CHAPTER 39
Brow Lift
Jon D. Perenack and Earl Peter Park
Department of Oral and Maxillofacial Surgery, Louisiana State University Health Sciences Center, New Orleans, Louisiana, USA
Procedures aimed toward addressing brow ptosis and forehead and glabellar rhytids. Approaches include endoscopic, trichophytic (subgaleal and subcutaneous), and coronal. Although all techniques address brow ptosis, treatment planning is often guided by cosmetic diagnoses, surgeon preference, and supplemental procedures such as bony orbital recontouring, muscle resection, hairline repositioning, and concomitant upper blepharoplasty.
General Indications
- Brow ptosis
- Brow asymmetry
- Deep rhytids and furrows traversing the forehead, glabella, and/or nasal radix
- Appearance of heavy or redundant forehead or temporal skin
- Pseudo-blepharoptosis and/or visual field restriction
General Contraindications
- Lagopthalmos
- Previous or current dry-eye symptoms
- Unrealistic patient expectations
Anatomy
- Supraorbital nerve: Exits the superior orbit parallel to the medial limbus. The nerve forms branches, which innervate the frontoparietal skin (deep branch) and upper eyelid (superficial branch).
- Supratrochlear nerve: Exits the superomedial orbit and is located 9.0 mm (+/− 3 mm) medial to the supraorbital nerve. Innervates the skin of the lower forehead (midline glabella), the medial upper eyelid, and a portion of the conjunctiva.
- Sentinel vein: Located approximately 10 mm lateral to the zygomaticofrontal suture. Serves as a warning for the proximity of the temporal branch of the facial nerve.
- Temporal branch of the facial nerve: As the temporal branch courses superior to the zygomatic arch, it is located within or along the undersurface of the temporoparietal fascia. The temporal branch provides motor innervation to the brow musculature and the superior portion of the orbicularis oculi muscle. The anticipated course of the temporal branch can be approximated by drawing a line from a point 5 mm anterior to the tragus to a point 15 mm lateral to the lateral taper of the ipsilateral brow.
- Conjoint (conjoin) tendon: The fusion of the galea, superficial and deep temporal fascia and periosteum (pericranium) within the anterior temporal region.
Preoperative Markings
- Patients are marked preoperatively while sitting upright.
- The brow lift is simulated with manual manipulation of the brows prior to placing the patient supine, and the desired vectors of pull are marked.
- Important markings include the incision sites, the skin to be resected, and the anticipated location of nerves (supraorbital, supratrochlear, and temporal nerve).
- Standard preoperative photographs are taken and placed in the operatory within the surgeon’s field of view for reference during the procedure.
Endoscopic (Closed) Brow Lift
Indications
- Circumvent the placement of more visible scars associated with open techniques (trichophytic and coronal)
- Patient preference for a less invasive procedure
- Patient with short to normal upper facial third (less than 6 cm from brow to hairline)
Note that the endoscopic brow lift procedure may raise the hairline.
Contraindications
- Excessive hairline recession
- Excessively curved forehead inhibiting the passing of endoscopic instruments to the periorbita
Technique
- Preoperative markings are made with the patient sitting upright (Figure 39.1 [all figures cited in this section appear in Case Report 39.1]).
- Intravenous sedation or oral endotracheal intubation is employed. A single dose of intravenous antibiotics is recommended prior to the start of the procedure.
- The patient is positioned supine (Figure 39.2) with the endoscope monitor within view of the surgeon and surgical assistant, typically at the foot of the operating table.
- Tumescent solution is injected within the anticipated tissue planes to be elevated. Local anesthetic is injected supraperiosteally along the supraorbital and lateral orbital rims. Nerve blocks of the auriculotemporal and zygomaticotemporal nerves is recommended with intravenous sedation.
Five incisions (ports) are placed and hidden posterior to the patient’s hairline: a single vertical 2 cm midline incision (Figure 39.3), two 1.5 cm vertical paramedian (parasagittal) incisions (Figure 39.4) located superior to the proposed highest point of the brow arch (lateral limbus of the eye), and two beveled 2–3 cm horizontal incisions (Figure 39.9) located within the temporal hair-bearing region 1–2 cm lateral to the temporal crest and 2–3 cm posterior to the hairline. The midline and paramedian incisions are made through all layers of the scalp to the cranium, and the temporal incisions are carried to the superficial layer of the deep temporal fascia.
- Blind dissection (without the endoscope) is performed with a curved periosteal elevator to develop a full-thickness subperiosteal flap using the midline and paramedian ports (Figure 39.5). Blindly, a curved endoscopic elevator is utilized to dissect within a subperiosteal tissue plane posteriorly to the coronal suture (vertex of the skull), anteriorly to a point 2 cm cephalic to the supraorbital rims, and laterally along the lateral orbit rims below the lateral canthus approaching the infraorbital rim. Care is taken to fully release the arcus marginalis from the orbital margins (Figure 39.6).
- A 30° endoscope with a protected sheath is inserted through the midline port (Figure 39.7). Endoscopic instruments are inserted through the paramedian ports, and dissection proceeds caudally toward the supraorbital rim, glabella, and lateral orbital rims. The endoscope is used to visualize the central compartment and to allow instrumentation to dissect the remaining central periosteum and to expose the brow (galeal) fat pad. The supraorbital nerves are often visualized (Figure 39.8) through the overlying tissue, and the periosteum is subsequently released around the nerve bundles. Below the brow fat pad, a horizontal release of the periosteum is typically carried out with a scoring instrument. The periosteal release is enlarged until the defect is at least 1 cm. This allows passive mobilization of the forehead and minimizes relapse. Care is taken not to tear the supraorbital neurovascular bundles as they are often denuded at this point.
- With periosteum exposure and scoring completed, resection or ablation of the corrugators and procerus muscles may be carried out if desired. The authors typically recommend scoring with the electrocautery as an alternative to muscle resection to minimize postoperative soft tissue defects and an unnatural brow appearance.
- Laterally, utilizing the temporal ports (Figure 39.9), a curved elevator is used to blindly dissect (Figure 39.10) within a tissue plane created between the temporoparietal fascia (superficial temporal fascia) and the temporalis fascia (deep temporal fascia) overlying the temporalis muscle. The entire superficial temporal space is released anteriorly and posteriorly to allow passive posterior movement of the scalp. Inferiorly, the dissection comes to a “soft” stop approximately 1 cm above the zygomatic arch where the temporoparietal fascia fuses with the temporalis fascia. Aggressive dissection below this point raises significant risk of injuring the facial nerve as it crosses the arch. The sentinel (medial zygomatic temporal) vein is located 1 cm lateral to the zygomaticofrontal suture and should also be avoided.
- The lateral subgaleal and the central subperiosteal dissection planes are connected by dividing the conjoint tendon (Figure 39.11) at the superior temporal line. A sharp dissector is placed through the temporal port and is driven through the conjoint tendon into the frontal pocket slightly above the supraorbital rim. The conjoint tendon is then opened posteriorly with a sweeping motion until there is a complete connection between the two pockets.
Fixation is accomplished at the temporal ports first and then at the paramedian ports. A 0-0 Nurolon (Ethicon US, LLC, Somerville, New Jersey, USA) suture is utilized to grasp the temporoparietal fascia on the medial aspect of the incision (Figure 39.12). The suture is superiorly and posteriorly ligated to the temporalis fascia (Figure 39.13). The vector follows the line formed from the ala to lateral canthus (Figure 39.1). Occasionally, a second suture is required to secure the flap. This suture placement is performed bilaterally to a symmetrical endpoint. (Note: If the corrugators were aggressively released earlier, this step has the risk of excessively widening the interbrow distance.) Fixation is accomplished at the paramedian incisions with the placement of resorbable 3.5 mm Endotine (Microaire Aesthetics, Charlottesville, Virginia, USA) devices. Skin hooks are utilized to retract the paramedian incision laterally. The Endotine drill is used to engage the cranium to the depth of the Endotine drill bit along the anticipated vertical vector (typically, the lateral limbus of the eye) of the brow lift. The osteotomy (Figure 39.14) site is irrigated to remove any residual bone shavings. The Endotine insertion tool is used to secure the Endotine into the predrilled Endotine osteotomy. The Endotine is fully seated when it is flush with the cranium. Endotines are placed bilaterally at each of the two paramedian incisions. The forehead scalp is elevated and positioned onto the Endotine devices. This maneuver sets the height and arch of the brows. Care is taken not to over– or underelevate the brow. If resistance to elevation is noted, additional periosteal release along the lateral supraorbital rims may be required. We recommend leaving the forehead scalp secured to the anchors for at least 10 minutes, and then reassess for any soft tissue creep and resulting laxity. If necessary, the lax scalp is then gently lifted off of the Endotine devices, re-elevated to the proper height with tension, and then resuspended.
- Scalp incisions are closed with either skin staples or sutures, and bacitracin is applied. Drains are usually not necessary. Light pressure dressing may be placed depending on the preference of the surgeon.

Figure 39.1. Preoperative markings are made with the patient in the upright position. The pink lines represent the anticipated vectors of pull.
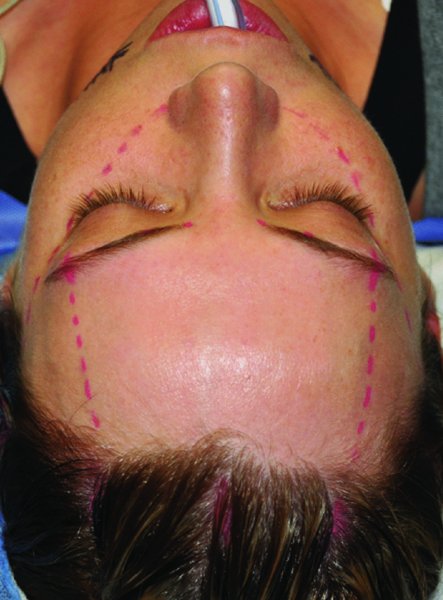
Figure 39.2. The patient is orally intubated, and the anticipated vectors of pull and the sites of the incisions are marked.

Figure 39.3. A vertical midline incision is created posterior to the hairline.

Figure 39.4. Two vertical paramedian incisions are created posterior to the hairline and along the anticipated vector of pull to elevate the apex of the brow.

Figure 39.5. The central flap is blindly elevated within a subperiosteal tissue plane. The supraorbital markings demonstrate the inferior extent of the blind dissection.

Figure 39.6. The arcus marginalis must be freed in order to sufficiently mobilize the tissue flap.

Figure 39.7. A 30° endoscope is inserted through the midline port and allows for dissection of the central flap under visualization.
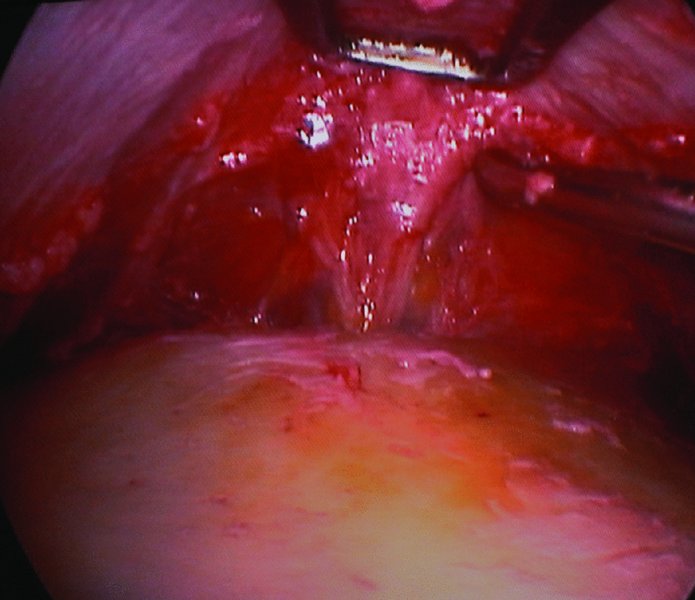
Figure 39.8. The endoscope allows for visualization of/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


