Signs and symptoms
Key Points
This chapter alphabetically summarizes a range of the more important medical conditions.
Abdominal Pain
Abdominal pain is common and often due to gastroenteritis. Acute and severe pain may be a symptom of more serious intra-abdominal disease, from inflammatory bowel disease to various ‘surgical emergencies’ (‘acute abdomen’); this includes appendicitis, intestinal obstruction, perforated peptic ulcer, perforated diverticulitis, ectopic pregnancy, twisted ovarian cyst, dissecting abdominal aneurysm, mesenteric embolism or thrombosis, biliary tract disease, pancreatitis and renal stone. A leaking abdominal aneurysm is an emergency.
Gangrene and intestinal perforation can follow as little as 6 hours after interruption of the intestinal blood supply from appendicitis, a strangulating obstruction or arterial embolism – and can lead to potentially fatal peritonitis.
Alopecia
Alopecia (hair loss) may be temporary and caused, for example, by radiotherapy, cytotoxic chemotherapy, other drugs (e.g. anticoagulants, retinoids, beta-blockers and oral contraceptives) or tinea capitis (ringworm). More permanent alopecia may be:
Autoimmune diseases, particularly lupus erythematosus, may also cause hair loss, as may factitious (self-induced) hair-pulling.
Amenorrhoea
Amenorrhoea – absence of menstruation (menses) – is pathological, except before puberty, during pregnancy or early lactation, and after the menopause. Amenorrhoea may be caused by anatomical abnormalities, endocrine dysfunction (hypothalamic, pituitary, adrenal, thyroid, anorexia nervosa or other), cirrhosis, chemo- or radio-therapy, ovarian failure or genetic defects.
Amenorrhoea is either primary (menarche has not occurred by age 16) or secondary (menses have not occurred for 3 or more months in women who have had menses).
Anaemia
Anaemia is a reduction in the haemoglobin level for an individual’s age and sex. Anaemia may be normocytic, microcytic or macrocytic, according to the cause (Ch. 8).
Angina Pectoris
See ‘Chest pain’ and Chapter 5.
Anorexia
Anorexia, or loss of appetite, is a non-specific symptom seen in many conditions, but notably in malignant disease (Ch. 22), chronic infections and eating disorders (Ch. 27).
Anosmia
Anosmia (loss of the sense of smell) is usually due to nasal occlusion from the common cold, rhinitis, hay fever or nasal polyps. Some loss of smell may be normal with ageing but medications may change or impair the ability to detect odours. Anosmia can also arise from damage to olfactory nerves after head injury, radiotherapy or viral infections. Systemic causes include cerebrovascular events, Alzheimer dementia, tabes (syphilis), brain tumours, and many endocrine, nutritional and nervous disorders.
Anxiety
Anxiety is common, and may be normal or part of a psychiatric disorder (Ch. 10), but it may also be caused by stimulant drugs such as amphetamines, caffeine, cocaine, ecstasy and many others – or by their withdrawal; neurological disorders (brain trauma, infections, inner ear disorders); cardiovascular disorders (cardiac failure, arrhythmias); endocrine diseases (adrenal or thyroid hyperfunction, hypoglycaemia, phaeochromocytoma); or respiratory diseases (asthma, chronic obstructive pulmonary disease).
Aphasia
Aphasia is a language disorder that impairs both expression and understanding of language, as well as reading and writing. Aphasia results from damage to the left cerebral hemisphere, often as the result of a stroke, injury or tumour. Speech disorders such as dysarthria or apraxia of speech, which also result from brain damage, may be associated.
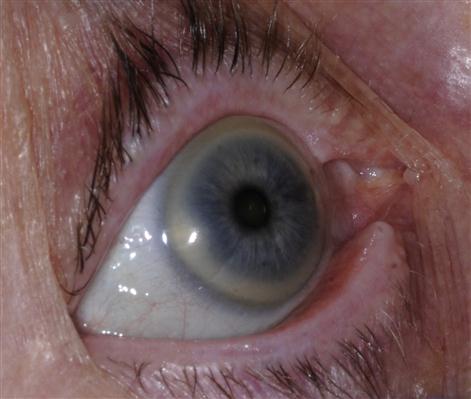
Arcus (Corneal Arcus)
Corneal arcus (arcus senilis) is a white or grey ring in the eyes due to cholesterol deposits in the cornea (Fig. 4.1); it is seen mainly in older age groups. These rings cause no visual problems but can indicate a problem with cholesterol metabolism – and an increased risk of ischaemic heart disease. Corneal arcus not only is associated with high cholesterol levels, but also can be seen in people with diabetes or hypertension, or those who smoke tobacco.
Arrhythmias
See Chapter 5.
Ascites
Ascites is the accumulation of fluid in the peritoneal cavity, either from peritoneal sources (bacterial, fungal or parasitic disease; cancer [malignant ascites]; endometriosis or starch peritonitis) or from extraperitoneal sources (cirrhosis, congestive heart failure, hypoalbuminaemia, myxoedema or ovarian disease, e.g. Meig syndrome).
Ataxia
Ataxia is incoordination or clumsiness of movement that has a cerebellar, vestibular or sensory (proprioceptive) origin rather than being the result of muscle weakness. In ataxia, movement is uncoordinated – defined as an inability to coordinate movements finely. Causes include: drugs (e.g. alcohol, aminoglutethimide, anticholinergics, phenytoin, carbamazepine, phenobarbital and tricyclic antidepressants); stroke or transient ischaemic attack (TIA); multiple sclerosis; head trauma; poisoning; and hereditary conditions (congenital cerebellar ataxia, Friedreich ataxia, ataxia telangiectasia). Ataxia may also follow infection (typically chickenpox or encephalitis).
Cerebellar ataxia is produced by lesions of the cerebellum or its afferent or efferent connections in cerebellar peduncles, pons or red nucleus.
Vestibular ataxia is produced by lesions anywhere along the eighth nerve pathway from labyrinth to brainstem or in the vestibular nuclei. Viral labyrinthitis is a typical cause. Nystagmus is frequently present, typically unilateral, and most pronounced on gaze away from the side of vestibular involvement. Vestibular ataxia is also gravity-dependent – incoordination of limb movements cannot be demonstrated when the patient is examined lying down but only when the patient attempts to stand or walk.
Sensory ataxia can result from abnormalities anywhere along the afferent pathway from peripheral nerve to the parietal cortex. Clinical findings include defective joint position and vibration sense in the leg and sometimes the arms, unstable stance with Romberg sign (sways with eyes shut), and a gait of slapping quality.
Back Pain
Back pain is a very common complaint; nearly four out of five people experience it at some time. Most cases do not have a definable cause but sedentary jobs and lifestyles predispose, as can obesity, or strenuous sports such as football and gymnastics. Women who have been pregnant, smokers, and workers who repetitively lift heavy objects are all at greater risk of back pain.
Bleeding Tendencies
Prolonged bleeding usually has a local cause such as excessive operative trauma (Ch. 5). Other causes include: haemorrhagic disease; anticoagulants; uncontrolled hypertension; and aspirin or other drugs that interfere with platelet function.
Blindness
See ‘Visual impairment’.
Bradycardia
Bradycardia (slow pulse rate) may have intrinsic or extrinsic causes (Ch. 5).
Intrinsic causes include: myocardial infarction, ischaemia or idiopathic degeneration; infiltrative diseases (sarcoidosis, amyloidosis or haemochromatosis); collagen diseases; myotonic muscular dystrophy; surgical trauma; and endocarditis.
Extrinsic causes include: autonomically mediated syndromes (vomiting, coughing, micturition, defecation, etc.); carotid-sinus hypersensitivity from vagal hypertonicity; drugs (beta-adrenergic blockers, calcium-channel blockers, clonidine, digoxin, antiarrhythmic agents); hypothyroidism; hypothermia; neurological disorders (affecting the autonomic nervous system); and electrolyte imbalances (hypokalaemia, hyperkalaemia).
Cervical Lymph Node Enlargement
See ‘Lymphadenopathy’.
Chest Pain
Angina and myocardial infarction (acute coronary syndromes) are the main causes of acute chest pain (Table 4.1; Ch. 5).
Table 4.1
Main causes of acute chest pain
| Cause of pain | Features | Predisposing factors |
| Myocardial infarction | Severe persistent crushing retrosternal pain, possibly radiating to left arm. Unrelieved by glyceryl trinitrate. May be accompanied by nausea or vomiting | Coronary heart disease Hypertension |
| Angina pectoris | Retrosternal pain, possibly radiating to left arm. Often previously experienced. Relieved in 3 min by glyceryl trinitrate | Coronary heart disease Hypertension |
| Acute abdominal pain | Pain location is of particular importance. Depending on cause, there may be concomitant symptoms such as gastro-oesophageal reflux, nausea, vomiting, diarrhoea, constipation, jaundice, melaena, haematuria, haematemesis, weight loss, and mucus or blood in stool | Serious causes: ruptured abdominal aortic aneurysm, perforated viscus, mesenteric ischaemia, ruptured ectopic pregnancy, intestinal obstruction, appendicitis, pancreatitis |
| Dissecting aneurysm | Sudden severe chest or upper back pain, often described as tearing, ripping or shearing sensation that radiates down back, loss of consciousness, shortness of breath | Men between 40 and 70 y |
| Oesophagitis | Low retrosternal pain on lying down or stooping. Improved by antacids | Hiatus hernia |
| Anxiety (hyperventilation) | Anxious patients with precordial pain. Overbreathing, panic and precordial pain | Stress |
| Trauma | Obvious history | – |
| Lung infection or tumour | Pain on inspiration. May be accompanied by dyspnoea or cough | Pneumonia |
| Pleurisy | ||
| Bronchogenic carcinoma |
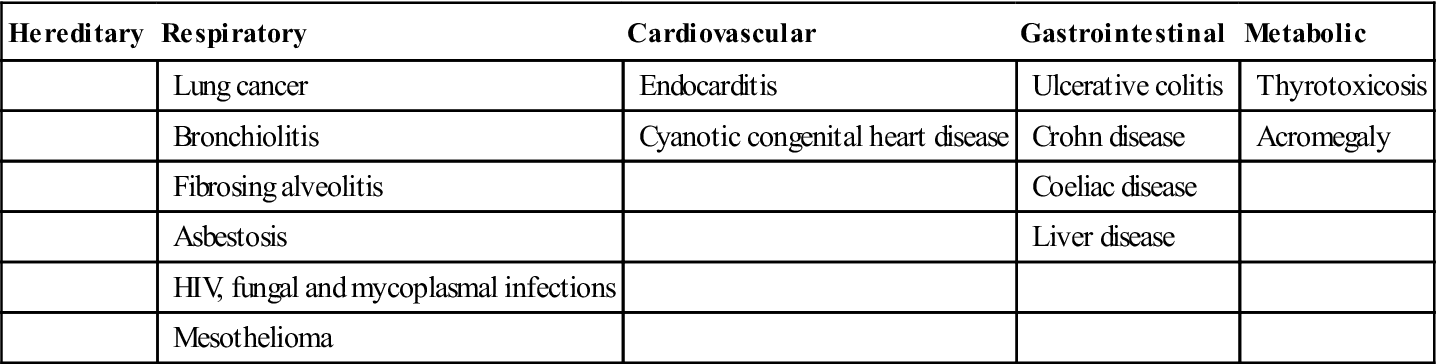
Clubbing of Fingers
Finger-clubbing is enlargement of the end of the digits. The cause is uncertain but might be hypoxia and circulating hormones such as erythropoietin. Clubbing can be hereditary but is usually acquired (Table 4.2).
Table 4.2
< ?comst?>
| Hereditary | Respiratory | Cardiovascular | Gastrointestinal | Metabolic |
| Lung cancer | Endocarditis | Ulcerative colitis | Thyrotoxicosis | |
| Bronchiolitis | Cyanotic congenital heart disease | Crohn disease | Acromegaly | |
| Fibrosing alveolitis | Coeliac disease | |||
| Asbestosis | Liver disease | |||
| HIV, fungal and mycoplasmal infections | ||||
| Mesothelioma |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Coma
A coma is profound unconsciousness in which the person is alive but unable to react or respond to stimuli. Coma results from central nervous system (CNS) diseases and conditions that affect CNS function, especially brain trauma, stroke, tumour, epilepsy, infection (e.g. meningitis), metabolic abnormalities (diabetic coma, ketoacidosis or electrolyte abnormality – hypernatraemia, hypercalcaemia), intoxication (e.g. alcohol, drugs of abuse, analgesics, anticonvulsants, antihistamines, benzodiazepines, digoxin, heavy metals, hydrocarbons, barbiturates, insulin, lithium, organophosphates, phencyclidine, phenothiazines, salicylates or tricyclic antidepressants), shock, hypoxia or hypotension (arrhythmia, heart failure).
Persistent coma is termed the vegetative state. Level of consciousness is assessed by the Glasgow Coma Scale (Ch. 24).
Confusion
The confused patient has fluctuating consciousness and impaired orientation and short-term memory, and is usually more confused at night. Causes are multiple and include old age, dementia and most of the causes of coma. See also “delirium”. Delusions or hallucinations can cause severe agitation. The confused patient should receive immediate medical attention since brain damage may result from many of the causes (see ‘Coma’). Confusional states need to be differentiated from dementia, in which there are similar disturbances of orientation and memory, with unimpaired consciousness.
Constipation
Constipation is the passage of small amounts of hard, dry faeces, usually fewer than three times a week. If they do not have a bowel movement every day, some people believe they are constipated or irregular – but there are no criteria for ‘normal’. Constipation is the most common gastrointestinal complaint.
Common causes include: lifestyle habits; inadequate dietary fibre, liquids or exercise; changes in life or routine, such as pregnancy, older age and travel; abuse of laxatives; or ignoring the urge to have a bowel movement. Codeine, opioids, antacids that contain aluminium, antispasmodics, antidepressants, iron supplements, diuretics and anticonvulsants may be implicated. More important but less common causes include colorectal disease (obstruction, scar tissue [adhesions]), diverticulosis, tumours, strictures, irritable bowel syndrome and Hirschsprung disease. Constipation may also be caused by systemic disease, such as neurological disorders (multiple sclerosis, Parkinson disease, chronic idiopathic intestinal pseudo-obstruction, stroke, spinal cord injuries), metabolic and endocrine conditions (diabetes, thyroid dysfunction, uraemia), or immunological disorders (amyloidosis, lupus, scleroderma).
Cough
A cough is a sudden, voluntary or involuntary, explosive expiratory manœuvre that intends to clear material (sputum) from the airways. Transient cough may simply be a mechanism to expel mucus or an inhaled foreign body. Cough is typical of respiratory, and sometimes of cardiac, disorders. Angiotensin-converting enzyme inhibitors (ACEIs) may also produce a cough.
A morning cough persisting until sputum is expectorated typifies chronic bronchitis. A cough that is provoked by exposure to cold air or during exercise may suggest asthma. Cough associated with rhinitis or wheezing or that is seasonal may be allergic. Cough induced by postural change may suggest chronic lung abscess, tuberculosis, bronchiectasis or a tumour. Cough associated with eating suggests a swallowing disturbance, or possibly pharyngeal pouch or tracheo-oesophageal fistula. A persistent cough should be taken seriously and tumours and infections excluded. See also “haemoptysis”
Cyanosis
Cyanosis is a bluish or purplish tinge to the skin due to very low oxygen saturation (SaO2) and thus excess reduced (deoxygenated) haemoglobin. Approximately 5 g/dL of reduced haemoglobin has to be present in the capillaries to generate the dark blue colour of cyanosis. For this reason, patients who are anaemic may be hypoxaemic without showing any cyanosis.
Peripheral cyanosis is a dusky or bluish tinge to the fingers and toes. When unaccompanied by hypoxaemia, it is caused by peripheral vasoconstriction as in the cold, especially in Raynaud disease.
Central cyanosis (where the colour is also seen in the lips or the mouth) is more serious and is usually an indication of hypoxaemia because of cardiac failure or respiratory disease, or both in cor pulmonale. Many factors, from natural skin pigment to room lighting, can affect detection of cyanosis and, if hypoxaemia is suspected, measurement of the oxygen level is necessary (arterial blood gas determination, pulse oximetry). Central cyanosis is an indication of gross hypoxia; such patients needing conscious sedation must be dealt with in hospital.
Delirium
Delirium is a state of mental confusion, caused by a disturbance in normal brain functioning, which develops quickly and usually fluctuates in intensity. More frequent in older people, delirium affects 1 in 10 hospitalized patients and is common in many terminal illnesses.
In contrast to dementia, delirium appears quickly, in hours or days, with a fluctuating level of consciousness. There may be limited awareness of the environment; confusion or disorientation (especially of time); memory impairment, especially of recent events; hallucinations, illusions and misinterpreted stimuli; mood disturbance, possibly including anxiety, euphoria or depression; and language or speech impairment. There are many possible causes of delirium, including:
Dementia
Dementia is a progressive loss of mental ability, including the ability to remember, think and reason (Ch. 10). The most common features include changes in memory, behaviour, mood and personality, and difficulty in communicating or understanding. Alzheimer disease is the most common form and responsible for about 50% of cases. Vascular dementia is the second leading cause and is a result of several TIAs. Other causes include parkinsonism, Huntington disease, human immunodeficiency virus (HIV) infection and Creutzfeldt–Jakob disease. Dementia may be reversible if caused by brain diseases or conditions such as tumours, depression or alcoholism.
Diarrhoea
Diarrhoea is defined as loose, watery stools passed more than three times in a day. Diarrhoea may be temporary, such as from an infection; this is common, usually lasts a day or two and resolves spontaneously. Prolonged diarrhoea can be a sign of other disorders, particularly intestinal disease such as infections: bacterial infections or toxins, such as preformed staphylococcal enterotoxin (from S. aureus) in contaminated food or water; viral infections; parasites; food intolerances (e.g. to lactose); drug reactions (such as to antibiotics like clindamycin, and antacids containing magnesium); intestinal diseases (inflammatory bowel disease, coeliac disease or irritable bowel syndrome); or after surgery (e.g. gastric surgery or cholecystectomy).
Where food hygiene is poor, diarrhoea can be life-threatening, especially if due to infections such as shigellosis (bacillary dysentery), Escherichia coli or cholera. The passing of blood in the stools is typical of severe diarrhoea – termed dysentery.
Diplopia
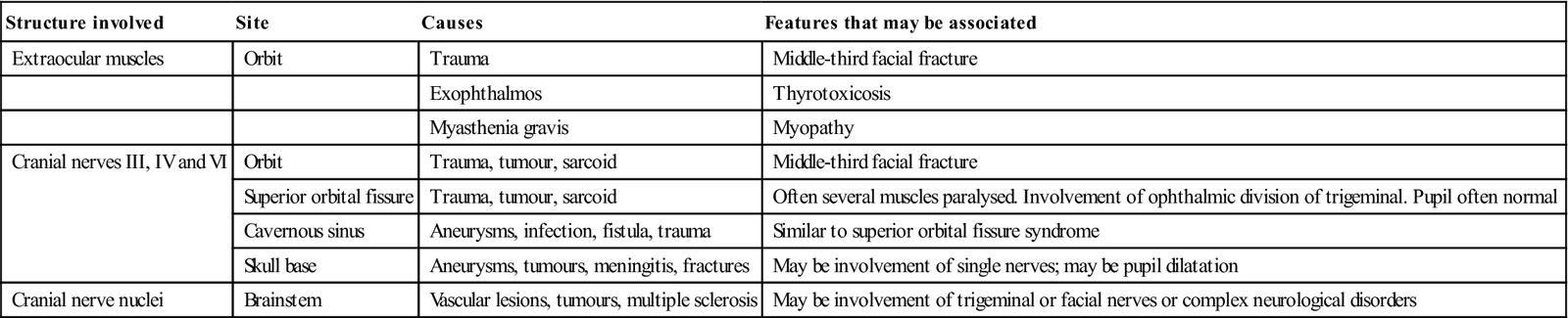
Double vision (diplopia) is the simultaneous perception of two images of a single object displaced horizontally, vertically or diagonally (i.e. both vertically and horizontally) in relation to each other. Diplopia is caused by misalignment of the eyes due to visual functional defects, mainly stemming from eye muscle or neurological disorders; by a structural defect in the eye’s optical system; or by drugs (e.g. alcohol, phenytoin, carbamazepine or lamotrigine). Diplopia may be an occasional transient complication of dental LA injections, presumably because anaesthetic tracks to the inferior orbital fissure, where it can block orbital nerves. Diplopia is not uncommon after maxillofacial or head trauma (from assault, accident and/or alcohol or drugs) but usually resolves spontaneously within a few days or weeks. Persistent diplopia after trauma can be caused by blow-out fractures of the floor of the orbit, entrapment of (or damage to) the orbital muscles or damage to the suspensory ligament to the frontal process or the zygomatic bone. Later fibrous adhesions between the orbital periosteum and coverings of the eye may cause permanent limitation of movement, as may injury to cranial nerves III, IV and VI (Table 4.3). Paralytic strabismus is characterized by variable deviation of the ocular axes according to the position of gaze and is the usual type of strabismus that follows maxillofacial injuries.
Table 4.3
< ?comst?>
| Structure involved | Site | Causes | Features that may be associated |
| Extraocular muscles | Orbit | Trauma | Middle-third facial fracture |
| Exophthalmos | Thyrotoxicosis | ||
| Myasthenia gravis | Myopathy | ||
| Cranial nerves III, IV and VI | Orbit | Trauma, tumour, sarcoid | Middle-third facial fracture |
| Superior orbital fissure | Trauma, tumour, sarcoid | Often several muscles paralysed. Involvement of ophthalmic division of trigeminal. Pupil often normal | |
| Cavernous sinus | Aneurysms, infection, fistula, trauma | Similar to superior orbital fissure syndrome | |
| Skull base | Aneurysms, tumours, meningitis, fractures | May be involvement of single nerves; may be pupil dilatation | |
| Cranial nerve nuclei | Brainstem | Vascular lesions, tumours, multiple sclerosis | May be involvement of trigeminal or facial nerves or complex neurological disorders |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Dizziness
Dizziness (vertigo) is a sensation of feeling unsteady or giddy, sometimes with a sensation of movement, spinning or floating. It is often due to disorders of the labyrinth. Movement of fluid in the semicircular canals signals the direction and speed of rotation of the head. Dizziness can also be due to central vestibular disorders (a problem in the brain or its connecting nerves); Ménière disease – an inner-ear fluid balance disorder that also causes fluctuating hearing loss and tinnitus (ringing in the ears); or perilymph fistula – a leakage of inner ear fluid to the middle ear. Dizziness can follow head injury or physical exertion; rarely, it has no known cause. Benign paroxysmal positional vertigo (a brief intense sensation of vertigo caused by a specific positional change of the head), labyrinthitis (inner ear infection) and vestibular neuronitis (a viral infection of the vestibular nerve) are other causes. Systemic disorders (vascular disorders) may occasionally be implicated.
Drooling
See ‘Sialorrhoea’.
Dry Mouth
Important causes of dry mouth (hyposalivation) are drugs, irradiation of major salivary glands, Sjögren syndrome and infections (Box 4.1). If dry mouth occurs when salivary flow is normal, it may be psychogenic. Smoking and alcohol use aggravate the complaint of dry mouth – xerostomia.
Dupuytren Contracture
Dupuytren contracture affects the hands and fingers, cause one or more finger, on one or both hands, to bend into the palm (Fig. 4.2). Apart from familial cases, diabetes, epilepsy, heavy smoking and heavy alcohol consumption have also been linked to the contracture.
Dysphagia
Swallowing is a process by which food and liquid move from the mouth, through the pharynx and then the oesophagus, and into the stomach. Each individual swallows 500–2000 times per day and swallowing also occurs during sleep. It is divided into three phases:
Cranial nerves IX to XII, and the pharyngeal muscles in particular, are essential to swallowing (Box 4.2). Dysphagia is ‘difficulty in swallowing’ (from the Greek dys meaning difficulty or disordered, and phagia ‘to eat’) and has many causes; older people in particular may develop swallowing dysfunction. This is due mainly to conditions such as cerebrovascular events or Parkinson’s disease. People with mental impairment often have cognitive and physiological impairments that may result in dysphagia.
Dysphagia may be secondary to defects in any stage of the swallowing process:
■ Neurological causes – may be fixed or progressive (Table 4.4)
■ Mechanical and obstructive causes:
◆ Infections, e.g. tonsillitis, dental abscess, tuberculosis
◆ Traumatic injuries to the face/neck
◆ Zenker diverticulum (pharyngeal pouch)
◆ medications affecting the oesophageal muscles, e.g. oxybutynin, tolterodine
Table 4.4
Neurological causes of dysphagia
| Non-progressive | Progressive |
| Cerebral palsy | Amyotrophic lateral sclerosis |
| Cerebrovascular events | Cerebrovascular events |
| Post-surgery | Dementia |
| Traumatic brain injury | Head and neck malignancies |
| Huntington disease | |
| Multiple sclerosis | |
| Muscular/myotonic dystrophy | |
| Myasthenia gravis | |
| Parkinson disease | |
| Supranuclear palsy |
Swallowing may be assessed by watching for signs of leakage from the mouth, facial weakness, poor muscular coordination, delayed pharyngeal/laryngeal elevation, choking, breathlessness and changes in voice quality after swallowing. The ‘gold standard’ is videofluoroscopy (VFS; modified barium swallow), in which radio-opaque barium liquid is swallowed by the patient and moving images of swallowing are captured. Fibreoptic endoscopic evaluation of swallowing (FEES) with nasoendoscopy has an advantage over VFS in that it is a bedside procedure with no radiation exposure.
Swallowing problems may lead to inhalation of either oropharyngeal or gastric contents into the airway. Aspiration may lead to chest infections, which are the leading cause of death in such people. The main risk of dysphagia is choking if the passage of air to the lungs is blocked by a foreign body; this is a precursor to asphyxiation. Signs of choking include coughing, gagging, inability to speak, breathe or cry, loss of consciousness and cyanosis. If the obstruction is not successfully removed, the patient is at risk from asphyxiation and ultimately death.
The major dental concern when treating patients with dysphagia is the risk of aspiration during treatment, which may lead to choking or aspiration pneumonia.
Dyspnoea
Dyspnoea is difficulty in breathing. Functional causes include anxiety, panic disorders and hyperventilation. Organic causes include cardiac and respiratory disorders and anaemia. Dyspnoea is typically exacerbated by exercise, but may occur at rest and persist or worsen when lying down (orthopnoea). Paroxysmal nocturnal dyspnoea (cardiac asthma) is a sudden attack of severe dyspnoea due to pulmonary oedema that wakes the patient from sleep with a terrifying sensation of suffocation.
Dysrhythmias
See Chapter 5.
Dysuria
Dysuria is the sensation of pain or burning on urination. It is more common in women than in men, and then bacterial cystitis (usually after intercourse) is the commonest cause. In men too, dysuria is usually a result of urinary tract infection – in younger patients most often caused by a sexually transmitted organism such as Chlamydia trachomatis. In those over 35 years, coliform bacteria predominate and infection typically results from urinary stasis secondary to prostatic hyperplasia.
Dysuria in either sex may occasionally be caused by renal calculus, genitourinary malignancy, spondyloarthropathy and medications.
Earache
As aircraft descend, pressure rises even in the normal middle ear, and this can cause excruciating pain. Earache (otalgia) is commonly due to middle ear infection (otitis media) and is especially common in children, often following a sore throat or cold. There is severe pain and often a temporary loss of hearing; with severe infections, the ear drum may perforate, causing a leakage of pus from the ear. Tumours in the middle ear are uncommon but include cholesteatoma. Pain may be referred to the ear from elsewhere, such as tongue cancer, the antra, dental abscesses and temporomandibular disorders.
Encopresis
Encopresis is the soiling of underwear with stool by children who are past the age of toilet training, but it is not considered a medical condition unless the child is at least 4 years old. A large amount of hard stool is in the intestine, and stool leaks around this mass and out through the anus. The best way to prevent encopresis is to avoid constipation by eating a varied diet with plenty of fruits and vegetables and wholegrain bread and cereals.
Epilepsy
See Chapter 13.
Epistaxis (Nosebleeds)
Most nosebleeds are caused by nose-picking, minor nose injuries, the common cold, or vigorous nose-blowing or sneezing. Rarely, they may be caused by a foreign body lodged in the nose, barotrauma, chemical irritants, drugs (e.g. anticoagulants, anti-platelet agents, non-steroidal anti-inflammatory drugs [NSAIDs] or vitamin E), maxillofacial or nasal surgery, hereditary telangiectasia or thrombocytopenia.
Erosion of Teeth
Tooth erosion can result from exposure to dietary acidic sources (carbonated drinks, citrus fruits and juices, pickles, vinegar, wine) or some drugs (e.g. chewable vitamin C); regurgitated gastric contents (anorexia nervosa, bulimia, gastro-oesophageal reflux or alcoholism); industrial sources (various acids); or, rarely, other sources (e.g. swimming-pool water).
Exophthalmos
See ‘Proptosis’.
Fainting (Vasovagal Syncope)
Syncope, commonly called fainting or ‘passing out’, is a temporary loss of consciousness due to a sudden decline of brain blood flow. Syncope can occur in otherwise healthy people and affects all age groups, but does so more often in older people. Vasovagal syncope is a reflex mediated by autonomic nerves in which there is splanchnic and skeletal muscle vasodilatation, bradycardia and thus diminished cerebral blood flow, leading to loss of consciousness. Fainting can be precipitated by psychological factors (e.g. pain, or fear at the sight of a needle or blood); postural changes; hypoxia; or carotid sinus syndrome. The latter is usually seen in older patients in whom mild pressure on the neck causes a vagal reaction, leading to syncope with bradycardia or cardiac arrest. Vasovagal syncope is treated by having the patient lie down with their legs raised (Ch. 1).
Recurrent syncope with complex associated symptoms in so-called neurally mediated syncope (NMS) is associated with any of the following: preceding or succeeding sleepiness, preceding visual disturbance (‘spots before the eyes’), sweating and light-headedness. Other types of syncope include:
Facial Paralysis
See Chapter 13.
Facial Sensory Loss
See Chapter 13.
Fever (Pyrexia)
Normal body temperature (37°C) has a diurnal rhythm, lower in the morning before dawn and higher in the afternoon. Temperature control activities balance heat loss and production. An abnormal rise in body temperature is caused by either hyperthermia or fever. In fever, the body temperature controls are functioning correctly, but the hypothalamic set point is raised by exogenous or endogenous pyrogens; temperature rises as the body responds to cytokines such as interleukin-1, produced by microorganisms or immunocytes.
The main causes of fever include: infections, tumours, drugs (e.g. chemotherapy drugs, biological response modifiers, and antibiotics such as vancomycin and amphotericin), neuroleptic malignant syndrome, blood transfusion reactions, connective tissue disorders, cerebrovascular events and or graft-versus-host disease.
Fever may, in children under 6 years, be complicated by seizures (febrile convulsions) and, in older persons when the hypothalamus temperature-regulating centres may function poorly, by arrhythmias, heart failure, cerebral hypoxia and confusion.
Gastrointestinal Bleeding
Bleeding in the digestive tract can be the result of many different conditions, some of which are life-threatening. Bleeding can sometimes be unnoticed (occult or hidden bleeding), but the faecal occult blood test (FOBT) checks stool samples for traces of blood, detecting bleeding from almost anywhere in the digestive tract. Causes of gastrointestinal bleeding, apart from drugs such as NSAIDs, include lesions in: the oesophagus (oesophagitis [hiatus hernia], varices, tears [Mallory–Weiss syndrome, after severe vomiting], cancer); the stomach (ulcers, gastritis, cancer); the small intestine (duodenal ulcer, inflammatory bowel disease); and the large intestine and rectum (haemorrhoids, infections, ulcerative colitis, diverticular disease, polyps or cancer).
The appearance of blood in the faeces depends upon the site and severity of bleeding. Bleeding from the oesophagus, stomach or duodenum can cause black or tarry stools (melaena). The stool may be mixed with darker blood if the bleeding is higher in the colon. Blood originating from the rectum or lower colon is bright red.
Vomited blood may be bright red or have the appearance of coffee grounds.
Endoscopy permits examination of the oesophagus, stomach, duodenum (oesophagoduodenoscopy), colon (colonoscopy) and rectum (sigmoidoscopy), and facilitates biopsies. Magnetic resonance imaging (MRI), computed tomography (CT), barium radiography, angiography, radionuclide scans and ultrasound can also be used to locate sources of chronic occult gastrointestinal bleeding.
Gingival Swelling
Gingival swelling may be localized or generalized. It is usually drug-induced gingival overgrowth (DIGO), but occasionally is due to a systemic disease (Box 4.3).
Localized
Congenital
Acquired
Epulides
Granulomatous conditions
Infections with human papillomavirus (HPV)
Tumours
Haematemesis
Haematemesis (blood in the vomit) typically results from blood regurgitation from the gastrointestinal tract (mouth, pharynx, oesophagus, stomach and small intestine). Conditions that cause haematemesis include bleeding ulcer(s), neoplasms, angiomas or varices in the stomach, duodenum or oesophagus; prolonged and vigorous retching, which may tear small blood vessels of the throat or oesophagus; drugs; and ingested blood (e.g. swallowed after a nosebleed) or gastroenteritis. It may be difficult to distinguish haematemesis from coughing up blood from the lung (haemoptysis) or a nosebleed (bloody postnasal drainage), but it can also cause blood in the stool.
Haematuria
Haematuria, blood in the urine, typically originates in the urinary tract (urethra, bladder or ureter) but, in wom/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



