42 Tooth Resorption
Resorption can be a physiologic or a pathologic process, and results in loss of dentin, cementum, or bone. Resorption may occur subsequent to traumatic dental injuries, orthodontic treatment, or chronic infections of the pulp or periodontal tissues.
Under normal circumstances, the mineralized tissues of permanent teeth are resistant to resorption. They are protected by a layer of predentin and precementum, on which clastic cells cannot gain foothold. If, however, this protective layer is damaged or altered by an injury in conjunction with an inflammation of the pulp or periodontal tissues, then multinucleated clastic cells will induce resorption.
Tooth resorption is classified on the basis of the site, nature, and pattern of the process (Ne et al., 1999). A distinction is generally made between internal and external resorption. External resorption can be further subdivided into external surface resorption, invasive cervical resorption, inflammatory root resorption, ankylosis, and replacement resorption.
Internal resorption is the only type of resorption that starts within the root canal, and it frequently results from chronic inflammation of the pulp. Vital pulp tissue is a prerequisite for active internal resorption. In the initial stage, the coronal portion of the pulp is totally or partially necrotic, whereas the apical pulp, which includes the internal resorption defect, can remain vital and inflamed. Therefore, pulp sensibility tests can remain positive (Trope, 2002).
Internal resorption is generally asymptomatic and is usually identified by chance on routine radiographs.
External surface resorption is a transient phenomenon in which the root surface undergoes spontaneous destruction and repair. It is found in all teeth, in varying degrees, and is probably a normal physiologic response. Hence, it requires no treatment (Ne et al., 1999).
Invasive cervical resorption is an insidious and often aggressively destructive form of external tooth resorption. It is a relatively uncommon condition that may occur in any tooth of the permanent dentition. It is characterized by invasion of the cervical region of the root by fibrovascular tissue, derived from the periodontal ligament. This resorptive process leads to progressive loss of tooth structure and may eventually invade the pulp space. However, the pulp survives until late in the resorptive process, because it is protected by the predentin and odontoblasts (Heithersay, 1999a). The etiology of this condition is poorly understood, but intracoronal bleaching, trauma, orthodontics, dentoalveolar surgery, and periodontal treatment have been cited as potential predisposing factors (Heithersay, 1999b).
In inflammatory root resorption, the necrotic, infected pulp provides the stimulus for periodontal inflammation. The most common cause of external inflammatory root resorption is trauma. If the cementum has been damaged, leaving the dentinal tubules exposed, this creates an open communication between the internal and external surfaces of the root. Bacteria and their byproducts, and tissue breakdown products from within the pulp space, diffuse through the dentinal tubules and stimulate an inflammatory response over large areas of the periodontal ligament, leading to aggressive and progressive resorption of the root (Andreasen, 1981).
Ankylosis and replacement resorption are primarily associated with a history of luxation injuries, in particular in avulsed teeth with an extended extra-oral dry time. If osteoblasts are able to cover the root surface after necrosis of the periodontal ligament, direct contact with bone and root will occur over some areas of the root surface. The term for this condition is ankylosis. Reversal of ankylosis is possible if less than 20% of the root surface is involved. If not, the root will gradually be replaced by bone (Tronstad, 1988).
Diagnosis of Resorption
It can be difficult to distinguish between invasive cervical resorption and internal root resorption. This may result in an inaccurate diagnosis and subsequently incorrect treatment.
Radiographically, internal resorption appears as a circumscribed, oval-shaped enlargement of the root canal space. The outline of the root canal is often distorted, and the resorption appears to be contiguous with the root canal. Regardless of the projection angle of the radiograph, internal resorption remains centered in the root.
Invasive cervical resorption moves away from the canal if the angle of projection of the radiograph is changed. In addition, the root canal outline appears normal and can usually be identified through the defect, in contrast to internal resorption.
Clinically, the presence of a pink spot in the coronal dentin can be a feature of both internal and invasive cervical resorption. This phenomenon occurs due to the presence of granulation tissue just under the enamel. In both conditions, a pulpal sensibility test is likely to be positive, because the pulp remains (partially) vital.
42.1 Invasive cervical resorption
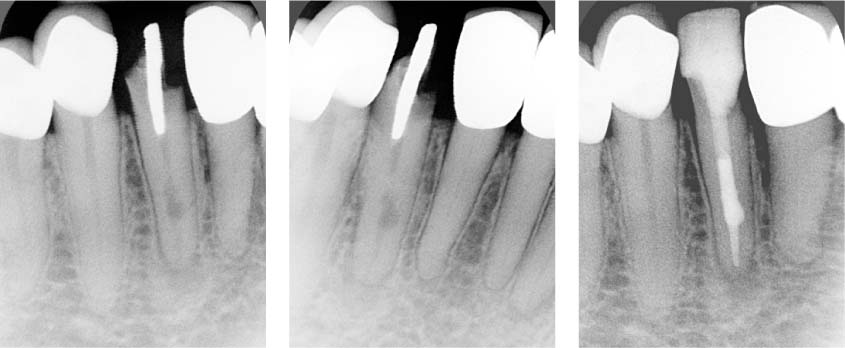
Left: Perpendicular periapical radiograph showing an internal resorption defect on tooth 42 with an apical radiolucency. Note the oval, circumscribed radiolucent enlargement of the root canal.
Middle: A radiograph taken from a different horizontal angle shows that the defect stays centered in the root.
Right: Postoperative radiograph confirms that the entire canal including the internal resoption defect has been filled, in this case with MTA. Failure to achieve this would indicate the presence of external resorption defect.
42.2 Invasive cervical resorption
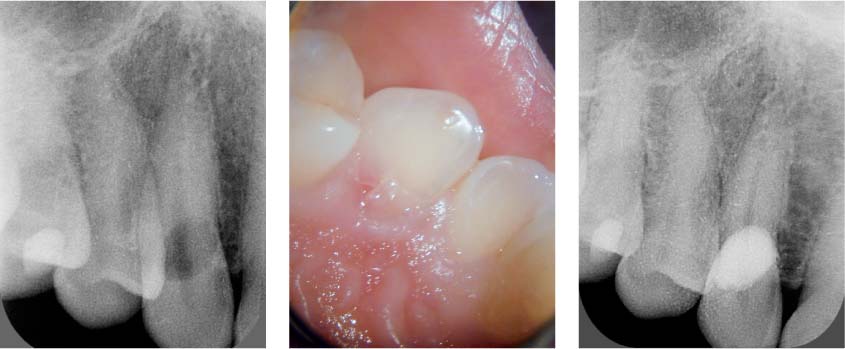
Left: Radiograph showing invasive cervical resorption on tooth 13. The outline of the canal is clearly visible through the resorption defect. The tooth tested vital.
Middle: A pink spot on the palatal surface indicates the presence of granulation tissue undermining the enamel.
Right: The 1.5-year follow-up radiograph showing the resorption defect restored with a composite filling.
Pulpal sensibility tests were positive, and there were no signs of periapical pathosis.
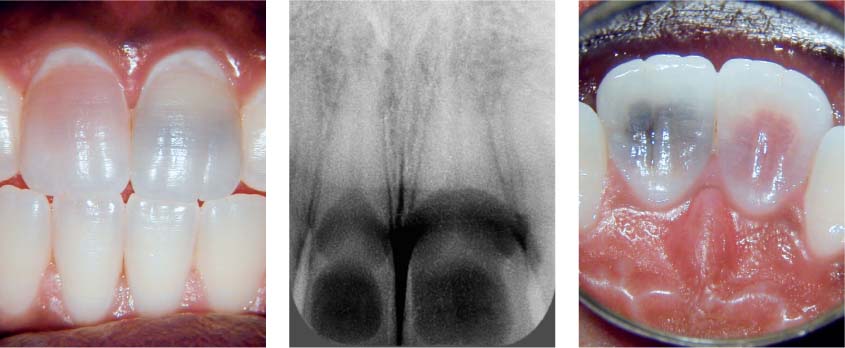
42.3 Severe internal resorption on two maxillary central incisors
Left: Teeth 11 and 21 exhibiting reddish and black discoloration, due to internal resorption, respectively.
Middle: Extensive radiolucencies in the coronal and cervical segments of the root canals of 11 and 21.
Right: Palatal aspect of affected central incisors. The teeth have been significantly weakened as a result of the resorption. Soon after the initial examination, the crown of tooth 11 broke off.
Pressure has also been identified as a possible etiological factor for external inflammatory root resorption, as evidenced by resorption that may occur in conjunction with orthodontic tooth movement,/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses