4
Different Implant–Abutment Connections
1Department of Oral and Maxillofacial Surgery, Washington Hospital Center, Washington, DC; and American Institute of Implant Dentistry, Washington, DC
2Private Practice, Gilbert, AZ
Introduction
The history of abutment connections began with Branemark’s landmark discovery of the dental implant. Branemark’s original implant was composed of a 0.7 mm external hex with a butt joint. Initially there was little interest in antirotational features of the abutment connection because implants were used to treat fully edentulous patients and were connected together with a one-piece metal substructure. The external hex portion of the implant was added to the design to enable surgical placement of the implant.
Times changed and clinicians started using implants for the replacement of single teeth. This new application meant that abutment connections were subjected to an increased level of forces. This challenge has encouraged research and the development of better forms of abutment connections within the implant dentistry.
Chronological Development of Abutment Connections
The abutment modifications that have occurred are vast and complex. For example, the external hex underwent several modifications of height and width. Besides altering the size, other modifications were also made in an effort to improve upon the original external hex design.
A major paradigm shift came with the evolution of the internal connection. Each implant company has developed their own design of the internal connection, resulting in a confusing variation in terminology and types of connections.
The initial relationship between the abutment and implant body was mainly associated with external connections. Over time the simple butt joint has evolved into slip-fit and friction-fit joints. The internal connections have splintered into a multitude of options from octagonal, hexagonal, cone screw, cylinder hex, spline, tri-channel to cam tube – to name just a few.
This chapter examines the basic differences between the abutment connections on the market and should enable readers to make educated decisions in selecting implant–abutment connections.
External Hex Connections
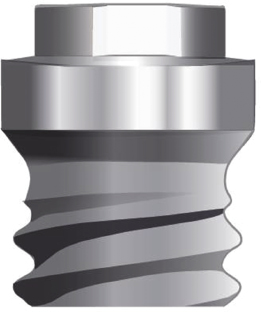
There are a number of advantages and disadvantages of the external hex connection (Figure 4.1) shown in the boxes.
Prosthetic success remains high with the external connection but the most common prosthetic complication is screw loosening when implants are used to replace a missing single tooth. Multiple studies have shown screw loosening to be anywhere from 6% to 48% with external connection devices.
Screw loosening can create serious challenges for the clinician and patient and diminishes a practitioner’s chairside time, which is the most valuable asset a practitioner has. In addition, screw loosening can be frustrating for patients, which damages the patient’s trust in the clinician’s qualifications and abilities.
When an external hex implant is used to replace a single tooth, the weakest link between the implant, abutment connection, screw, and bone is the screw. This is because with this connection type the screw alone secures the abutment.
External Connection
The initial 0.7 mm external connection, being short in length, provided only limited screw engagement. The original narrow platform associated with the external hex connection created a short fulcrum arm, which also increased screw loosening due to adverse tipping forces. Consequently, the short and narrow external connections made screw loosening a common occurrence. Research clearly indicates that screw loosening is more common with external connections. The seriousness of screw loosening resulted in manufacturers implementing major modifications to the external hex connection.
Modifications
The first solution to overcome the adverse force distribution and instability of the abutment connection was increasing the width and height of the external hex connection. Currently available external hex heights range from 0.7 to 1.2 mm and widths from 2.0 to 3.4 mm, depending on the manufacturer. These adjustments increased the fulcrum arm and deepened the abutment screw engagement, thus limiting the tipping forces on abutment screws and reducing the prevalence of screw loosening.
Retaining Prosthetic Screw
Another aspect that was modified to lessen screw loosening was the design of the retaining prosthetic screw itself. As a screw is tightened with torque it elongates and produces tension between the abutment and implant. Elastic recovery then occurs within the screw, which creates a “clamping force” binding the abutment and the implant.
Preload is defined as the difference between screw elongation and elastic recovery. This determines the “clamping force” which binds the abutment and implant together. Screw loosening occurs when the forces acting on the implant are greater than the “clamping force” or preload of the screw.
Modifications
Several modifications have been made to improve upon the design of Branemark’s original abutment screw. In 2000, Binon noted screw modifications that included the shank, number of threads, diameter, length, thread design, and torque applications of the abutment screw.
Other changes have focused on the material of the screw itself. Haack et al. (1995) suggested that gold screws were superior to titanium. Haack noted that, at manufacturers’ torque recommendations, the mean preload using a gold screw was greater than that of titanium. Reports have shown gold alloy screws to achieve over twice the preloads of titanium alloy screws. A greater preload minimizes screw loosening.
Rotational Misfit and Screw Loosening
Rotational misfit is the misfit between the implant and the abutment. This rotational freedom of the abutment itself on the implant contributes to screw loosening and may lead to micro-movements during loading. In addition, when components do not seat properly, tightening a screw may damage the threads within the implant or on the screw itself. Either way the misfit of the abutment and implant leads to screw loosening.
Studies have shown that a rotational misfit of less than 2 degrees provides a stable screw joint, thus limiting screw loosening. However, the rotational misfit of the external hex connection was originally shown to be between 3 and 10 degrees, providing a further cause of screw loosening.
Modifications
Once taller and wider external hex connections were introduced, the problem of rotational misfit improved. From a manufacturing standpoint, machining a larger hex is much easier and results in enhanced precision of fit and a reduction in rotational misfit.
In addition, other designs were developed to eliminate the degree of rotational misfit. For example, 1.5 degrees of taper among hex flats was introduced, which creates a friction fit between the abutment and implant. Another design involved adding micro-stops in the corners of the abutment hexagon that engages the implant hexagon. Both these designs aimed to limit the misfit, which in turn limits micro-movements and screw loosening.
Internal Connections
External connection modifications have reduced the problem of screw loosening. However, overcoming the esthetic and microbial seal issues warranted a novel approach to the design of the abutment connection. Rather than modify the existing abutment, a new concept was developed – that of the internal connection. This shift revolutionized the market. Now numerous variations of internal connections are available from the different implant manufacturers.
Force Distributions
With an internal connection the weakest link between the implant, abutment connection, screw, and bone is the bone. The force distribution with an internal connection loads deep within the implant wall and distributes out towards the bone. This force distribution shields the forces placed on the screw itself, thus dramatically reducing screw loosening. Levine et al.’s study in 1999 showed screw loosening with conical internal abutment connections to be as low as 3.5%. This was a remarkable improvement from the external connection record, where studies found levels of screw loosening ranging from 6% to 48%.
However, some practitioners do not consider the load transfer feature of the internal connection to be a positive improvement. They argue that if an implant–abutment connection receives excessive forces due to traumatic occlusion or implant malpositioning, screw loosing is easier to deal with than crestal bone loss around the implant.
Rotational Misfit and Screw Loosening
The rotational misfit found in internal connection designs is significantly less than that of the original external hex connection. Some internal connections have essentially eliminated rotational misfit by using a friction-fit design. The precise fit between implant and abutment limits any micro-motion between them, thus limiting screw loosening.
Esthetics
With esthetic zone restorations, the buccal aspect of the prosthesis needs to have enough bulk of ceramic to achieve an ideal color and esthetic outcome. In addition, an esthetically pleasing restoration requires a coronal transition depth from the implant–abutment connection to the gingival margin. This maintains a proper emergence profile and masks the unesthetic metal connection.
External connections are limited in their ability to provide the necessary transition depth or bulk required for esthetic restorations. They may also occasionally appear bulky with an unesthetic emergence profile. Also, external connections may have metal exposed at the finish line level since an expansive abutment cuff height is required to house the external connection of the implant.
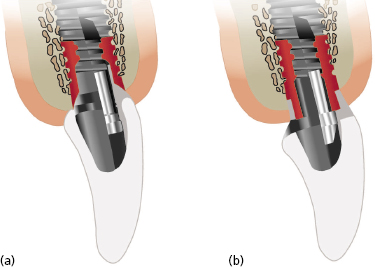
Internal connections (Figure 4.2) are undeniably superior in their ability to provide an esthetic restoration. They permit a sufficient bulk of restoration while at the same time permitting a smooth buccal contour. In addition, the internal connection may provide a better prosthetic emergence profile because technicians can trim the abutment accurately.
Microbial Seal
Any implantologist has experienced a foul odor when an implant abutment is removed. This is due to a leakage of saliva and bacteria into the micro-gap between the implant and abutment, providing a space for micro-organisms to accumulate and thrive. This collection not only creates toxins that cause the unpleasant odor when the abutment is removed, but also increases inflammation at the implant–abutment junction that will eventually cause crestal bone loss.
Internal connections have a greater potential for obtaining a microbial seal between the abutment and implant than do external connections. This microbial seal is achieved due to the precise fit between the abutment and implant, excluding even the smallest microbes. This is a major advantage, although some internal connections fare better than others in this respect.
Many implant companies have capitalized on their superior microbial seal to market their implant systems. For example, Bicon’s study in 2004 verified that their internal morse taper connection provides a hermetic seal that does not permit bacteria to leak from outside-in or from inside-out the abutment connection (Dibart et al. 2005). Mairgünther and Netwig in 1992 showed that the Ankylos abutment connection could provide a vacuum seal for 60 hours.
Most internal connection designs have entered the market with studies promoting their ability to provide a microbial seal.
Superior Joint Strength
Mollersten et al., back in 1997, concluded that deep joints were more likely to resist bending forces than shallow joints. The shallow 0.7 mm external hex connections are simply outdated as deep internal joint connections have greater joint strength. This superior joint strength is particularly important under increased load-bearing areas like the molar regions.
Some practitioners argue that the main reason to use internal connections is because they are esthetically superior in the anterior area. Others maintain that their main attraction is due to their superior joint strength in the posterior area. And some still argue that they prefer internal connections because they are less of a hassle with little screw loosening. Regardless of where implants are placed in the mouth, most clinicians now consider internal connections to be preferable to external connections. It is no surprise that there is such a wide variety of internal connections on the market today for clinicians to choose from.
Platform Switching
Platform switching is a method of preventing crestal bone loss. Although this feature is offered by internal and external connections, the internal connection design uses platform switching more often. To platform switch, the diameter of the abutment is narrower than that of the implant. For example, a 5 mm diameter implant might be used with a 4 mm diameter abutment. Traditionally, the diameter of the implant and the abutment were identical.
The rationale behind platform switching has varied in the literature. Many studies have theorized that an inflammatory infiltrate collects around the implant–abutment junction. By bringing this infiltrate medially, the inflammatory process is confined within the implant platform, thus lessening coronal bony resorption.
Most studies, however, agree on one thing, the effectiveness of platform switching. Atieh’s systematic review and meta-analysis in 2010 also validated this point. Atieh noted that the degree of crestal bone loss was affected by the difference between the diameter of the implant and the abutment. She noted a significant decrease in crestal bone resorption if the implant–abutment diameter difference was greater or equal to 0.4 mm.
Platform switching has been on the market since the introduction of the cone screw or morse taper designs with implants from companies such as Straumann, Ankylos, Bicon, or Astra. These conical designs have always inherently offered the benefits of platform switching.
Comparison of Different Internal Connection Designs
As discussed earlier internal connection have several advantages over external connections, namely less screw loosening, improved esthetics, an advanced microbial seal, a strengthened implant–abutment joint connection, and a variety of options for platform switching. It is clear that practitioners and research, as well as manufacturers, are supporting the internal connection as the superior design. However, the internal connection market has splintered into several different competing designs. Little landmark research has been done to clarify which internal connection is likely to be the best design. The shear fact that the market has not rallied around one single internal connection type leads to the fact that solid research is still lacking.
There are advantages to having different internal implant connections on the market, but the decision between them is arguably more of a style or preference issue than anything else. This text certainly does not seek to endorse one connection design over another. Rather, this section characterizes the major friction-fit joints followed by the slip-fit joints currently available on the market (Table 4.1).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


