CHAPTER 19
Panfacial and Naso-Orbito-Ethmoid (NOE) Fractures
Celso F. Palmieri, Jr. and Andrew T. Meram
Department of Oral and Maxillofacial Surgery, Louisiana State University Health Sciences Center, Shreveport, Louisiana, USA
Reduction and reconstruction of hard and soft tissue injures of the facial skeleton to allow for early and total restoration of facial form, symmetry, and function.
Indications for Reduction of Panfacial and NOE Fractures
- To establish airway security in the presence of unstable fractures, expanding hematoma, and foreign body aspiration
- Extensive soft tissue injury requiring debridement with primary closure
- Profuse blood loss from facial injuries
- Large, open, contaminated compound wounds
- Concomitant systemic injuries requiring immediate operative intervention by another surgical subspecialty
- Restoration of pre-injury facial aesthetics and function
- Prevention of latent cosmetic and functional deficits
Contraindications
- Patients with severe, compromising, concomitant systemic trauma, rendering them unstable for open reduction with internal fixation (ORIF)
- Unstable patients requiring correction of blood volume, electrolyte, and nutritional deficits
- Significant facial edema in stabilized patients that interferes with the ability to obtain an accurate clinical evaluation, obscures maxillofacial anatomy or surgical landmarks, and makes the surgical procedure itself more difficult
- Increased intracranial pressure (>15 mm Hg) in patients with concomitant head injuries
Anatomy
The facial skeleton receives support and stability from a series of transverse and vertical facial buttresses. Facial buttresses represent areas of thick bone that support the surrounding thinner facial bones, sustain masticatory forces, and protect vital structures. Restoration of facial width, height, and projection is achieved by reducing and reconstructing the facial buttresses.
Transverse (Horizontal) Facial Buttresses
- Superior transverse facial buttress (frontal bar): Orbital plate of the frontal bone and the cribriform plate of the ethmoid
- Middle transverse facial buttress: Temporal bone, zygomatic arch, infraorbital rim and orbital floor, frontal process of the maxilla, and nasal bones. Crosses the zygomaticotemporal, zygomaticomaxillary, and nasofrontal sutures
- Inferior transverse facial buttress: Hard palate and maxillary alveolus
- Superior transverse mandibular buttress: Inferior alveolar ridge of the mandible
- Inferior transverse mandibular buttress: Inferior border of the mandible from angle to angle
Vertical Facial Buttresses
- Central nasoethmoidal buttress: Ethmoid and vomer bones
- Nasomaxillary buttresses: Frontal process of maxilla, nasal bones, nasion and medial walls of maxillary sinuses, and orbits
- Zygomaticomaxillary buttress: Posterior maxillary molars vertically through zygomaticomaxillary sutures, zygomatic bodies, and lateral orbital walls into the frontal bones
- Pterygomaxillary buttresses: Pterygoid processes of sphenoid bone and posterolateral and posteromedial walls of maxillary sinuses
- Posterior mandibular buttress: Ascending ramus and condyle
Figure 19.1 shows horizontal and vertical facial buttresses.
- Naso-orbital-ethmoidal (NOE) complex: often divided into two components: the interorbital space and the medial orbital wall
- Interorbital space: two ethmoidal labyrinths, superior and middle turbinates, and perpendicular plate of ethmoid
- Medial orbital wall: anteriorly—lacrimal bone, lacrimal apparatus, and lamina papyracea; posteriorly—body of sphenoid and medial canthal tendon
- Signs of NOE fractures include a lack of skeletal support on palpation of the nose, a wide and depressed nasal radix (flat nose), an upturned nasal tip, lacrimal dysfunction, a swollen medial canthal area, traumatic telecanthus, a shortened palpebral fissure, enophthalmos, ocular dystopia, cerebrospinal fluid (CSF) rhinorrhea, and a positive eyelid traction test.
- Medial canthal tendon (MCT): The MCT is formed from fibrous bands that originate from the tarsal plates of the upper and lower lids and insert at the frontal process of the maxilla (anterior limb) and at the posterior and superior aspect of the lacrimal bone (posterior limb). The segment of bone that the MCT attaches to is often called the central fragment.
- Markowitz NOE Classification System: Based on the fracture patterns of the central fragment and associated MCT attachment
- Markowitz Type I: A large central fragment of bone without avulsion of the MCT
- Markowitz Type II: Comminution of the central fragment without avulsion of the MCT
- Markowitz Type III: Comminution of the central fragment with avulsion of the MCT
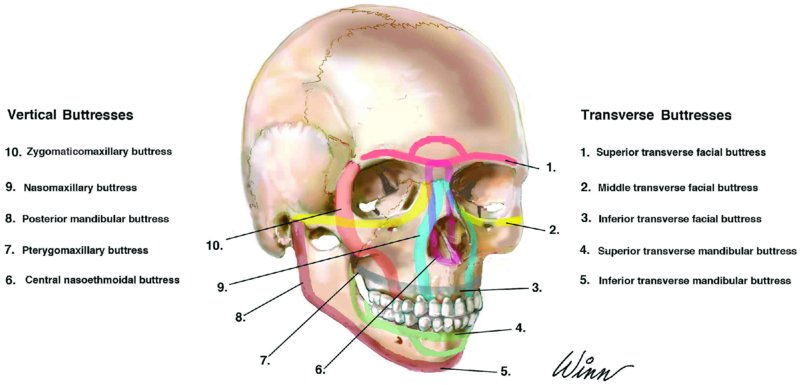
Figure 19.1. Transverse and vertical buttresses of the facial skeleton.
Panfacial fracture and NOE reduction technique
- The patient is positioned supine on the operating room table, the cervical spine (if involved) is stabilized and the airway are secured.
- Corneal shields are lined with LacriLube ointment and placed over the corneas.
- The patient’s posterior oropharynx is suctioned, and a moistened Ray-Tec gauze is placed within the posterior oropharynx to serve as a throatpack.
- The patient’s oral cavity is cleaned with Chlorhexidine Gluconate 0.12% mouth rinse and a toothbrush. Care is taken to scrub the existing dentition, gingiva, and tongue thoroughly.
- The patient is prepped and draped to allow for visualization of all involved structures and normal adjacent anatomy.
- All planned incision sites are marked and subsequently injected with local anesthesia containing a vasoconstrictor.
- Avulsive and contaminated soft tissue injuries are irrigated and debrided to remove all foreign bodies and debris, often with pulsatile lavage. Soft tissue injuries are assessed for use as possible areas of surgical access.
- Maxillary and mandibular arch bars are placed in order to reestablish the patient’s pre-trauma occlusion and to serve as a stable base for the repair of mandibular and facial bone fractures.
-
If mandibular fractures are present, attention is first turned toward the reduction of the mandibular fractures based on the patient’s occlusion and known anatomical landmarks. Mandibular fractures are exposed using the standard intraoral or extraoral incisions, reduced, and internally fixated (Figure 19.5, Case Report 19.1). In cases with bilateral subcondylar fractures, at least one condyle is opened, reduced, and rigidly fixated in order to establish proper vertical height (Figure 19.4, Case Report 19.1).
- Once the mandible is repaired, attention is directed toward midface fractures.
- All remaining facial fractures are exposed through a combination of approaches. Existing lacerations can be utilized as well. Specific techniques are discussed in detail in preceding chapters.
- NOE fractures are reduced and fixated by reconstructing the nasomaxillary vertical facial buttresses and the superior and middle transverse facial buttresses. Often, calvarian and columellar strut grafting and concomitant medial canthal tendon (MCT) resuspension is required.
- Markowitz type I and mild type II fractures are repaired with repositioning of the central segment with bone plates. Markowitz III and grossly comminuted type II fractures are repaired with a combination of bone plates and transnasal wiring in order to reposition the displaced or avulsed MCT.
- The avulsed MCT or small bone segment containing the MCT (central fragment) is identified. For unilateral Markowitz type II/III fractures, a 28– or 30–gauge wire (with or without a barb) is used to pass twice through the MCT or central fragment. The wire is passed through the nasal cavity posterior and superior to the lacrimal bone with either a bone awl or a spinal needle. A small fixation plate (anchor plate) is secured to the contralateral side within solid bone along the medial orbital wall or reconstructed nasal bridge. The wire is secured to the anchor plate to restore the intercanthal distance. For bilateral Markowitz type II/III fractures, transnasal wiring of the bilateral MCT or central fragment is performed and secured to the anchor plate to correct the intercanthal distance. In either situation, a slight overcorrection is performed.
- After reduction and fixation of all facial fractures, maxillomandibular fixation (MMF) is released, and the occlusion is checked to ensure adequate stability. If the occlusion is non-ideal, the patient is placed back into MMF, the facial fractures are reevaluated, and adjustments are made.
- All incisions are irrigated with copious normal saline and closed. Large, avulsive tissue injuries may require debridement and closure with either local or regional flap elevation.
- At the completion of the procedure, the patient’s oropharynx is suctioned, and the throat pack is removed and MMF is typically reapplied with either elastics or stainless steel wires.
- The corneal shields are removed, and the eyes are flushed with balanced salt solution. All blood and prep are removed from the patient’s skin with a wet and a dry lap.
- Steri-strips and pressure dressings are applied. If indicated, a rigid c-collar is placed.



