4
Endocrine and Metabolic Disorders
Endocrine and metabolic disorders of particular importance to dentistry include disorders of the pancreas, adrenal glands, and thyroid gland, and as such, this chapter is divided into three sections.
Section 1. Pancreatic Diseases
I. Background
Description of Disease
Diabetes Mellitus (DM)
DM is a hormonal metabolic disorder of multiple etiologies characterized by chronic hyperglycemia resulting from deficiencies in insulin secretion or function or both.
Pancreatic Cancer
The pancreas is a major endocrine and digestive organ that produces hormones, including insulin, glucagon, and somatostatin, and secretes pancreatic juice containing digestive enzymes that assist the absorption of nutrients and digestion in the small intestine. Cancer of the pancreas has a median survival of 6–12 months. This grim outcome largely relates to the aggressiveness of the malignancy, difficulty in establishing early diagnosis, low rate of resection, and lack of an effective chemotherapy agent to treat the tumor.
Pathogenesis/Etiology
DM
Sustained hyperglycemia adversely affects all body tissues. Classic complications of DM include retinopathy, nephropathy, neuropathy, macrovascular disease (cardiovascular, cerebrovascular, peripheral vascular), altered wound healing, and possibly increased incidence and severity of periodontal diseases. These effects may become more profound in diabetics who smoke or have other major medical conditions.
Classification:
- Type 1 DM is immune mediated. The autoimmune response usually occurs in children and young adults accounting for 5–10% of all diabetics. Individuals with type 1 DM require insulin supplementation for life. Undiagnosed type 1 DM is associated with the classic symptoms of polydipsia (excessive thirst), polyurea (frequent urination), and polyphagia (excessive hunger), and if untreated, it can lead to ketoacidosis, coma, or death.
- Type 2 DM is characterized by impaired insulin resistance, and it may be associated with low, normal, or increased insulin production. It occurs most commonly in adults and is associated with obesity or the metabolic syndrome. Increasing obesity and reduced physical activity among children have resulted in a markedly increased incidence of type 2 DM in younger individuals.
- Gestational DM may affect 7% of pregnant females in the United States resulting in more than 200,000 new cases annually.1 It is defined as increased insulin resistance that develops during pregnancy. Gestational DM is more common in women who are obese and who are at increased risk for other adverse pregnancy outcomes. It may lead to significant perinatal morbidity and mortality, as well as obesity and diabetes in the offspring. After delivery, most women return to a normoglycemic state but 30–50% will subsequently develop type 2 DM within 10 years.
- Prediabetes (increased risk for DM): Glucose levels are higher than normal but not high enough for a diagnosis of DM.
- Metabolic syndrome: The presence of certain risk factors increases the likelihood of developing type 2 DM. These include a positive family history, obesity, and a cluster of factors sometimes referred to as the metabolic syndrome (dyslipidemia, hypertension, visceral obesity; abnormal coagulation factors; and endothelial dysfunction). These factors collectively increase insulin resistance, induce hyperinsulinemia, and impair glucose tolerance.
- Impaired glucose tolerance (IGT): Affected individuals are usually normogylcemic but may develop hyperglycemia after large glucose intake.
- Impaired fasting glucose (IFG): Glucose levels respond normally after food consumption but fasting glucose levels remain somewhat elevated.
- Both IGT and IFG are associated with increased insulin resistance. Type 2 DM may develop in 40–50% of affected individuals within 10 years of onset. Type 2 DM may sometimes be prevented if treatment is initiated in individuals who have IGT or IFG.2
Pancreatic Cancer
Ductal adenocarcinoma accounts for >80%. Most arise in the pancreatic head and act in a highly aggressive manner with frequent invasion of the vascular, lymphatic, and perineural tissue. In most instances, it affects the exocrine (digestive enzyme producing) portion of the pancreas, but the endocrine (insulin producing) portion may be affected as well. Causes remain unknown, with smoking, DM, and genetics being likely risks.3
Epidemiology
DM
DM has reached epidemic proportions in the United States and around the world, and its impact is worsened by the fact that many diabetics are unaware that they have the disease. U.S. statistics are reported annually by the Centers for Disease Control and Prevention (CDC):
- Incidence: In 2010, 1.9 million Americans >20 years of age were newly diagnosed with DM.
- Prevalence: In the United States, 25.8 million children and adults (8.3% of the U.S. population) had DM of which 7.0 million were undiagnosed. Prediabetics (persons at risk) were estimated at 79 million people.
- Race/Ethnicity: Minority populations are at higher risk. DM occurs in 7.1% of non-Hispanic whites, 8.4% of Asian-Americans, 11.8% Hispanics, and 12.6% non-Hispanic blacks.
- Mortality: DM is the seventh leading cause of death in the United States.
Pancreatic Cancer
It is the fourth leading cause of mortality from cancer, primarily because <20% of patients present with localized potentially curable tumors.3 Individuals of both sexes and all races may be affected. For 2011, there are estimated to be 44,030 new cases and 37,660 deaths from pancreatic cancer.
 Coordination of Care between Dentist and Physician
Coordination of Care between Dentist and Physician
DM
The dentist should review the patient’s medical history, take vital signs, and evaluate for oral signs and symptoms of undiagnosed or inadequately controlled DM. If the patient has severe periodontal disease, the physician should be reminded that periodontal therapy may improve metabolic control and allow adjustments in drug dosages. Medical consultation may be necessary to determine health status and if planned dental treatment can be safely and effectively accomplished. The physician should provide laboratory test results to the dentist on request and make the dentist aware of any diabetic complications that may be present. On occasion, the physician may need to adjust the patient’s DM medications to insure sustained metabolic control before, during, and after surgical procedures.4
Pancreatic Cancer
Because of the aggressive nature and current unavailability of effective screening tools, the dentist is unlikely to be asked to provide definitive elective treatment for the patient with active pancreatic cancer. However, emergency dental care may be needed. If so, the physician should be queried about planned medical treatment and when it is to be accomplished. Optional dental treatment should be coordinated so as not to interfere with planned surgery, radiation therapy, or chemotherapy.
 II. Medical Management
II. Medical Management
Identification/Medical History/Physical and Laboratory Examination
DM
The American Diabetes Association and World Health Organization recognize four suitable tests to diagnose DM. Plasma glucose can be measured in a fasting state, randomly (nonfasting), or 2 hours after consumption of a measured quantity of glucose. Abnormal findings must be present on two separate occasions to establish the diagnosis. See Table 4.1.
Table 4.1. American Diabetes Association Diagnostic Criteria for Diabetes Mellitus
| Diagnostic Test | Test Result Diagnostic Criteria |
| Fasting plasma glucose | ≥126 mg/dL (7.0 mmol/L) |
| Random plasma glucose | ≥200 mg/dL (11.1 mmol/L) |
| 2-hour plasma glucose (after 75 oral glucose load) | ≥200 mg/dL (11.1 mmol/L) |
| HbA1c (glycated hemoglobin) | ≥6.5% |
Determination of glycated hemoglobin (HbA1c) percentage has recently been added as a diagnostic tool for DM with an HbA1c ≥6.5% indicating DM. HbA1c is also used to monitor long-term metabolic control because it evaluates blood glucose levels over a period of 30–90 days.5,6
| Normal range | <6% |
| Good control | <7% |
| Moderate control | 7–8% |
| Poor control | >8% |
Pancreatic Cancer
- Screening: Currently, it is neither advisable nor cost-effective to screen the general population for pancreatic cancer, but it is customary to screen individuals who are at high risk. A mechanism for early diagnosis is badly needed and the use of salivary biomarkers offers great promise as one such mechanism.7
- Diagnosis: Diagnosis is usually based on physical examination and evaluation of signs and symptoms (weight loss, jaundice, abdominal bloating and pain, malaise, diarrhea, nausea, elevated blood sugar). Specific tests include computed tomography (CT), ultrasound, endoscopy and possibly needle biopsy.
Medical Treatment
DM
A primary goal of diabetes care management is to maintain an HbA1c ≤7% so as to reduce microvascular and neuropathic complications.8
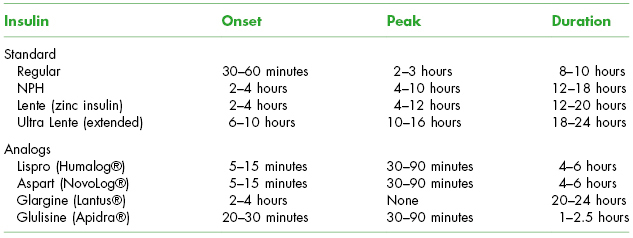
Type 1 DM requires insulin supplementation. Insulins are classified as rapid, short, intermediate, or long acting. Each class induces variable onset of peak activity and duration. See Table 4.2. Patients frequently use a combination of the various types in order to maintain a normal or near-normal level of plasma glucose.
Table 4.2. Standard Insulins and Insulin Analogs
Type 2 DM may be treated with weight loss, exercise, and oral antidiabetic medications that improve carbohydrate metabolism, decrease insulin resistance, or increase insulin production. See Table 4.3. Over time, individuals with type 2 DM may experience a reduction in insulin production and consequently require insulin supplementation.
- Prognosis: Prognosis is good for diabetics who respond adequately to insulin, oral antidiabetic medications, weight loss, and exercise. However, diabetes affects multiple organs, and even with treatment, diabetics are at increased risk for blindness, kidney failure, heart disease, stroke, limb amputation, and peripheral neuropathy. Diabetics who maintain rigid control of their blood glucose at normal or near-normal levels are much less likely to experience these complications.5
Table 4.3. Oral Antidiabetic Medications
| Medication Class/Drugs | Action |
| Sulfonylureas | Stimulate insulin secretion |
| Glyburide | |
| Glipzide | |
| Glimepiride | |
| Meglitides | Stimulate rapid insulin secretion |
| Repaglinide | |
| Nategline | |
| Biguanides | Block liver production of glucose |
| Metformin | |
| Thiazolidinediones | Improve insulin sensitivity |
| Rosiglitazone | |
| Proglitazone | |
| Alpha-glucosides | Slow carbohydrate absorption |
| Acarbose | |
| Meglitol | |
| Combination agents | Multipurpose |
Pancreatic Cancer
It can be cured if diagnosed early and surgical removal is complete. Chemotherapy, radiation therapy, and targeted therapy may enhance and prolong life.
 III. Dental Management
III. Dental Management
Evaluation
DM
Diabetics require a complete medical history supplemented by careful questioning regarding their status.
It is often prudent to discuss the patient’s medical status with the physician and obtain medical input before performing invasive dental therapy, particularly in the poorly controlled diabetic.
Pancreatic Cancer
Patients and their physicians should be queried regarding the course of treatment and the patient’s overall health status.
 Key questions to ask the diabetic patient
Key questions to ask the diabetic patient- What type of diabetes do you have?
- How old were you when diabetes was diagnosed? How long has it been since the diagnosis?
- What medications do you take?
- How do you monitor your blood sugar levels?
- How often do you see your doctor about your diabetes? When was the last visit to your doctor?
- How does your doctor monitor your blood sugar levels?
- What was the most recent HbA1c (A1C) result?
- Do you ever have episodes of very low or very high blood sugar?
- Do you ever find yourself disoriented, agitated, and anxious for no apparent reason?
- Do you have any mouth sores or discomfort?
- Does your mouth feel dry?
- Do you have any other medical conditions related to your diabetes, such as heart disease, high blood pressure, history of stroke, eye problems, numbness of limbs, kidney problems, delays in wound healing, history of severe gum disease? If so, what?
 Key questions to ask the diabetic patient’s physician
Key questions to ask the diabetic patient’s physician- What medications does the patient take? Is the patient compliant with the prescribed drug regimen?
- Does the patient have a history of diabetic hyperglycemic or hypoglycemic crisis?
- What are the most recent laboratory findings for the patient, in particular the HbA1c?
- Does the patient have other medical problems that might affect dental care?
- Do you feel prophylactic antibiotics are indicated prior to dental procedures?
 Key questions to ask the pancreatic cancer patient
Key questions to ask the pancreatic cancer patient- When was your cancer diagnosed?
- What treatments have you had or are proposed?
- Do you have other medical conditions related to your cancer such as DM, thyroiditis, Addison’s disease, or Cushing’s disease?
- During your cancer therapy have you developed any problems with excessive or prolonged bleeding?
 Key questions to ask the pancreatic cancer patient’s physician
Key questions to ask the pancreatic cancer patient’s physician- What is the course of treatment for this patient? What are the adverse effects of the treatment?
- Does the patient have other medical problems that might affect dental treatment?
- Do you feel the patient will be able to tolerate the dental treatment without difficulty?
- Are any special precautions indicated during dental treatment?
- Are there contraindications to use of local anesthetics, parenteral conscious sedation, oral sedation, or antibiotics?
- Is the patient likely to have excessive or prolonged bleeding following an invasive dental procedure?
- Do you feel prophylactic antibiotics are indicated prior to dental treatment?
Dental Treatment Modifications
DM
The well-controlled diabetic can usually be managed conventionally to include most surgical procedures.
- Maintenance of a normal postsurgical diet is important. If this is not possible, dietary supplements should be recommended.
- Occasionally, it may be necessary for the patient’s physician to modify insulin protocols to insure a stable postoperative outcome. Patients may require reduction of insulin dose immediately prior to oral surgical procedures that will result in reduced calorie oral intake so as to prevent unintended hypoglycemia.
Marginally or poorly controlled diabetics should be treated with caution. Elective dental treatment should be avoided until the patient is stabilized. If the patient has associated medical complications, apply appropriate steps necessary in management. Patients should be encouraged to maintain excellent oral hygiene and comply with recall appointments. If dental caries is a potential problem, fluoride-containing, caries-preventive agents are appropriate. Xerostomia should be managed on a case-by-case basis.
It is well known that in patients with poor glycemic control, surgical stress promotes hyperglycemia through the release of various hormones and inflammatory cytokines, possibly predisposing them to poor wound healing, surgical site infections, and even diabetic ketoacidosis. However, glycemic control has not been shown to influence the rate of postextraction epithelialization and thus healing in diabetic patients.9 Dental implants can usually be successfully placed in well-controlled diabetics and possibly in moderately controlled individuals. However, implant placement in poorly controlled diabetics has an unpredictable prognosis and, if possible, should be avoided.10
Pancreatic Cancer
- Elective dental treatment is not indicated during cancer treatment.
Oral Lesion Diagnosis and Management
DM
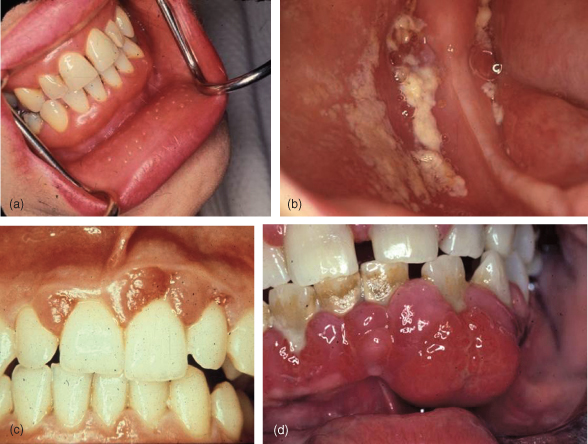
Oral manifestations of undetected or poorly controlled DM are common. See Fig. 4.1. They may include xerostomia, burning mouth (possibly due to neuropathy), delayed wound healing, increased incidence and severity of infections, enlargement of parotid salivary glands, gingivitis, and periodontitis.11 Conversely improved periodontal health may facilitate metabolic control.12 The effect of DM on caries risk is unclear. Candidiasis is a frequent secondary infection in the presence of xerostomia and among denture wearers.13
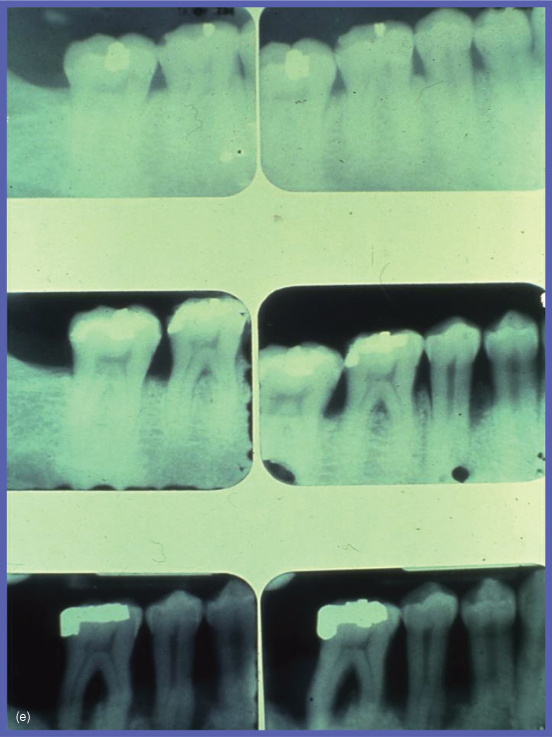
Figure 4.1 Oral signs of undiagnosed/uncontrolled diabetes mellitus. (a) Xerostomia; (b) chronic candidiasis; (c) multiple periodontal abscesses; (d) severe periodontal disease; (e) rapidly progressive alveolar bone loss over a 2-year period of time.
Pancreatic Cancer
Some evidence suggests that poor oral health may slightly, but significantly, increase risk for pancreatic and other cancers. However, a cause–effect relationship has not been established, and individuals with oral infection share some risk factors (smoking and possibly genetic similarities) with those with pancreatic cancer. At any rate, cohorts of individuals with pancreatic cancer can be expected to have more tooth loss and periodontal disease than the general population.14,15
 Risks of Dental Care
Risks of Dental Care
Hemostasis
Susceptibility to Infection
Drug Actions/Interactions
Patient’s Ability to Tolerate Dental Care
Medical Emergencies
Be prepared to manage diabetic emergencies. Although rare, hyperglycemia can be life threatening and is seen far less frequently in type 2 diabetics. Both type 1 and type 2 diabetics are much more likely to experience hypoglycemia during dental treatment in this era of “tight” glycemic control.16
- Onset is usually slow, and consequently, ketoacidosis and hyperglycemic crisis are rare in the dental office.
- Signs include mental disorientation, sweating, coma, and even death.
- Patients with ketoacidosis require medical treatment, so activate the emergency medical system, administer oxygen, monitor vital signs, and perform cardiopulmonary resuscitation if needed.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


