4 Endodontic Diagnosis
The goal of endodontic diagnostic procedures is to determine the condition of the pulp and the periradicular tissue. Diagnosis is difficult because it is impossible to directly inspect the pulp and the clinician has to rely on indirect methods of examination.
Patients who present with pain in the facial region often have pulpal or periradicular disease. Within a very short period, the dentist must arrive at the proper diagnosis and devise a targeted clinical and therapeutic regimen which relieves the patient’s pain and assures long-term maintenance of the affected tooth. In terms of the appointment structure within the dental practice, this presents an important challenge for the dentist. However, no diagnostic method has perfect sensitivity and specificity. Knowledge gleaned from the patient’s chief complaint, medical/dental history, appropriate clinical tests, and differential diagnosis, will in most cases lead to an accurate diagnosis and subsequent successful treatment.
The absence of clinical symptoms does not necessarily mean that the pulp is completely healthy. In the case of infection with bacteria with minimal virulence, or in the case of strong immunologic resistance within the pulpal tissues, a transient acute inflammation can become chronic and be detected by chance, for example due to crown discoloration or lack of pain or painlessness during the placement of a restoration. Conversely the acute phase may develop within a chronic process. Infection may also be primarily acute. Pain as a diagnostic criterion of endodontic disease has relatively low sensitivity. According to Langeland et al. (1994), there is no correlation between clinical signs and symptoms and the histopathologic status of the pulp, although in one study 80% of the patients who presented with dental pain had histological evidence of an irreversible alteration within the pulp (Dummer, 1980). There is also no direct correlation between the severity of pain and the progression of the inflammatory process, (i.e., between the specific types of bacteria and the clinical symptoms) (Dummer, 1980).
To quickly establish an appropriate working diagnosis, it is wise to follow a systematic procedure (e.g., from the outside to the inside). All clinical investigations regarding pain intensity should always be interpreted in comparison with the adjacent and/or contralateral teeth. This helps to establish clear comparisons with regard to both the objective and subjective reactions of each individual patient. In the case of multirooted teeth, the diagnosis is rendered much more difficult due to the different histopathologic conditions within the pulp of the individual root canals.
Tenderness to percussion indicates an extension of pulpal inflammation into the periapical tissue (e.g., periodontal ligament). Pulpitic and/or periapical discomfort may radiate to other areas of the jaw and face, but almost never crosses the facial midline (Seltzer et al., 1963). Pain originating from the mandibular teeth is often referred to the periauricular area, and pain originating from maxillary teeth may be referred up to the temple.
If the patient reports bilateral pain, one must consider systemic disease rather than pain of odontogenic origin. In such cases, although a patient may believe that the teeth are the origin of their discomfort, the pain is actually originating elsewhere. Natkin et al. (1975) observed cardiac etiologies in 18% of patients presenting with supposed tooth pain. The possible pulpal and periapical diagnoses are listed below (the transition between the individual pulpal states is sometimes vague):
• clinically healthy pulp;
• reversible pulpitis;
• irreversible pulpitis;
• necrosis;
• apical periodontitis (acute or chronic).
Medical History and Clinical Examination
The information gleaned from the patient’s medical history should clarify whether the patient has any systemic medical disease or whether any medications are being taken that could influence the treatment and prognosis of endodontic therapy. The best method for taking a medical history is to use a standardized questionnaire.
In general, there are no contraindications to endodontic treatment; however, each patient’s physical and psychologic condition should be considered. If the dentist is in any way uncertain, the patient’s general physician or a medical specialist should be consulted before the initiation of endodontic treatment.
As a basic principle, the medical history should be reviewed and updated before each endodontic appointment. If the medical history reveals pre-existing conditions such as endocarditis, heart valve replacement, or rheumatic fever, antibiotic prophylaxis is indicated before root canal therapy. In the case of other conditions such as glaucoma, asthma, or pregnancy, epinephrine-containing anesthetic solutions should not be used. In patients with diabetes, human immunodeficiency virus (HIV) infection, or following radiation therapy, one must remember that the course of healing will be longer. It is also critically important to note the presence of any allergies (e.g., latex, penicillin).
4.1 Patient information
The patient’s dental history must include questions concerning previous dental visits, recently placed restorations or pulp capping procedures, and any previous complications associated with dental treatment.
If a patient presents as an emergency, the primary complaint should first be recorded briefly in the patient’s own words. Details to be documented include pain localization, duration, and quality/quantity, as well as any stimuli that trigger, increase, or relieve the pain. After questioning the patient, a comprehensive examination of the entire intraoral environment should be carried out. If a tooth is suspected of requiring endodontic treatment it should be assessed in terms of restorability and strategic importance.
The decision about endodontic treatment should be made only after a comprehensive assessment of the clinical findings, the primary complaint, medical/dental history, and the differential diagnosis, which is the only relatively reliable way to reach an accurate diagnosis. This allows rapid planning of targeted therapy to reduce the patient’s discomfort.
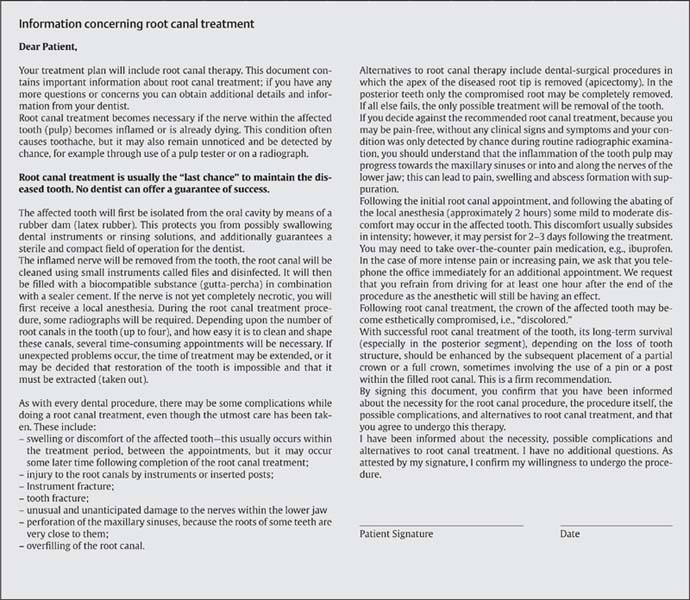
It is obligatory to inform the patient not only about the prognosis and procedures involved in endodontic therapy, including the necessity for numerous radiographs, possible complications, but also about the financial burden of the endodontic therapy itself and subsequent costs of necessary prosthetic treatments after successful root canal therapy.
Extra- and Intraoral Examination
The extraoral examination begins when the clinician greets the patient. During this time any atypical external facial features should be noted including facial asymmetry (e.g., swelling, skin color, the appearance of fistulae and localized redness, etc).
Extraoral bimanual palpation, including a comparison of the submandibular and cervical lymph nodes on both sides may provide clues about any spread of infection or the presence of tumorous diseases. It is essential to clarify whether a localized or generalized condition represents the etiology of any abnormality noted. The masticatory muscles should be palpated bimanually. The mouth opening should also be checked: It should be at least three fingers’ wide for root canal treatment to be carried out.
The intraoral examination includes an assessment of the general dental status combined with careful examination of the hard and soft tissues for swellings, sinus tracts, crown discoloration, or tooth mobility. The condition of the hard and soft tissues (tongue, lips, cheeks, palate, and neck) as well as the status of the dentition, the periodontium, and the oral hygiene, and number and quality of dental restorations should be recorded.
4.2 Extraoral examination
Left: Submandibular abscess extending posteriorly from the mandibular left second molar.
Right: Extraoral cutaneous fistula caused by odontogenic infection.