CHAPTER 4
Orthodontic Records and Case Evaluation
In a problem-oriented approach to diagnosing and treatment planning of patients with malocclusions, it is necessary to gather relevant information in a consistent manner in order to start a comprehensive database of information for each patient.
First, the orthodontist must establish a case history of each patient, noting the chief concerns, including medical and dental history. Second, a thorough clinical examination of the patient should be conducted to obtain accurate measurements and objective findings, which are the basis of the orthodontic diagnosis. This clinical examination should include a facial evaluation, both in the frontal and profile views, as well as an examination of the patient’s extraoral and intraoral soft tissue. The clinical examination should also contain an assessment of the dentition and a functional analysis of the temporomandibular joint (TMJ). Finally, complete orthodontic records should be taken, which consist of digital or plaster of Paris study models, panoramic and cephalometric radiographs, bitewing and periapical radiographs of the anterior teeth in adults, and extraoral and intraoral photographs. Any additional records that the orthodontist deems necessary should be included. In general, these orthodontic records document the patient’s initial condition and supplement the diagnostic information obtained through the patient interview and examination. The orthodontist can now analyze the collected data for problems in the areas of clinical examination, study casts analysis, radiographic analysis, and photographic analysis (< ?xml:namespace prefix = "mbp" />
After completion of the analysis, a list of problems in each of these areas can be developed and prioritized. In addition, a 3D-3T diagnostic grid is recommended as an aid in ensuring that all three dimensions (3D) of a malocclusion as well as all three tissues (3T) are evaluated. The three dimensions include sagittal, transverse, and vertical plane; the three tissues include skeletal, soft tissue, and dental structures. It is critical to understand that incorrect diagnosis is usually related to lack of information. A comprehensive diagnosis will provide a summary of the most important problems from each of the four areas listed above.
CLINICAL EXAMINATION
1 Which key points should be clarified in the patient’s medical and dental history?
It is important to note the patient’s chief concern and specify whether treatment is sought for functional reasons, esthetic improvement, or both.
2 Which aspects should be covered in the clinical examination?
In general, the face, oral cavity, and surrounding areas (including dentition) and TMJs should be examined. This specifically includes assessment of asymmetries, lip position in closure and repose, classification of the perioral musculature, and measurement of the incisor display at rest (see following cephalometric and photographic analysis questions). The health of all oral tissues and the patient’s periodontal status, especially in adults, should be evaluated. Periapical and bitewing radiographs are essential in evaluating all adult patients.
3 Which aspects of jaw and occlusal function should be evaluated?
There are five main areas of interest to the orthodontist: mastication, speech, breathing mode, orofacial dysfunctions, and TMJ function. Mastication, including swallowing patterns as well as the presence of speech problems such as articulation distortion, stuttering, or dyslexia, requires evaluation. Depending on the severity, this may necessitate referral to a specialist. The patient should also be asked about the prevalent respiration mode, mouth versus nasal breathing, and possible sleep disorders or problems with restricted airways, such as snoring. These may be associated with such conditions as tonsillar or adenoid enlargement, nasal obstruction, allergies, and retruded mandible. However, the etiologic significance of respiration mode in relationship to facial growth and development of malocclusions remains controversial throughout the literature.
4 How is the TMJ function examined?
The patient should be initially questioned about existing TMJ problems and the history of symptoms verified through manipulation and auscultation of the TMJ for sounds such as clicking, popping, or crepitus. Palpation of the TMJ and masticatory muscles is necessary to detect tenderness or pain. In addition, the patient’s range of motion (ROM) should be recorded by observing and measuring maximal mouth opening, right and left lateral excursions, and protrusive movement.
5 Which areas should be explored in the patient’s social and behavioral evaluation?
The patient’s motivation to seek orthodontic treatment should be assessed, since attitude and expectations concerning treatment are closely related to motivation. In general, internally as opposed to externally motivated patients show better cooperation.
6 What are the ages that need to be considered in orthodontic care?
Chronologic, skeletal, dental, mental, and emotional age are differentiated in the assessment of the development of a patient. Chronologic age does not correlate well with the other ages; thus, assessment of the skeletal or physiologic age helps to determine the biologic age.
7 What methods can be applied to assess the physical growth and maturation status of an individual?
Evaluation of the skeletal maturity of a patient is important to maximize efficiency and effectiveness of orthodontic treatment through proper timing. If a treatment plan demands a skeletal dentofacial orthopedic modification, the patient should be treated as close as possible to the peak velocity of growth.
More recently, it has been shown that the peak pubertal growth can also be estimated by evaluation of the maturation level of the cervical vertebrae pictured on a cephalographic radiograph.
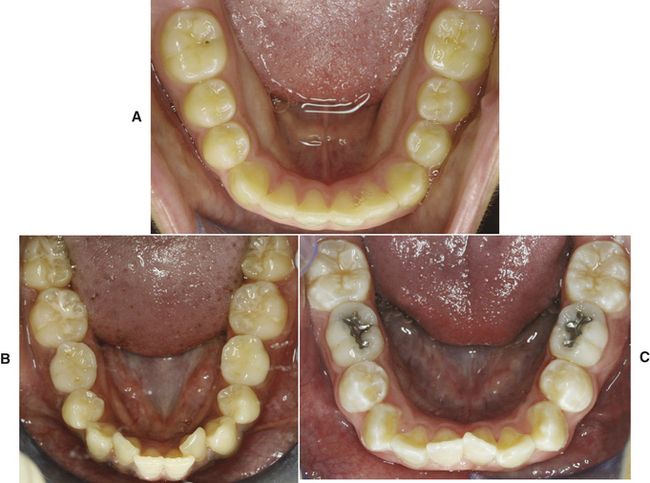
8 How is the malposition of individual teeth classified?
A malposed tooth can be inclinated, centrically or eccentrically malpositioned, totally displaced, rotated, transposed, or localized by various combinations thereof. According to Liescher’s nomenclature, the malposition of a tooth is termed mesioversion if it is displaced toward the facial midline (

FIG 4-2 A, Mesioversion of maxillary right central incisor. B, Distoversion of maxillary right lateral incisor. C, Labioversion of maxillary left central incisor. D, Linguoversion of maxillary central incisors. E, Infraversion of mandibular left second deciduous molar. F, Transposition of maxillary right cuspid and first premolar.
If an incisor or canine is misplaced outside the arch form toward the lip, this is described as labioversion (
9 Which tooth most often displays an anomaly?
In general, third molars are most commonly affected by size and shape variations, followed by upper lateral incisors and lower second premolars. Anomalies can result from genetic factors as well as environmental influences such as nutrition or diseases during the prenatal period of tooth development. Upper lateral incisors have been described as absent, peg-shaped, hypoplastic, dens evaginatus or invaginatus. Peg-shaped laterals are found in 1% to 2% of the population and are characterized as being small, conical, and tapered toward the incisal (
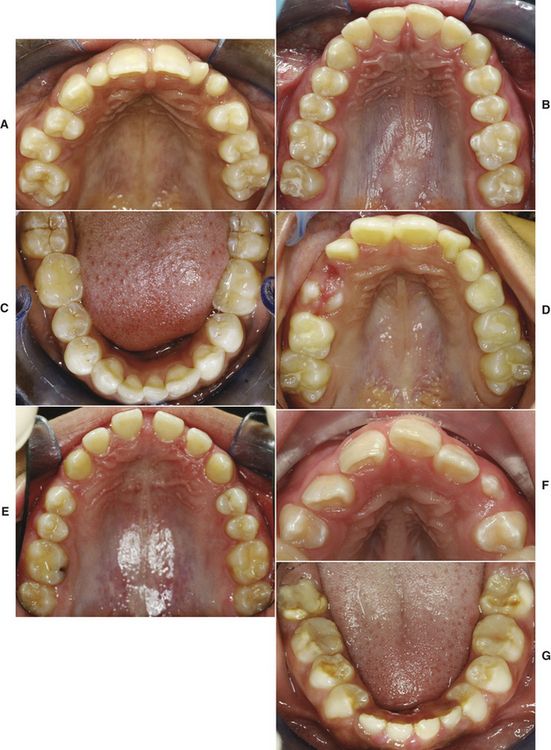
FIG 4-3 A, Maxillary peg lateral incisors and retained left deciduous cuspid. B, Cusp of Carabelli on maxillary first molars. C, Gemination of mandibular central and lateral incisors. D, Dens in dente with talon cusp. E, Microdontia of maxillary tooth with generalized spacing. F, Macrodontia of maxillary lateral incisors. G, Amelogenesis imperfecta.
Shovel-shaped incisors mark another morphological variant. These teeth show pronounced lingual ridges and cingula and are more common in the Asian, Eskimo, and Native American populations.
The term taurodontia describes a tooth whose crown and pulp chamber is elongated with little or no constriction at the cementoenamel junction (CEJ), resulting in a short root. The incomplete division of a single tooth germ is known as gemination (
These teeth clinically appear as fused with a notch in the crown but generally display a single root and pulp chamber. Truly fused teeth, however, result from union of the dentin of two adjacent tooth buds. Consequently, tooth count will normally reveal one less individual tooth in the affected arch. Twinning is the complete division of one tooth germ into two teeth, resulting in one more individual tooth than the normal complement. If two adjacent teeth are joined only at the cementum, they are described as being concrescent.
A dens evaginatus is characterized by a talon cusp (
The teeth can be hypoplastic (microdontia) (
Mineralization abnormalities can also be observed sporadically or as part of a syndrome such as dentinogenesis and amelogenesis imperfecta (
ORTHODONTIC MODELS
10 What are the significant areas of cast analysis?
Dental casts obtained from impressions that extend far enough into the sulcus to allow accurate reproduction of the soft tissue anatomy should accurately represent the dentition and immediate supporting structures. The objective of study cast analysis is the 3D assessment of the maxillary and mandibular dental arches and their occlusal relationships. This encompasses the metric analysis of arch width, length, symmetry, and palatal height as well as tooth size and space analysis in relation to the apical bases and examination of the interarch occlusion. The apical base arch is the area of alveolar bone on the level of the root apices of the teeth, whereas the basal arch is formed by the maxillary and mandibular corpus. Its dimensions are stable and unaffected by tooth loss or alveolar resorption. The dental arch perimeter is measured through the contact points of the teeth and ideally should be congruent to the sizes of the alveolar and basal arches. It should be noted that the mandibular arch is often referred to as the diagnostic arch because of the cortical bone on the facial and lingual surfaces. In contrast to the intermolar width, which significantly increases in the maxillary arch between 3 and 13 years of age, the mandibular intercanine distance increases during the transition of primary to permanent dentition
As part of the cast analysis, the individual arch shape should be appreciated. It has been shown that the most common arch form is the ovoid arch, followed by tapered and squared arch shapes (
Arch length discrepancy, also referred to as arch circumference discrepancy, is identified as the difference between the available arch length and the required arch length. It is determined by measuring the mesiodistal tooth widths of the permanent teeth from the mesial of the permanent mandibular first molars for the mandibular arch and permanent maxillary first molars for the maxillary arch.
11 What is the Bolton analysis?
The Bolton analysis offers a method to determine the ratio of the mesiodistal widths of the maxillary versus the mandibular permanent teeth, also known as tooth size discrepancy, and its interarch effects. When looking at interarch relationships, it is essential to treat the anterior teeth separately from the posterior units. Tooth size discrepancies in the anterior region can be corrected only with compensations in the anterior region and not through treatment changes in the posterior teeth. Thus, the Bolton analysis consists of an anterior ratio analysis, designed to identify incompatibilities in anterior teeth, or a whole dentition ratio, which, when compared to the anterior ratio, determines the discrepancies of the posterior teeth. The anterior ratio is calculated by dividing the sum of the mesiodistal widths of the mandibular six anterior teeth by the sum of the mesiodistal widths of the maxillary anterior teeth and then multiplying the result times 100. The mean anterior ratio is 77.2, whereas the mean overall ratio is 91.3. The latter is calculated according to the same principle as the anterior ratio but is calculated by dividing the sum of the mesiodistal widths of the mandibular right first molar tooth to the left first molar tooth by the sum of the mesiodistal widths of the maxillary first molar to first molar teeth.
12 What represents the basis for Angle’s dental classification?
The Angle classification, first published in the 1890s, is based on the anteroposterior occlusal relationship of the permanent first molar that was termed the key to occlusion. According to Angle, a Class I normal occlusion is defined by the interlocking of the mesiobuccal cusp of the upper first molar into the mesiobuccal g/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses