Prosthodontics
Chapter Contents
Overview
The discipline of prosthodontics has evolved over the last decade from being a discipline heavily weighted to complete denture construction to a specialty concerned with removable, fixed, implant-supported prosthesis and maxillofacial prosthodontics. As people are living longer and retaining their dentitions into later life, the demands on the prosthodontist have changed to match the increasing demands of a changing population. This chapter addresses the clinical stages involved with complete and partial denture construction and highlights other areas of interest to the prosthodontist. Detailed information on material science, preprosthetic surgery and prosthetic laboratory techniques has not been included and indeed this text should be seen as an introduction and summary of the areas covered.
4.1 Complete dentures
Patient assessment
The evaluation of a patient who requires any form of dental treatment should begin at the earliest stage of meeting that patient. On an initial meeting with the patient, the points that should be subconsciously noted, even before any dialogue occurs, are the sex and age of the patient, their physical stature, the appearance they wish to present to the public and, finally, their present dental status. These brief thoughts about a new patient can often provide reliable predictions of the expectations of the patient and, based on that, the possible outcomes. Initial impressions of a new patient often give a very valuable insight into a patient’s potential expectations of the dental care. It is vitally important, nevertheless, not to categorise definitively patients as a result of initial impressions. A patient’s appearance and demure can be deceptive; therefore, a detailed history is required to give a broader, more structured assessment of the patient’s oral status, dental demands and psychological attitude towards treatment. A short but concise evaluation of the presenting complaint or reason for attendance is required, and in this respect it is important that the patient’s perspective of the problem is identified rather than considering what the clinician feels is wrong. Structured questioning should only begin after the patient has clearly indicated their reasons for attendance, complaints and any wishes they may have. A detailed dental history should then be built up gradually. Important features that must be gained from such a history are the following:
• When did you become edentulous?
• Why did you lose your teeth?
• Have you worn partial dentures or complete dentures previously?
• Did you have immediate dentures fitted?
• How many sets of dentures have you had?
• How long did each set of dentures last?
• Did you attend the dentist for any denture maintenance visits?
• How old is your present set of dentures?
• Which set of dentures was the most successful in your opinion?
• Do your present dentures cause you any discomfort?
• Do you wear your dentures at night?
A clear and concise medical history is also required with certain features being of particular note for denture wearers (Table 4.1).
Table 4.1
Important medical factors for denture wearers
| Area | Significant factors |
| Physical disabilities | Disability (mental or physical), arthritis |
| Neuromuscular disorders | Parkinson’s disease, epilepsy, stroke |
| Airway/breathing disorders | Asthma, bronchitis |
| Skin/mucosal disease | Pemphigus, pemphigoid, lupus erythematosus |
| Medication | Any medication that may cause dry mouth |
An extraoral assessment for any temporomandibular joint problems, facial asymmetry, lymph node enlargement, lower face height and soft tissue support are all routine clinical requirements. Following this, the patient should be asked to remove their dentures and an intraoral assessment should be carried out. All soft tissues should be inspected, including the floor of mouth and tonsillar fossa and the health of the tissues evaluated. The elderly edentulous patient is more likely to present with oral lesions, and a dentist may often be the first person to detect such problems. In this respect, it is important to appreciate the possible oral manifestations of systemic disorders as elderly patients often present with complex medical conditions.
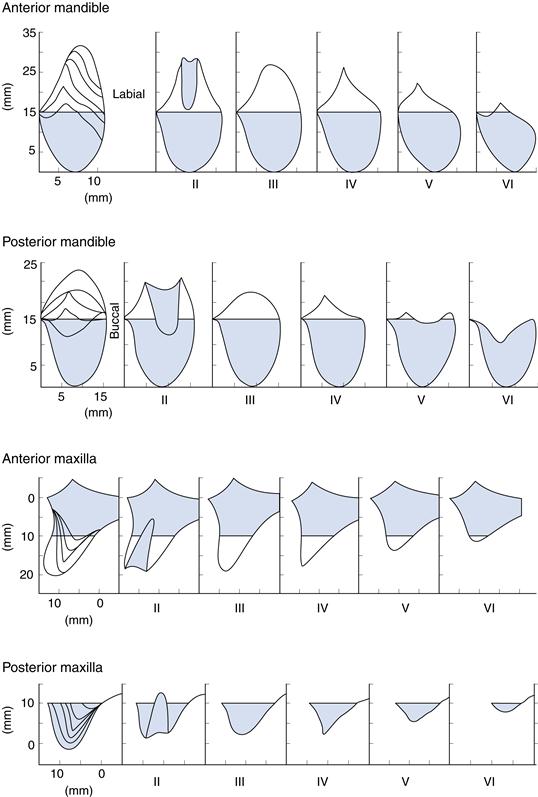
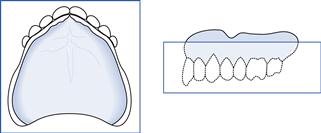
The ridges should then be palpated and a note made as to the remaining hard tissue support. A classification system of the type shown in Figure 4.1 is of great benefit.
Once the health of the extraoral and intraoral hard and soft tissues has been examined, a detailed examination of the dentures themselves should be carried out away from the mouth to assess their cleanliness and condition. Each denture in turn should then be placed intraorally to assess:
Retention
Definition: Resistance of a denture to vertical movement away from the tissues.
It is often beneficial to classify retention as being good, adequate or poor; reasons for lack of retention should be listed, such as under- or overextension of the periphery, position of post-dam, adaptation of the fitting surface
Stability
Definition: The resistance of a denture to displacement by functional forces.
A scale of good, adequate or poor should be used and the reasons for lack of stability listed such as flabby ridge, unsupported ridge, extensive resorption or inadequate muscle control
Occlusion
Definition: Any contact between teeth of opposing dental arches.
A classification should be used to describe the occlusal relationship of the dentures and a general assessment of occlusal contact and support should be made; a measure of the freeway space (interocclusal clearance) provided by the dentures is also important.
Once the history has been completed, it is important that a treatment plan should be developed for every patient, which will be dependent upon the presenting complaints together with the findings from the clinical examination. The proposed treatment should include any preliminary requirements, treatment of denture stomatitis or preprosthetic surgery, followed by the intended technique of denture construction including any special considerations. It is not satisfactory for the treatment plan to be simply the construction of complete dentures. It should also clearly indicate the impression materials, freeway space present, balanced occlusion, tooth selection and selection of acrylic matrix. Specific indication should be given of the indications for copy dentures, functional impression, neutral zone technique, lingualised occlusion or flat-cusped teeth.
Clinical techniques
Visit 1: Preliminary impressions
Preliminary impressions are taken in stock trays using impression compound or another suitable impression material of choice. Impression compound is widely used in teaching establishments as it often records a slightly overextended first impression which is preferable for tray construction. These special trays may need modification (reduction or border moulding) to improve their suitability for the patient. In some cases, the detail of such impressions may be improved using an alginate wash.
Laboratory prescription
As the next appointment will be for recording master impressions, it is essential at this and subsequent stages to indicate precisely your technical requirements. The prescription on the laboratory card should be clear and comprehensive. If there is any possibility of confusion, it is most valuable to discuss the patient personally with the technician involved. If a laboratory card is not completed and dated properly, the work may not be available at the next appointment.
Requirements for trays
Upper trays
Spaced (two thickness of modelling wax) light-cured trays should be prescribed for use with silicone or alginate impression material.
Lower trays
Close-fitting light-cured trays for use with zinc oxide/eugenol paste can be requested. If extensive undercuts are present, a spaced tray for alginate or silicone may be required. The spacing for the tray is dependent on the clinician’s choice of master impression material and therefore must be clearly requested on the laboratory card.
Borders
The peripheral border of all trays should finish 2 mm short of the depth of the sulcus when the spacer is in place. This is approximately the position of the mucogingival line and will enable the clinician to record the functional sulcus depth in the master impression.
Visit 2: Master impressions
(This stage may not be required if a high-quality primary impression is recorded. See evidence base.)
The master impression should record detail of the denture-bearing area together with the depth and width of the functional sulcus so that the finished denture maintains an effective facial seal. In some cases, the tray will require modification to its peripheral border and this should be carried out using autopolymerising acrylic resin or greenstick compound prior to the impression being recorded.
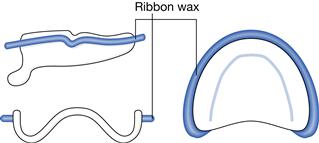
Normally, upper impressions using silicone or alginate and lower impressions will be recorded using alginate or zinc oxide/eugenol paste. These impressions are not to be considered complete until ribbon wax is placed approximately 2 mm from the periphery of the impression in order to provide a land area and protect the width of the sulcus on the resultant master cast. This placement of ribbon wax is called beading (Fig. 4.2). In the cases where alginate is used, a line must be drawn with indelible pencil on the facial surface of the impression 2 mm from the periphery for the same reason. This land area must not be removed!
Laboratory prescription
Casts should be poured in dental stone and a prescription provided regarding the construction of occlusal rims. The material to be used for the occlusal rim bases must be specified. This may be polystyrene (a vacuum-formed base) or shellac for the maxilla with wax and a wire strengthener being acceptable for the mandible. Acrylic resin may also be used and if permanent acrylic bases are requested these should be made in clear, heat-cured resin. In this event, you must prepare a post dam on the upper cast and indicate the position of a palatal relief if required. Wax bases are never suitable for upper rims.
It is always advisable after pouring the master casts to retain the individual trays until all treatment has been completed.
Visit 3: Recording jaw relations
It is important to remember that previous dentures may provide useful information on the appropriate jaw relationship, occlusal plane, incisal level and the relationship of teeth to soft tissues. Any alterations to these factors that may be required should have been noted at the treatment-planning stage.
Clinical procedure
Wax rims can either be provided on heat-cured bases, shellac or polystyrene vacuum-formed bases or with some form of strengthener present. If the occlusal rims are constructed on acrylic bases, the fitting surfaces should be examined for sharp edges, acrylic ‘pearls’ and excessive undercuts. These must be corrected before proceeding. If the acrylic resin has been extended into bony undercuts, disclosing wax or pressure relief cream may be used to locate any area requiring adjustment. The stability, retention and peripheral extension of upper and lower occlusal rims should be assessed and modified if necessary. If retention is persistently poor, it must be decided whether this is the result of an inaccurate cast. If this is the case, the master impressions should be repeated or a wash impression recorded if heat-cured baseplates are being used. Remember to chill occlusal rims frequently in cold water in order to minimise distortion.
The presence of dentures in the mouth will modify the rest position. Measurements of the resting face height should normally be made with the upper rim in place.
The upper record rim is adjusted so that:
• occlusal plane is correct (parallel to the lower ridge, alar-tragus and interpupillary lines)
• labial and buccal contour is correct (allowing for buccal corridors to be present)
The lower rim should be adjusted to correct the buccolingual contour posteriorly and correct the labial contour anteriorly. The rim should sit in the neutral zone. It should be trimmed to establish even, bilateral contact at the retruded contact position. In this respect, the patient should be asked to close until the rims first contact. Excessive pressure may cause them to tilt or be displaced into the alveolar mucosa, giving the appearance of even contact when, in fact, it does not exist. In some cases, the patient may be helped to find the retruded position by asking them to curl the tongue back to contact the posterior border of the upper occlusal rim.
An assessment should be made of the rest vertical dimension and vertical dimension of occlusion both from facial appearance and from measurement using the Willis gauge or using dividers measuring two soft tissue marks on the face. This should ensure that there is an adequate intraocclusal clearance. In an elderly patient who has been a denture wearer for many years, often providing slightly more freeway space is beneficial.
When satisfied that the patient is consistently occluding in the retruded jaw relation at the correct vertical dimension of occlusion, make locating marks in the midline and buccally in the canine region. Remove the rims and place them together outside the mouth using the locating marks. The jaw relation is now ready to be recorded but, prior to this, cut V-shaped notches in the upper rim and the round locating stops on the occlusal surface of the lower rim.
The rims are placed in the mouth and silicone jaw registration material or a similar recording material is applied to the lower rim. Stabilise the rims with fingers and encourage the patient to close into retruded jaw relation (check locating marks are coincident) and wait until the material has set. After removing rims from the mouth, check that casts can be placed into the rims without any premature contacts distally. Also ensure that the rims can be separated and relocated accurately.
Select teeth that are appropriate for the age, sex and racial characteristics of the patient. Reference may be made to previous dentures if the patient was happy with their appearance.
Cut the post dam on the master cast and outline any areas of the cast requiring relief (this will have been done at an earlier stage if heat-cured bases are used).
If the patient has consistently had problems with complete dentures or had a gross skeletal abnormality, it may be worth considering using a face-bow registration of the upper rim to allow for a more accurate location of the cast on the articulator in the laboratory.
Laboratory prescription
Record the shade, mould and material to be used for the artificial teeth on the laboratory card. Indicate the type of articulator (average movement or semiadjustable) on which the dentures are to be set up and indicate any aspects of the occlusal rims that are to be copied in the trial dentures. Indicate the type of bases required for the trial dentures. All casts should be mounted using a split-cast technique.
Visit 4: Trial dentures
An examination of the completed set up on the articulator should be carried out before trying in the mouth, and any discrepancies noted. The occlusion is then assessed, checking balance in excursive movements. If the trial dentures are not correct on the articulator, this must be rectified before proceeding.
In the mouth, carry out a complete assessment of the trial dentures including the following:
• Peripheral extension and shape of polished surfaces.
After carrying out any corrections that are necessary, obtain the patient’s comments. Do not proceed to finish unless the patient is satisfied, especially with the appearance (record this in the notes).
If the occlusion and vertical dimension of occlusion is incorrect, it means that the previous jaw registration was also incorrect. Accordingly, a new jaw registration will require to be recorded using the trial denture as an occlusal rim. In this case, it is usually necessary to remove all posterior teeth from the lower denture and replace them with a wax occlusal rim. This can then be modified using bite registration material until the correct occlusion is obtained, and the dentures sealed together at the new registration. Where the occlusion of trial dentures is subject to such modifications, the casts must be remounted on the articulator to the new registration as the jaw relationship has been changed. The dentures would then proceed to being reset and tried in again at the next visit.
Final laboratory prescription
The prescription should state definitely whether dentures can be finished or if a further trial is required. If the jaw relationship has been re-recorded, the casts are remounted on the articulator and a second trial stage is carried out. When the dentures are processed, use of the split-cast technique will avoid occlusal errors during processing. Instructions should be given for any special colouring of the acrylic matrix.
Porosity
One of the possible faults that can occur in the laboratory is porosity within the acrylic resin or tooth movement during the processing cycle.
Contraction porosity results when insufficient acrylic dough has been placed to create an excess or flash. Alternatively, the application of insufficient pressure during curing can lead to porosity voids dispersed throughout the whole mass of the denture base.
Gaseous porosity results when the temperature of the dough is raised significantly above the boiling point of the monomer (100°C), producing spherical voids in the hottest part of the curing dough. This occurs most commonly in the lingual flanges of a lower denture.
Granular porosity results from evaporation of the monomer during preparation. Proportioning of the powder to liquid ratio is dependent on allowing each powder particle to become wetted by monomer. The mixture is left to stand until it reaches the right consistency suitable for packing into the gypsum mould. During this standing period, a lid should be placed on the mixing vessel to prevent evaporation of the monomer. Loss of monomer during this stage can produce granular porosity in the set material, which is characterised by a blotchy opaque surface.
Visit 5: Final dentures
The processed dentures should be checked for any sharp edges, acrylic ‘pearls’ or excessive undercuts on the fitting surface. Insert each denture separately and check on fit and comfort to the patient. An examination of the occlusion in the mouth can be done either visually or using articulating paper.
Visual assessment is made by observing and by asking the patient if the teeth are meeting with equal pressure on both sides of the mouth when the mouth is closed gently.
Articulating paper is used to confirm these findings and to locate precisely any premature contacts. A heavy mark made by the paper may indicate where the initial contact is being made. Fossa rather than cusp tips should be ground at this stage only. Beware of artefacts, such as those produced by tilting of the dentures. This would produce marks from the articulating paper on both sides of the mouth, whereas initial observations may have indicated that the first occlusal contact is only on one side.
Remember, if any occlusal faults are diagnosed, it is a clinical and not a laboratory error providing that the split-cast technique has been used. Relatively minor occlusal discrepancies may be adjusted at the chair side until:
Chair-side occlusal adjustments are particularly difficult; where there is any doubt, a check record should be obtained.
Check record
A check record is advisable for the correction of occlusal errors that are too large to adjust easily at the chairside. This technique is also more reliable and accurate than major adjustment made at the chair side using articulating paper. Narrowed wax wafers, constructed from one thickness of pink modelling wax, are sealed to the occlusal surfaces of the lower posterior teeth and adjusted so that the patient occludes evenly on the wafers in retruded jaw relation with the teeth separated by a distance less than the freeway space. The teeth should not penetrate through the wax, otherwise tooth contact may cause displacement of the dentures and/or the mandible. This occlusal registration may be refined using registration paste. The dentures are then remounted on an average movement, or semiadjustable, articulator.
The articulator is closed with the incisal pin removed, and the occlusal contacts are checked visually and with articulating paper. Adjustments are carried out until an even occlusion is obtained. The dentures are reinserted and the occlusion checked in the mouth. This is often a major saving in time if an occlusal error is found at the initial insertion stage. A face bow is unnecessary for check record adjustments.
The time taken for remounting can be reduced significantly if the need for a check record is anticipated at the trial stage. The laboratory should be asked to return the processed dentures for the fit stage with the upper denture and cast located by the split-cast mounting. It is then only necessary for the occlusal record to be obtained and the lower denture to be remounted before the adjustments can be carried out.
Evidence base for this clinical approach to complete denture construction
As with lots of areas of clinical dentistry, there is little evidence to support clinical approaches, however the following does suggest that maybe master impressions may not be required to provide the same degree of patient satisfaction.
Simple complete denture techniques can provide patient satisfaction
When complete dentures are required, are simplified techniques as effective as complex traditional ones for their manufacture? A randomised controlled trial (RCT) was carried out in a hospital environment by Kawai et al (2005). A total of 122 edentulous individuals, aged 45–75 years, were randomly allocated into groups to receive dentures made using either traditional or simplified techniques. Individuals allocated to the traditional arm had a final impression taken in a custom-made tray and a face-bow recording and a semiadjustable articulator were used, with articulator remount after delivery. Those in the simplified technique group had impressions taken in stock trays and no face-bow recording and a monoplane articulator were used, with no articulator remount after delivery. There were no significant differences between the two groups in patient ratings for overall satisfaction at 3 or 6 months. These results suggest the use of simplified techniques, which are easier to master and which should reduce treatment costs. Educators should consider these findings when designing curricula for prosthodontic training.
Critical review of some dogmas in prosthodontics (Carlsson 2009)
Advice to patients
Preferably a printed leaflet giving instructions in respect of new dentures should be discussed with your patient after the final dentures have been inserted. In particular, the importance of good denture hygiene should be emphasised. If an immersion cleaner is recommended, a hypochlorite type is the most suitable. Any mechanical cleaning should be done with a brush that allows access and has good adaptability to all surfaces of the denture.
If the patient has to leave the new dentures out because of pain or soreness, request that the dentures be worn for 24 hours before the review appointment, in order that the cause of the discomfort may be more readily detected. Under no circumstances should the patient attempt adjustment of the dentures.
Denture maintenance
Unfortunately, evidence-based guidelines for the care and maintenance of removable complete denture prostheses do not exist. Based on the best available evidence, the following are guidelines for the care and maintenance of dentures (Felton et al 2011):
b. Denture cleansers should ONLY be used to clean dentures outside of the mouth.
4. Dentures should never be placed in boiling water.
7. Denture adhesives, when properly used, can improve the retention and stability of dentures and help seal out the accumulation of food particles beneath the dentures, even in well-fitting dentures.
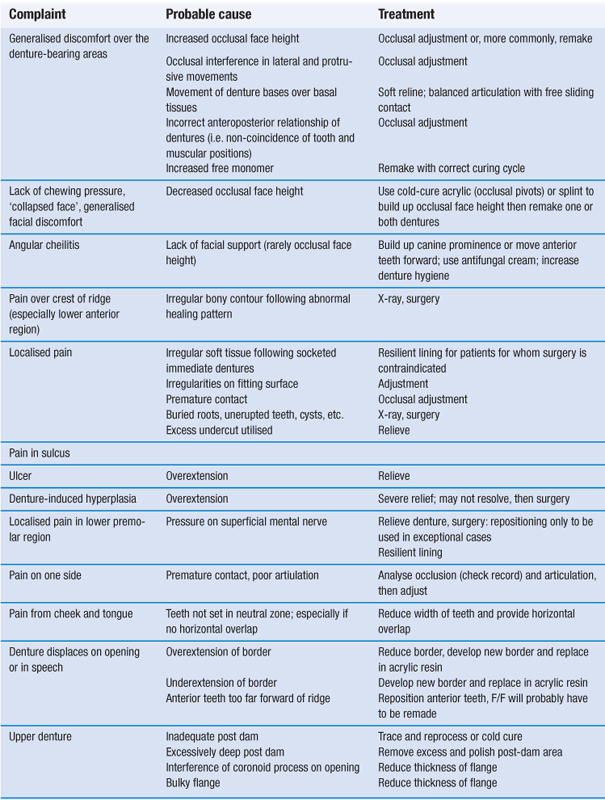
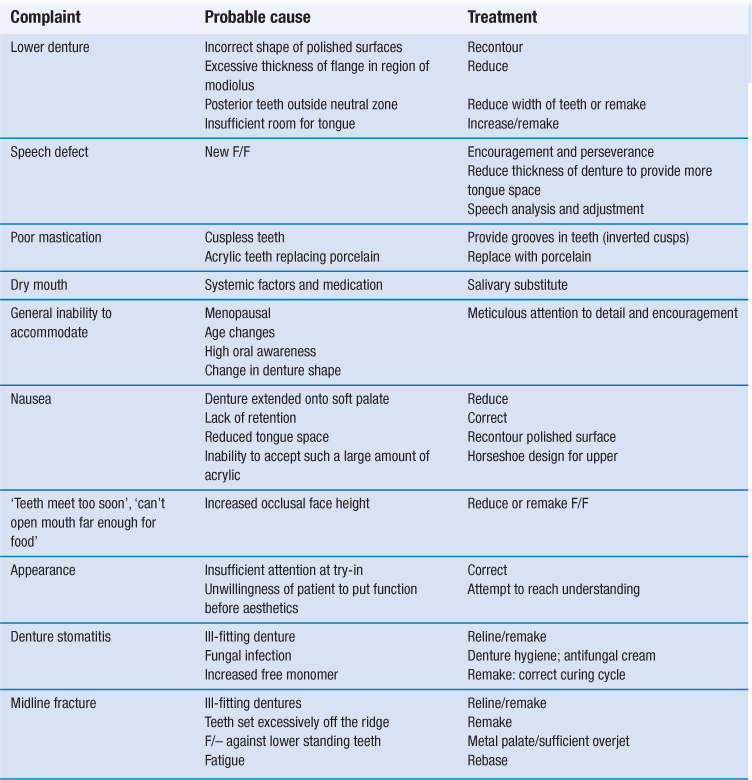
Common complaints of the edentulous patient
Most prosthetic complaints can be prevented or minimised by adequate diagnosis, treatment planning and treatment plus attention to detail during the construction phase. A preprosthetic radiographic investigation can prevent the finding of retained roots, unerupted teeth and bone pathology after the new dentures have been constructed; however, this should not be done as a matter of course. Pretreatment case history and clinical investigation with a detailed assessment of any existing dentures should aid the solution of such problems as correct face height, tooth position and polished contour. However, problems and complaints will still occur with new dentures. Table 4.2 lists some of the more common complaints, their probable causes and suggested treatment.
Relines or rebases
A reline involves the addition of a material to the fitting surface of a denture base. A rebase involves the removal and replacement of virtually all the denture base, namely the fitting and polished surface of the denture.
Advantages of a reline
Advantages of a rebase
• Will not increase the thickness of the palate.
• Will remove the majority of the previous denture base if, for example, bleaching has occurred.
There are few indications these days for a full rebase as it is often more satisfactory to consider a copy technique of the denture that would have been rebased; this will not necessitate the removal of the denture from the patient.
4.2 Copy/duplicate dentures
Tradition in dentistry dies hard as it does in other fields, and many dentists still persist in starting from the assumption that a patient presents no valuable information from the existing prosthesis and a conventional technique of denture construction can always produce a better result. This, of course, is not always the case, as patients who have worn dentures satisfactorily over a long period of time have developed a neuromuscular feedback in relationship to the spatial relationship of the denture to the surrounding tissues. It is for such patients that the concept of the copy denture can yield satisfactory results.
In this respect, however, it is important to realise that the copy denture does not simply replicate the current dentures worn by the patient. It is designed specifically to reproduce the favourable aspects of the current prosthesis such as tooth position and polished surfaces, while improving the adaptation and occlusion. Copy dentures are particularly useful for elderly patients with good denture-wearing experience.
Indications
There are a number of situations where copy dentures are advisable:
• Loss of retention in otherwise favourable dentures requiring replacement.
• Wear of the occlusal surfaces.
Typical dental history that would suggest an indication for copy dentures:
• Elderly patients presenting with satisfactory complete dentures.
• Worn occlusal surfaces, indicating long-term acceptability.
• Deterioration of denture base materials.
Clinical advantages
Technical advantages
Alginate copy box/silicone copy technique
First clinical stage
Any modifications are made at the first clinical stage (Box 4.1).
Laboratory stage
Wax-acrylic replicas are poured by adding wax into the mould to 1 mm past the gingival margins of the teeth and allowed to set. The base of the wax is then scored and self-cured acrylic is poured into the closed mould through previously cut sprue holes and allowed to polymerise. A stone duplicate is cast into the mould once the wax and acrylic copy has been removed. This stone mould can be used for comparison of the copy try-in. The denture templates are then removed from the moulds and articulated using the/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses