 months | 175 | CHX (0.06%) | 35.4 | 42.5 | 53.2 |
| Water | 24 | 23.1 | 0.1 | |||
| Flemmig et al33 | 6 months | 60 | Acetylsalicylic acid 3% | 8.9 | 55.6 | |
| Water | 50 | 29.2 | 0 | |||
| Felo et al31 | 3 months | 24 | CHX (0.06%) | 62 | 45 | 29 |
| Fine et al32 | 6 weeks | 50 | Essential oils† | 14.8-21.7 | NR | 36.8-37.7 |
| Water | 7.5-10.6 | NR | 15.5-18.4 | |||
| Jolkovsky et al50 | 3 months | 58 | CHX (0.4%) | NR | 33.1 | 51.6 |
Stay updated, free dental videos. Join our Telegram channel
VIDEdental - Online dental courses
 Get VIDEdental app for watching clinical videos
Get VIDEdental app for watching clinical videos

|