4
Rational Basis for Transitioning from 2D to 3D Radiographic Imaging in Orthodontic Practice and Research
Introduction
The orthodontic profession has been successful in merging the dental, technical, and medical worlds. Publications in dental journals initially transferred one clinician’s experiences about treatment technologies to his or her colleagues. The “fathers of orthodontics” further developed the profession by sharing their experiences and descriptions of techniques without applying any basic rules of research.
Although clinicians initially attempted to raise the level of treatment through clinical trials, a research- or evidence-based approach to clinical practice did not exist yet. Indeed, of the approximately 50,000 papers with the keywords orthodontic or orthodontics published between 1912 and 2012, fewer than 6,000 were retrieved when the search was limited to clinical trials, randomized clinical trials, or animal experiments. The majority of the remaining manuscripts were written by orthodontists who were reporting their experiences or describing new clinical methods.
Following the introduction of the cephalostat in the United States by Broadbent (1931) and in Europe by Hofrath (1931), cephalometric studies dominated the literature. Almost 6,000 studies reported results from clinical trials, prospective or retrospective, and rarely randomized controlled studies, all based on cephalometric analyses. However, the two-dimensional (2D) measurements on which this research was based had inherent errors related to the 2D imaging of three-dimensional (3D) structures, as well as the projection of bilateral structures with different magnification onto one image. Thus the larger the distance from the anode to the film compared with that of the object to the film, the smaller the error. Due to the need to minimize irradiation and the footprint of the unit, however, the anode to film distances have been reduced from 240 cm to 190 cm to as low as 150 cm for most of the cephalostats used in the orthodontist’s offices today, while maintaining the object-to-film constant at 10 cm with each of these configurations. Thereby both types of flaws related to the images were increased.
The panoramic radiograph was the second contributor as a source of information on which the orthodontic problem list was developed and soon became a standard component of the diagnostic material. However, panoramic images also have caveats such as distortions and differences in magnification of the two sides resulting from the dissimilarities in object-film distance caused by asymmetry or asymmetrical positioning of the patient (Schulze et al., 2000).
After cephalograms were introduced into practice, a variety of analyses were developed in which measurements typically were performed on midsagittal structures and generally were limited to angles or proportions in order to minimize the influence of the inherent bias (Athanasiou, 1995). Norms for different populations made it possible to classify patients with malocclusions into different categories according to their skeletal and dentoalveolar presentation or future development. A number of databases were generated and consisted of cephalograms taken of untreated individuals annually or biannually; these recently were made available for public use by the American Association of Orthodontists Foundation (AAOF) Craniofacial Growth Legacy Collection (http://www.cril.org/aaof/aaof_home.asp).
By superimposing on the stable structures, it was possible to perform longitudinal studies illustrating normal and atypical growth patterns. It was, however, not until stable indicators were inserted into the maxilla and the mandible that it was possible to differentiate between displacements of the jaw due to sutural and condylar growth, and modeling of the individual bones and intramaxillary tooth movements. The detailed description of a series of radiographs of untreated individuals with the Bjork indicators deepened the understanding of the factors contributing to the post-natal development of the craniofacial skeleton, specifically in the sagittal plane of space (Bjork & Skieller, 1972). The transverse development was studied on postero-anterior (PA) headfilms (Athanasiou et al., 1992; Kapila et al., 2011), but few standard analyses have been developed specially for these projections. An attempt to obtain 3D information was proposed by combining the occlusal image of the study casts or virtual models with the profile image, but it still was far from the true 3D situation (Bjork & Skieller, 1974, 1977). Frontal and axial exposures were recommended when specific information in these planes of space was required and a reduction of the distortion of the lateral structures could be obtained by a 45° image in which the body of the mandible was positioned parallel to the film (Sakima et al., 2004).
In spite of the questionable validity and the low reproducibility of many of the applied variables, treatment plans traditionally have been developed based on a cephalometric analysis and study casts.
Although there are limitations related to the 2D imaging of 3D structures, several attempts to obtain 3D information by stereometry were made, although the approach never became part of a clinical routine (Baumrind et al., 1983a, 1983b). The need for real 3D images remained an important objective, however, and the use of fan-beam computed tomography (CT) was reported for specific problems such as treatment planning of patients suffering from craniofacial anomalies or particular types of ectopic teeth (Ericson & Kurol, 1987). Both the high doses of radiation and high costs limited the use of this method, but these concerns have been mitigated substantially when cone beam computed tomography (CBCT) was introduced to the dental community (Mozzo et al., 1998). As a result, CBCT is becoming an important component of the orthodontic armamentarium. Its role still is not well defined and there is little consensus regarding the indications for CBCT imaging within the field of orthodontics (Kapila et al., 2011; Halazonetis, 2012; Larson, 2012).
The purpose of this chapter is to present an objective assessment on the utility of CBCT imaging for clinical and research applications in orthodontics. More specifically, we discuss whether (1) CBCT can replace the conventional set of radiographs, (2) CBCT will lead to improvements in treatment relative to that performed with conventional radiography, (3) research based on CBCT will change the treatment approach, and (4) the fusion of CBCT with other 3D visualization modalities can enhance treatment and research.
Can CBCT Replace the Conventional Set of Radiographs?
The dynamic character of the CBCT image allows for the generation of distortion-free images in user-defined planes of space. Additionally, the parameters defined in the midsagittal plane of space from a lateral cephalometric radiograph obviously can be replicated by the CBCT images (Adams et al., 2004). The question then arises whether all parameters derived from 2D cephalometric images can be measured on reconstructions made from CBCT scans (Farman & Scarfe, 2006; Cattaneo et al., 2008). As the CBCT images allow for measurements of true distances and undistorted angles, the answer to the above question definitely is “yes,” but the question could be rephrased by replacing the word “can” with “should.” In that case, should a new set of cephalometric analyses be developed? Our answer here is “no.” To replace all headfilms indiscriminately with CBCT scans would be not only costly but also unethical. It also should be mentioned that anatomy is taught based on the observation of 3D structures and the education in cephalometrics is focused on describing 3D structures in 2D. Keeping the original anatomy intact rather than reducing it to a 2D derivation contributes to a better understanding of the CBCT image as well as that of the true anatomy and relationships of the craniofacial structures.
Although it has been almost universally accepted that orthodontic treatment is based on a plan that is generated following a clinical, a model, and a cephalometric analysis, the value of the latter has been questioned from time to time. Nijkamp and coworkers, (2008) demonstrated that important decisions regarding treatment rarely were influenced by cephalometric parameters. The ability to acquire valid 3D information, therefore, should not lead to the routine use of CBCT, which, as with cephalometric analyses of 2D headfilms, may be superfluous in making treatment decisions. The availability of undistorted 3D measurements should not necessarily call for a repetition of the multiplicity of analyses that describe morphological characteristics of various populations and/or determine the effects of different appliances with similar but true absolute values obtained from the 3D images.
Radiographs should be taken only when the findings are likely to have a decisive impact on the patient’s treatment plan (see Chapter 6). In other cases, the clinician should refrain from taking both conventional headfilm and CBCT. In this context, Kapila and colleagues (2011) listed the types of cases that could benefit from CBCT imaging, which include those requiring (1) precise assessment of root morphology and length, (2) detailed information regarding morphology of alveolar bone and interdental relationship, (3) morphometric analysis of craniofacial anomalies, (4) specific analysis of TMJ in health and disease, and (5) assessment of the airways. These recommendations, however, do not justify a routine replacement of headfilms with CBCT in clinical orthodontics today. As Kapila and associates (2011) suggested in concordance with several others (Kau et al., 2006, 2009; Hussain et al., 2008; DeVos et al., 2009), the possibility of obtaining 3D information should lead the orthodontist to define a new set of rules identifying where this type of imaging can benefit the individual patient. These sets of rules are discussed in depth elsewhere in this textbook (Chapters 1 and 6).
Will CBCT Lead to Improvement of Treatment?
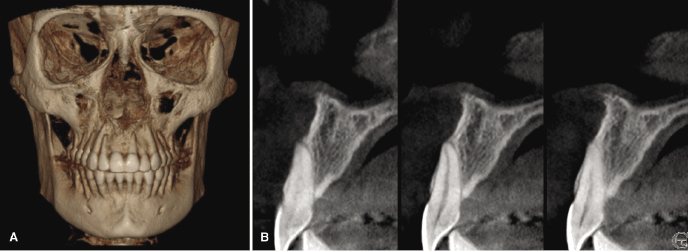
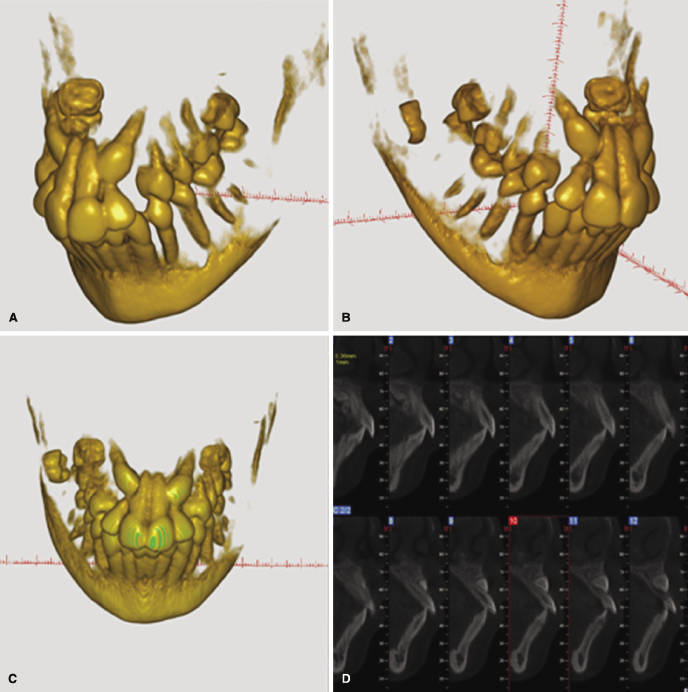
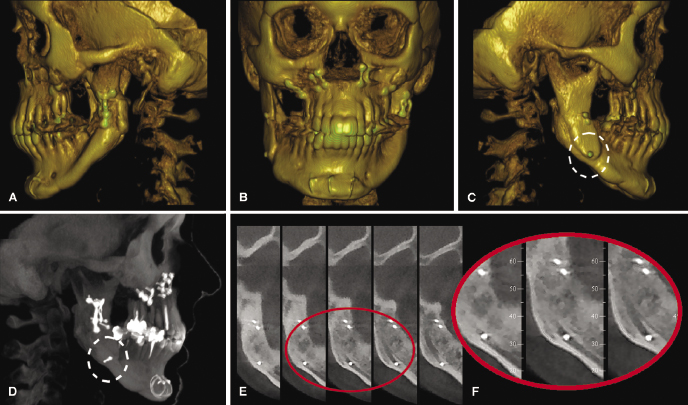
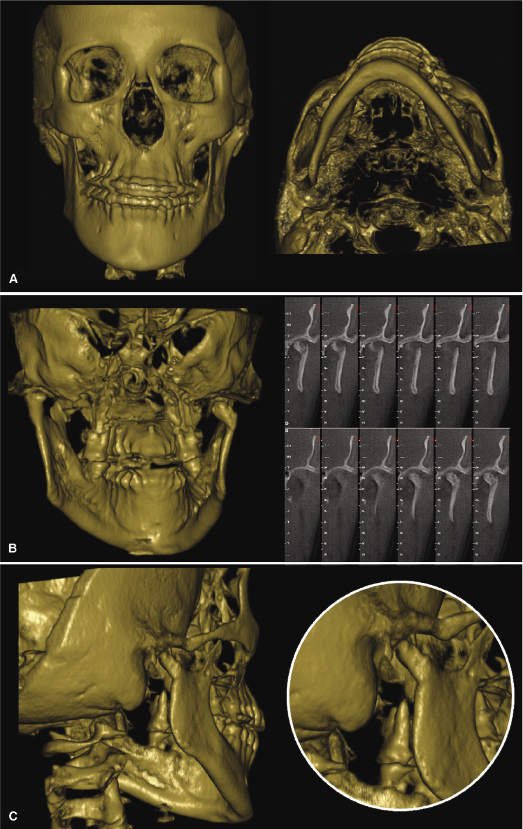
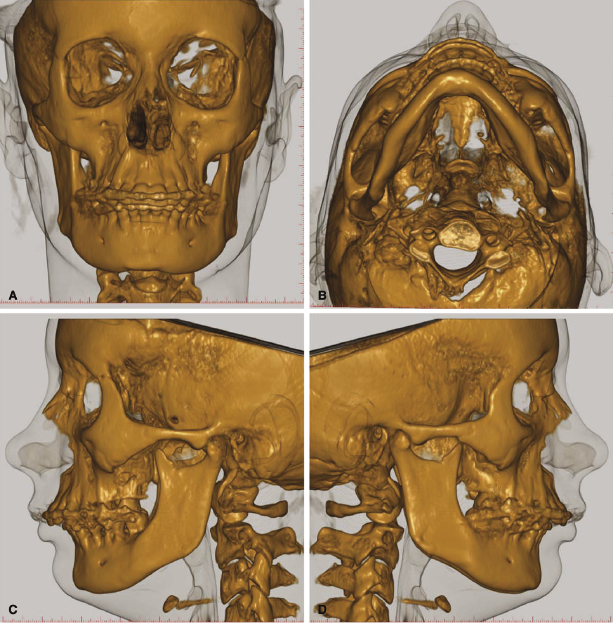
In relation to an orthodontic treatment, information derived from CBCT could influence the problem list, the treatment plan, and the evaluation of the treatment result. Specifically, CBCT can be valuable in refining or optimizing a problem list in several types of cases, including those requiring (1) information on the alveolar bone and risks of fenestrations that might result from eventual expansion (Figure 4.1; see also Chapter 14), (2) localization of ectopic teeth (Figure 4.2; see also Chapters 8 and 16), (3) determination of the cause of unexplainable symptoms (Figure 4.3), (4) assessment of morphology and position of the condyles in patients with temporomandibular joint disorders (TMJDs) and in the localization of asymmetries (Figure 4.4; see also Chapters 12 and 21), (5) description and quantification of anomalies in the craniofacial skeleton in all three planes of space using appropriate 3D coordinates (Figure 4.5; see also Chapter 23), and (6) the assessment of whether a skeletal problem can be camouflaged or needs surgery (Figure 4.6).
With regard to its applications to treatment planning, CBCT will be useful when defining the changes planned in 3D, whether dental, dentoalveolar, or skeletal. For dental movements, once these are defined in 3D, the force system needed can be determined and the biomechanically correct appliance designed as demonstrated for impacted teeth elsewhere in this book (Chapter 16). In cases of surgical interventions, a definition of the displacement of the bony units in 3D likewise can be of considerable help in the treatment planning process (see below and also Chapters 20 and 22).
In relation to quality control or assessing to what degree the chosen treatment approach has achieved the treatment goal, this is possible only if the treatment goal has been proactively defined, which frequently is not the case. CBCT or other 3D imaging technologies are likely to be the method of choice in future clinical studies in which 3D rather than 2D images will provide the required information on whether a pre-specified treatment goal has been achieved.
Will CBCT-Based Research Change the Treatment Approach?
Many prospective and numerous retrospective studies using cephalometrics have focused on comparing treatment results obtained from different treatment approaches. Due to ethical reasons including radiation exposure, many of these studies probably are not repeatable with CBCT imaging. However, the magnification and other adjustments necessary for performing valid comparisons between conventional and CBCT-constructed cephalometric images are possible. As the longitudinal radiographic records of the AAOF Legacy Project never will be repeated, the information held in this database regarding normal growth and development will serve as a valuable basis with which the results of CBCT-based trials can be compared.
Although cephalometric studies that assess the effect of various interventions can be repeated with a smaller error of the method, these studies should be performed only where it is expected that the data derived will be substantially more precise than what currently are available and would have a significant impact on clinical practice. On the other hand, it should not be considered lege artis to perform new clinical studies based on conventional 2D headfilms. Whereas an indiscriminate use of CBCT for routine clinical use can be questioned seriously, there is no doubt that clinical research that evaluates the results of different approaches to treatment will benefit from a well-planned prospective and, if possible, randomized controlled studies using CBCT images.
Until this point, CBCT imaging has had only limited impact on research. Most studies have been focused on the technology and its possible clinical uses; only a few randomized clinical trials have been published. Tai and colleagues (2010, 2011) analyzed the 3D changes generated with Schwartz appliances; Botticelli and coworkers (2011) assessed the influence of the 3D image on the treatment plan in a clinical trial on unerupted canines; and Cattaneo and associates (2011) performed a randomized clinical trial comparing the results of two different bracket systems on the expansion of the upper arch. Because CBCT imaging also allows for the identification of stable structures, it enables the differentiation between modeling, changes in shape of the individual bone related to growth and development and/or treatment, and displacement of bones due to sutural or condylar growth. Overall, CBCT allows for the effect of the treatment to be analyzed in great detail since orthopedic and orthodontic effects can be differentiated by superimposing on both internal and external stable structures (Cevidanes et al., 2005, 2009).
Can the Fusion of CBCT with Other 3D Visualization Modalities Enhance Treatment and Research?
Despite the advantages and new possibilities of CBCT imaging as a diagnostic, treatment planning, and evaluation tool, there are some inherent problems with CBCT scans. The most important is the inability to create smooth surfaces of anatomical structures in 3D reconstructions. The lower depth and contrast in gray values, as compared with conventional CT, makes it harder to distinguish between the different tissues. As a consequence, isolation of a particular tissue by segmentation of the gray values can result in surfaces that do not correspond to the true anatomy. This could be due to the presence of noise when the threshold value is set too low or holes when the threshold is too high. When making a 3D reconstruction of a skull from a CBCT dataset, a typical problem is that when a threshold value that gives a fair representation of the dental surfaces is chosen, it l/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


