4 PRINCIPLES OF OCCLUSION
ANATOMY
Temporomandibular Joints
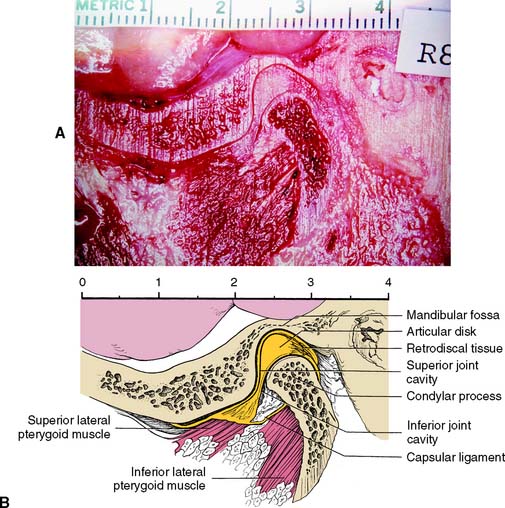
The major components of the temporomandibular joints (TMJs) are the cranial base, the mandible, and the muscles of mastication with their innervation and vascular supply. Each joint can be described as ginglymoarthrodial, which means that it is capable of both a hinging and a gliding articulation. An articular disk separates the mandibular fossa and articular tubercle of the temporal bone from the condylar process of the mandible.
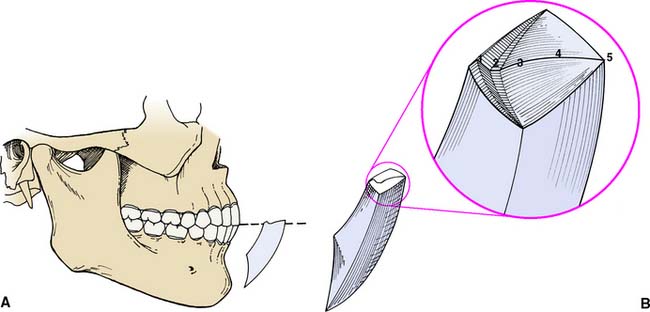
The articulating surfaces of the condylar processes and fossae are covered with avascular fibrous tissue (in contrast to most other joints, which have hyaline cartilage). The articular disk consists of dense connective tissue; it also is avascular and devoid of nerves in the area where articulation normally occurs. Posteriorly, it is attached to loose highly vascularized and innervated connective tissue, the retrodiscal pad or bilaminar zone,* which connects to the posterior wall of the articular capsule surrounding the joint (Fig. 4-1). Medially and laterally, the disk is attached firmly to the poles of the condylar process. Anteriorly, it fuses with the capsule and with the superior lateral pterygoid muscle. Superior and inferior to the articular disk are two spaces: the superior and inferior synovial cavities. These are bordered peripherally by the capsule and the synovial membranes and are filled with synovial fluid. Because of its firm attachment to the poles of each condylar process, the disk follows condylar movement during both hinging and translation, which is made possible by the loose attachment of the posterior connective tissues.
Ligaments
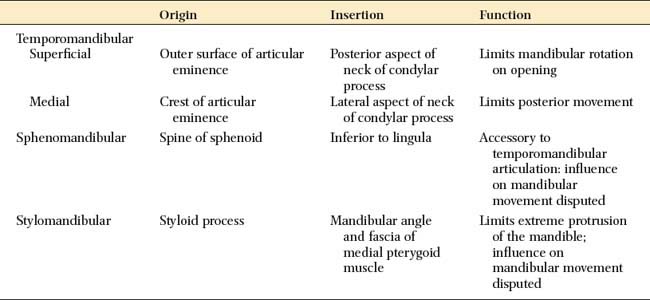
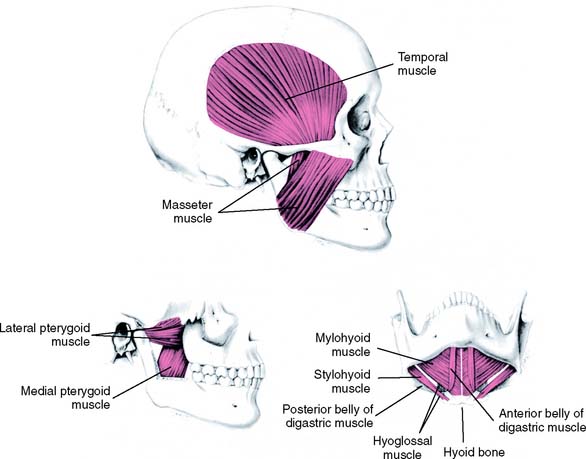
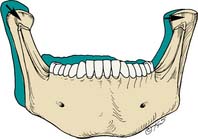
The body of the mandible is attached to the base of the skull by muscles and also by three paired ligaments (Table 4-1): the temporomandibular (also called the lateral), the sphenomandibular, and the stylomandibular. Ligaments cannot be stretched significantly, and so they limit the movement of joints. The temporomandibular ligaments limit the amount of rotation of the mandible and protect the structures of the joint, limiting border movements.1 The sphenomandibular and stylomandibular ligaments (Fig. 4-2) limit separation between the condylar process and the disk; the stylomandibular ligaments also limit protrusive movement of the mandible.
Musculature
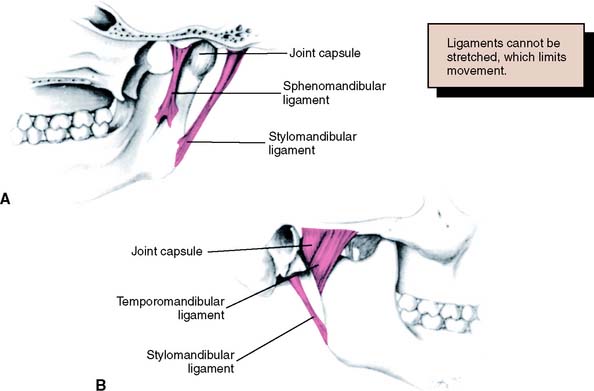
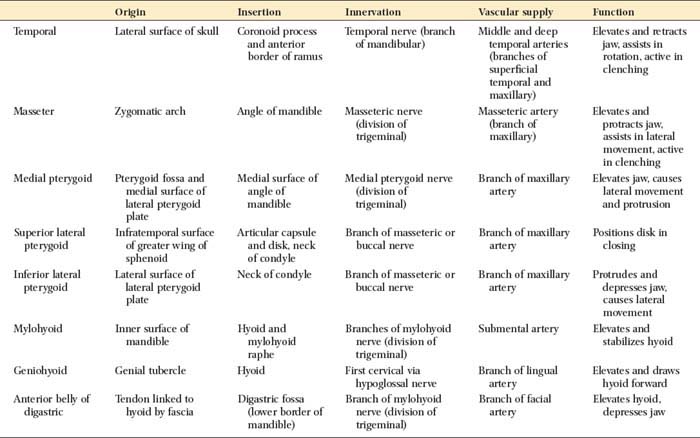
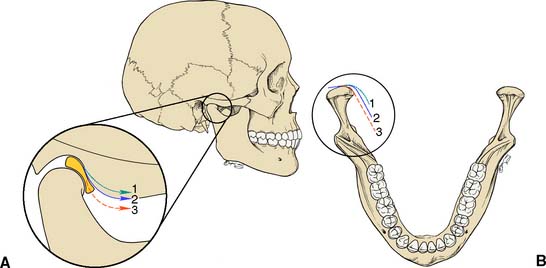
Several muscles are responsible for mandibular movements. These can be grouped into the muscles of mastication and the suprahyoid muscles (Fig. 4-3). The former include the temporal, the masseter, and the medial and lateral pterygoid muscles; the latter are the geniohyoid, the mylohyoid, and the digastric muscles. Their respective origins, insertions, and innervation and vascular supply are summarized in Table 4-2.
Muscular function
The functions of the mandibular muscles are well-coordinated, complex events.
The three paired muscles of mastication provide elevation and lateral movement of the mandible. These are the temporal, the masseter, and the medial pterygoid muscles. The lateral pterygoid muscles, each with two bellies (which probably should be considered as two separate muscles), function horizontally during opening and closing; the inferior belly (or inferior lateral pterygoid) is active during protrusion, depression, and lateral movement; the superior belly (or superior lateral pterygoid) is active during closure. The latter muscle is thought to assist in maintaining the integrity of the condyle-disk assembly by pulling the condylar process firmly against the disk, because the superior belly has been shown to attach to the disk and the neck of the condyle.
Dentition
The relative positions of the maxillary and mandibular teeth influence mandibular movement. Many “ideal” occlusions have been described.2 In most of these, the maxillary and mandibular teeth contact simultaneously when the condylar processes are fully seated in the mandibular fossae and the teeth do not interfere with harmonious movement of the mandible during function. Ideally, in the fully bilateral seated position of the condyle-disk assemblies, the maxillary and mandibular teeth exhibit maximum intercuspation. This means that the maxillary lingual and mandibular buccal cusps of the posterior teeth are evenly distributed and in stable contact with the opposing occlusal fossae. These functional cusps can then act as stops for vertical closure without excessively loading any one tooth, while left and right TMJs are simultaneously in an unstrained position.
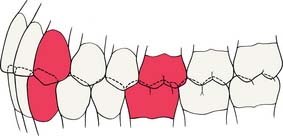
However, in many patients, maximal intercuspal contact occurs with the condyles in a slightly translated position. This position is referred to as maximum intercuspation which is defined as the complete intercuspation of the opposing teeth independent of condylar position, sometimes referred to as the best fit of the teeth regardless of the condylar position. If the mesiobuccal cusp of the maxillary first molar is aligned with the buccal groove of the mandibular first molar, an Angle Class I orthodontic relationship (Fig. 4-4) exists; this is considered normal (see glossary). In such a relationship, the anterior teeth overlap both horizontally and vertically. This position is defined as the dental relationship in which there is normal anteroposterior relationship of the jaws, as indicated by correct intercuspation of maxillary and mandibular molars, but, when a malocclusion is present, there are crowding and rotation of teeth elsewhere (i.e., a dental dysplasia or arch length deficiency). Orthodontic textbooks3 have traditionally described an arbitrary 2 mm for horizontal overlap and vertical overlap as being ideal. For most patients, however, greater vertical overlap of the anterior teeth is desirable, to prevent undesirable posterior tooth contact as a result of flexing of the mandible during mastication. Empirically, dentitions with greater vertical overlap of the anterior teeth appear to have a better long-term prognosis than do dentitions with minimal vertical overlap.
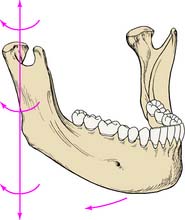
MANDIBULAR MOVEMENT
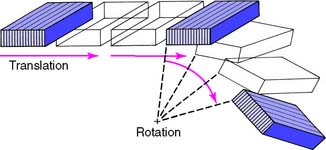
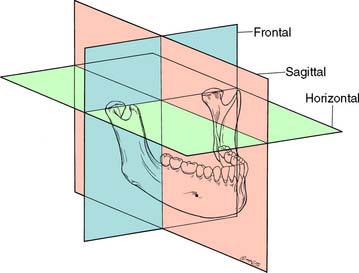
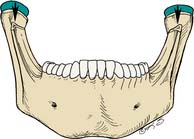
As for any other movement in space, complex three-dimensional mandibular movement can be broken down into two basic components: translation, when all points within a body have identical motion, and rotation, when the body is turning about an axis (Fig. 4-5). Every possible three-dimensional movement can be described in terms of these two components. It is easier to understand mandibular movement when the components are described as projections in three perpendicular planes: sagittal, horizontal, and frontal (Fig. 4-6).
Reference Planes
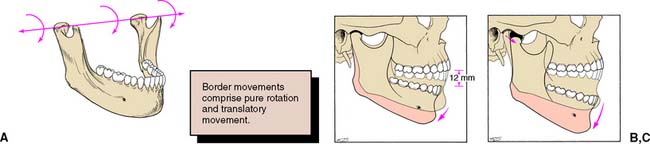
Sagittal plane
In the sagittal plane (Fig. 4-7), the mandible is capable of a purely rotational movement as well as translation. Rotation occurs around the terminal hinge axis, an imaginary horizontal line through the rotational centers of the left and right condylar processes. The rotational movement is limited to about 12 mm of incisor separation before the temporomandibular ligaments and structures anterior to the mastoid process force the mandible to translate. The initial rotation or hingeing motion is between the condyle and the articular disk. During translation, the lateral pterygoid muscle contracts and moves the condyle-disk assembly forward along the posterior incline of the tubercle. Condylar movement is similar during protrusive mandibular movement.
Horizontal plane
In the horizontal plane, the mandible is capable of rotation around several vertical axes. For example, lateral movement consists of rotation around an axis situated in the working (laterotrusive) condylar process (Fig. 4-8) with relatively little concurrent translation. A slight lateral translation of the condyle on the working side in the horizontal plane—known as laterotrusion, Bennett movement,4 or mandibular side shift (Fig. 4-9)—is frequently present. This may be slightly forward or slightly backward (lateroprotrusion or lateroretrusion). The orbiting (nonworking) condyle travels forward and medially as limited by the medial aspect of the mandibular fossa and the temporomandibular ligament. Finally, the mandible can make a straight protrusive (anterior) movement (Fig. 4-10).
Frontal plane
In a lateral movement in the frontal plane, the mediotrusive (or nonworking) condyle moves down and medially, whereas the laterotrusive (or working) condyle rotates around the sagittal axis perpendicular to this plane (Fig. 4-11). Again, as determined by the anatomy of the medial wall of the mandibular fossa on the mediotrusive side, transtrusion may be observed; as determined by the anatomy of the mandibular fossa on the laterotrusive side, this may be lateral and upward or lateral and downward (laterosurtrusion and laterodetrusion). A straight protrusive movement observed in the frontal plane, with both condylar processes moving downward as they slide along the tubercular eminences, is shown in Figure 4-12.
Border Movements
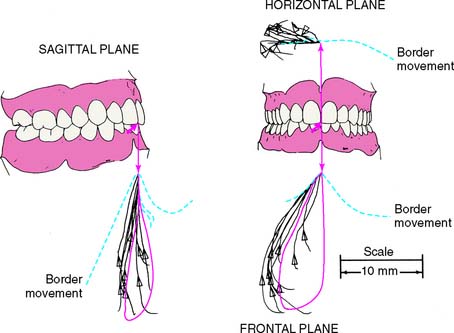
Mandibular movements are limited by the TMJs and ligaments, the neuromuscular system, and the teeth. Posselt5 was the first to describe mandibular movement at the limits dictated by anatomic structures, as viewed in a given plane which he called border movements (Fig. 4-13). His classic work is well worth reviewing in the attempt to understand how the determinants control the extent to which movement can occur.
Posselt used a three-dimensional representation of the extreme movements that the mandible is capable of (see Fig. 4-13B). All possible mandibular movements occur within its boundaries. At the top of both illustrations, a horizontal tracing represents the protrusive movement of the incisal edge of the mandibular incisors (solid numbered line in Fig. 4-13B).
Starting from the maximum intercuspation position, in the protrusive pathway, the lower incisors are initially guided by the lingual concavity of the maxillary anterior teeth. This leads to gradual loss of posterior tooth contact as the incisors reach the edge-to-edge position. This is represented in Posselt’s diagram by the initial downward slope. As the mandible moves farther protrusively, the incisors slide over a horizontal trajectory representing the edge-to-edge position (the flat portion in the diagram), after which the lower incisors move upward until new posterior tooth contact occurs. Further protrusive movement of the mandible typically takes place without significant tooth contact.
The border farthest to the right of Posselt’s solid (see Fig. 4-13B) represents the most protruded opening and closing stroke. The maximal open position of the mandible is represented by the lowest point in the diagram. The left border of the diagram represents the most retruded closing stroke. This movement occurs in two phases: The lower portion consists of a combined rotation and translation, until the condylar processes return to the fossae. The second portion of the most retruded closing stroke is represented by the top portion of the border that is farthest to the left in Posselt’s diagram. It is strictly rotational.
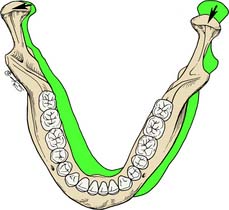
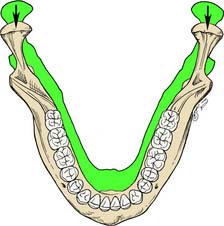
Posterior and anterior determinants of mandibular movement
These determinants (Table 4-3) are the anatomic structures that dictate or limit the movements of the mandible. The anterior determinant of mandibular movement is the dental articulation. The posterior determinants of mandibular movement are the temporomandibular articulations and their associated structures The posterior determinants (Fig. 4-14)—shape of the articular eminences, anatomy of the medial walls of the mandibular fossae, configuration of the mandibular condylar processes—cannot be controlled, and it is not possible to influence the neuromuscular responses of the patient unless it is done by indirect means (e.g., through changes in the configuration of the contacting teeth or by the provision of an occlusal appliance). If a patient has steeply sloped eminences, there is a large downward component of condylar movement during lateral and protrusive excursions. Similarly, the anatomy of the medial wall of each fossa normally allows the condyle to move slightly medially as it travels forward (mandibular side shift, or transtrusion). The side shift becomes greater as the extent of medial movement increases. However, the anatomy of the joint dictates the actual path and timing of condylar movement. Movement of the laterotrusive or working condylar process is influenced predominantly by the anatomy of the lateral wall of the mandibular fossa. The amount of the side shift is, of course, a function of the mediotrusive or nonworking condyle; on the working side, however, it is the anatomy of the lateral aspect of the fossa that guides the working condyle straight out or upward and downward. The amount of side shift does not appear to increase as the result of a loss of occlusion.6
Table 4-3 IMPACT OF SELECTED VARIABLES ON OCCLUSAL FORM OF RESTORATIONS
| Variation | Impact on Restoration | |
|---|---|---|
| POSTERIOR DETERMINANTS | ||
| Inclination of articular eminence | Steeper | Posterior cusps may be taller |
| Flatter | Posterior cusps must be shorter | |
| Medial wall of glenoid fossa | Allows more lateral translation | Posterior cusps must be shorter |
| Allows minimal lateral translation | Posterior cusps may be taller | |
| Intercondylar distance | Greater | Smaller angle between laterotrusive and mediotrusive movement |
| Lesser | Increased angle between laterotrusive and mediotrusive movement | |
| ANTERIOR DETERMINANTS | ||
| Horizontal overlap of anterior teeth | Increased | Posterior cusps must be shorter |
| Reduced | Posterior cusps may be taller | |
| Vertical overlap of anterior teeth | Increased | Posterior cusps may be taller |
| Reduced | Posterior cusps must be shorter | |
| OTHER | ||
| Occlusal plane | More parallel to condylar guidance | Posterior cusps must be shorter |
| Less parallel to condylar guidance | Posterior cusps may be longer | |
| Anteroposterior curve | More convex (shorter radius) | The most posterior cusps must be shorter |
| Less convex (larger radius) | The most posterior cusps may be longer |
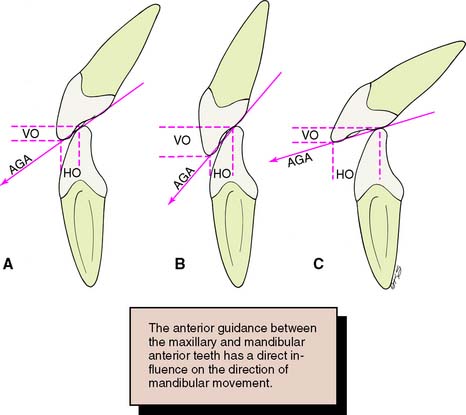
The anterior determinants (Fig. 4-15) are the vertical and horizontal overlaps and the maxillary lingual concavities of the anterior teeth. These can be altered by restorative and orthodontic treatment. A greater vertical overlap causes the direction of mandibular opening to be more vertical during the early phase of protrusive movement and creates a more vertical pathway at the end of the chewing stroke. Increased horizontal overlap allows a more horizontal jaw movement.
Although the posterior and anterior determinants combine to affect mandibular movement, no correlation has been established7; that is, patients with steep anterior guidance angles do not necessarily have a steep posterior disclusion, and those with a steep posterior disclusion do not necessarily have steep guidance angles.
Functional Movements
Chewing
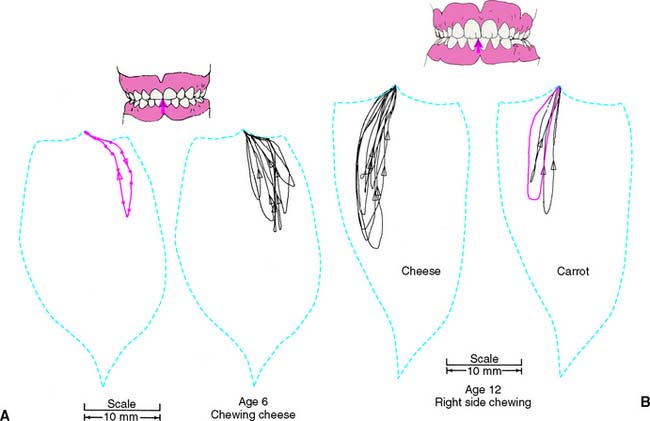
When incising food, adults open their mouths a comfortable distance and move the mandible forward until they incise, with the anterior teeth meeting approximately edge to edge. The food bolus is then transported to the center of the mouth as the mandible returns to its starting position, with the incisal edges of the mandibular anterior teeth tracking along the lingual concavities of the maxillary anterior teeth (Fig. 4-16). The mouth then opens slightly, the tongue pushes the food onto the occlusal table, and, after moving sideways, the mandible closes into the food until the guiding teeth (typically the canines) contact.8 The cycle is completed as the mandible returns to its starting position.9 This pattern repeats itself until the food bolus has been reduced to particles that are small enough to be swallowed, at which point the process can start over. The direction of the mandibular path of closure is influenced by the inclination of the occlusal plane with the teeth apart and by the occlusal guidance as the jaw approaches maximum intercuspation.10
The chewing pattern observed in children differs from that found in adults. Until about age 10, children begin the chewing stroke with a lateral movement. After the age of 10, they start to chew increasingly like adults, with a more vertical stroke11 (Fig. 4-17). Stimuli from the pressoreceptors play an important role in the development of functional chewing cycles.12
Speaking
The teeth, tongue, lips, floor of the mouth, and soft palate form the resonance chamber that affects pronunciation. During speech, the teeth are generally not in contact, although the anterior teeth may come very close together during soft “c,” “ch,” “s,” and “z” sounds, forming the “speaking space: the space that occurs between the incisal and/or occlusal surfaces of the maxillary and mandibular teeth during speech.”13 When pronouncing the fricative “f,” the inner vermilion border of the lower lip traps air against the incisal edges of the maxillary incisors. Phonetics is a useful diagnostic guide for correcting vertical dimension and tooth position during fixed and removable prosthodontic treatment.14–17
Parafunctional Movements
Parafunctional movements of the mandible may be described as sustained activities that occur beyond the normal functions of mastication, swallowing, and speech. There are many forms of parafunctional activities, including bruxism, clenching, nail biting, and pencil chewing, among others. Typically, parafunction is manifested by long periods of increased muscle contraction and hyperactivity. Concurrently, excessive occlusal pressure and prolonged tooth contact occur, which is inconsistent with the normal chewing cycle. Over a protracted period, this can result in excessive wear; widening of the periodontal ligament; and mobility, migration, or fracture of the teeth. Muscle dysfunction such as myospasms, myositis, myalgia, and referred pain (headaches) from trigger point tenderness may also occur. The degree of symptoms varies considerably among individuals. The two most common forms of parafunctional activities are bruxism and clenching. Increased radiographic bone density is often seen in patients with a history of sustained parafunctional activity.
Bruxism
Oral habits consisting of involuntary rhythmic or spasmodic nonfunctional gnashing, grinding, or clenching of teeth, in other than chewing movements of the mandible, that may lead to occlusal trauma is known as bruxism (Fig. 4-18). This activity may be diurnal, nocturnal, or both. Although bruxism is initiated on a subconscious level, nocturnal bruxism is potentially more harmful because the patient is not aware of it while sleeping. Therefore, it can be difficult to detect, but it should be suspected in any patient exhibiting abnormal tooth wear or pain. The prevalence of bruxism is about 10% and is less common with age.18 The etiology of bruxism is often unclear. Some theories relate bruxism to malocclusion, neuromuscular disturbances, responses to emotional distress, or a combination of these factors.19 A study on cohort twins has demonstrated substantial genetic effects20; the condition has been related to sleep disturbance21; and the symptoms of bruxism are three times more common in smokers.22 Altered mastication has been observed in subjects who brux23,24 and may result from an attempt to avoid premature occlusal contacts (occlusal interferences). There may also be a neuromuscular attempt to “rub out” an interfering cusp. The fulcrum effect of rubbing on posterior interferences creates a protrusive or laterotrusive movement that can cause overloading of the anterior teeth, with resultant excessive anterior wear. It is common for wear on anterior teeth to progress from initial faceting on the canines to the central and lateral incisors. Once vertical overlap diminishes as the result of wear, posterior wear facets are commonly observed. However, the chewing patterns of normal subjects can be quite varied, and the relationship, if any, between altered mastication and occlusal dysfunction is not clear.25
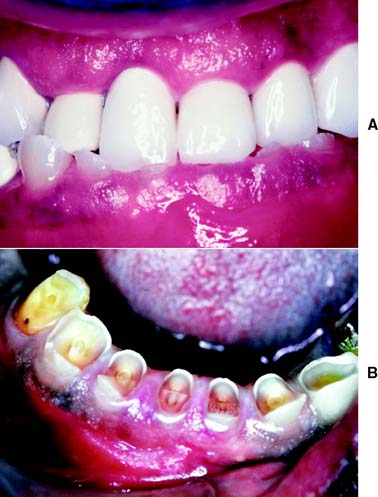
Fig. 4-18 Extensive abrasion (tooth wear) resulting from parafunctional grinding.
(Courtesy of Dr. M. Padilla.)
The causes of bruxism are difficult to determine. One theory26 states that bruxism is performed on a subconscious reflex-controlled level and is related to emotional responses and occlusal interferences. In certain malocclusions, the neuromuscular system exerts fine control during chewing to avoid particular occlusal interferences. As the degree of muscle activity necessary to avoid the interferences becomes greater, an increase in muscle tone may result, with subsequent pain in the hyperactive musculature, which in turn can lead to restricted movement. The relationship, if any, between bruxism and temporomandibular disorders is still unclear.27
Clenching
Clenching is defined as the pressing and clamping of the jaws and teeth together frequently associated with acute nervous tension or physical effort. The pressure thus created can be maintained over a considerable time with short periods of relaxation in between. The etiology can be associated with stress, anger, physical exertion, or intense concentration on a given task, rather than an occlusal disorder. In contrast to bruxism, clenching does not necessarily result in damage to the teeth because the concentration of pressure is directed more or less through the long axes of the posterior teeth without the involvement of detrimental lateral forces. Abfractions—cervical defects at the cementoenamel junction—may result from sustained clenching.28,29 Also, the increased load may result in damage to the periodontium, TMJs, and muscles of mastication. Typically, the elevator muscles become overdeveloped. Muscle splinting, myospasm, and myositis may progress, causing the patient to seek treatment. As with bruxism, clenching can be difficult to diagnose and difficult if not impossible for the patient to voluntarily control.
HISTORY OF OCCLUSAL STUDIES
Historically, the study of occlusion and articulation has undergone an evolution of concepts. These can be broadly categorized as concepts of bilaterally balanced,30 unilaterally balanced, and mutually protected articulation. Current emphasis in teaching fixed prosthodontics and restorative dentistry has been on the concept of mutual protection (Fig. 4-19). However, because restorative treatment requirements vary, the clinician should understand possible combinations of occlusal schemes and their advantages, disadvantages, and indications.
Bilaterally Balanced Articulation
Early work in removable prosthodontics centered on the concept of a bilaterally balanced articulation. This requires having a maximum number of teeth in contact in maximum intercuspation and all excursive positions. In complete denture fabrication, this tooth arrangement helps maintain denture stability because the nonworking contact prevents the denture from being dislodged. However, as the principles of bilateral balance were applied to the natural dentition and in fixed prosthodontics, it proved to be extremely difficult to accomplish, even with great attention to detail and with the use of sophisticated articulators. In addition, high rates of failure resulted. An increased rate of occlusal wear, increased or accelerated periodontal breakdown, and neuromuscular disturbances were commonly observed. The last were often relieved when posterior contacts on the mediotrusive side were eliminated in an attempt to eliminate unfavorable loading. Thus, the concept of a unilaterally balanced occlusion (group function) evolved31 (Fig. 4-20).
Unilaterally Balanced Articulation (Group Function)
Long centric
As the concept of unilateral balance evolved, it was suggested that allowing some freedom of movement in an anteroposterior direction is advantageous. This concept is known as long centric. Schuyler32 was one of the first to advocate such an occlusal arrangement. He thought that it was important for the posterior teeth to be in harmonious gliding contact when the mandible translates from centric relation forward to make anterior tooth contact. Others33 have advocated long centric because centric relation only rarely coincides with the maximum intercuspation position in healthy natural dentitions. However, its length is arbitrary. At given vertical dimensions, long centric ranges from 0.5 to 1.5 mm in length have been advocated. This theory presupposes that the condyles can translate horizontally in the fossae over a commensurate trajectory before beginning to move downward. It also necessitates a greater horizontal space between the maxillary and mandibular anterior teeth (deeper lingual concavity), allowing horizontal movement before posterior disocclusion (separation of opposing teeth during eccentric movements of the mandible).
Mutually Protected Articulation
During the early 1960s, an occlusal scheme called mutually protected articulation was advocated by Stuart and Stallard,34 based on earlier work by D’Amico.35 In this arrangement, centric relation coincides with the maximum intercuspation position. The six anterior maxillary teeth, together with the six anterior mandibular teeth, guide excursive movements of the mandible, and no posterior occlusal contacts occur during any lateral or protrusive excursions.
The relationship of the anterior teeth, or anterior guidance, is critical to the success of this occlusal scheme. In a mutually protected articulation, the posterior teeth come into contact only at the very end of each chewing stroke, minimizing horizontal loading on the teeth. Concurrently, the posterior teeth act as stops for vertical closure when the mandible returns to its maximum intercuspation position. Posterior cusps should be sharp and should pass each other closely without contacting to maximize occlusal function. Investigations of the neuromuscular physiology of the masticatory apparatus indicate advantages associated with a mutually protected occlusal scheme.8 However, in studies involving unrestored dentitions, relatively few occlusions can be classified as mutually protected.36
Optimum occlusion
In an ideal occlusal arrangement, the load exerted on the dentition should be distributed optimally. Occlusal contact has been shown37 to influence muscle activity during mastication. Any restorative procedures that adversely affect occlusal stability may affect the timing and intensity of elevator muscle activity. Horizontal forces on any teeth should be avoided or at least minimized, and loading should be predominantly parallel to the long axes of the teeth. This is facilitated when the tips of the functional cusps are located centrally over the roots and when loading of the teeth occurs in the fossae of the occlusal surfaces rather than on the marginal ridges. Horizontal forces are also minimized if posterior tooth contact during excursive movements is avoided. Nevertheless, to enhance masticatory efficiency, the cusps of the posterior teeth should have adequate height. Stabilizing contacts involves primarily the mandibular buccal cusps, and it has been suggested that maintenance or improvement of the number of such contacts should be among occlusal treatment objectives.38
The chewing and grinding action of the teeth is enhanced if opposing cusps on the laterotrusive side interdigitate at the end of the chewing stroke. The mutually protected occlusal scheme probably meets this criterion better than the other occlusal arrangements. The features of a mutually protected articulation are as follows39:
Rationale
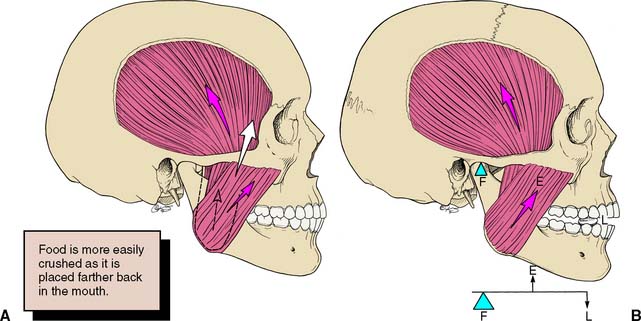
At first glance, it might seem illogical to load the single-rooted anterior teeth as opposed to the multirooted posterior teeth during chewing. However, the canines and incisors have a distinct mechanical advantage over the posterior teeth40: The effectiveness of the force exerted by the muscles of mastication is notably less when the loading contact occurs farther anteriorly.
The mandible is a lever of the class III type (Fig. 4-21), which is the least efficient of lever systems. An example of another class III lever would be a fishing pole. The longer the pole, the more effort it takes to pull a fish out of the water. The same holds true for the muscles of mastication and the teeth: the farther anteriorly initial tooth-to-tooth contact occurs (i.e., the longer the lever arm), the less effective the forces exerted by the musculature are and the smaller the load to which the teeth are subjected is. The canine—with its long root, significant amount of periodontal surface area, and strategic position in the dental arch—is well adapted to guiding excursive movements. This function is governed by pressoreceptors in the periodontal ligament, receptors that are very sensitive to mechanical stimulation.41
PATIENT ADAPTABILITY
There are significant differences in the adaptive response of patients to occlusal abnormalities. Some individuals are unable to tolerate seemingly trivial occlusal deficiencies, whereas others are able to tolerate distinct malocclusions without obvious symptoms (Fig. 4-22). Most patients seem able to adapt to small occlusal deficiencies without exhibiting acute symptoms.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses