Conscious Sedation
Rationale for Sedation During Periodontal and Implant Surgical Procedures
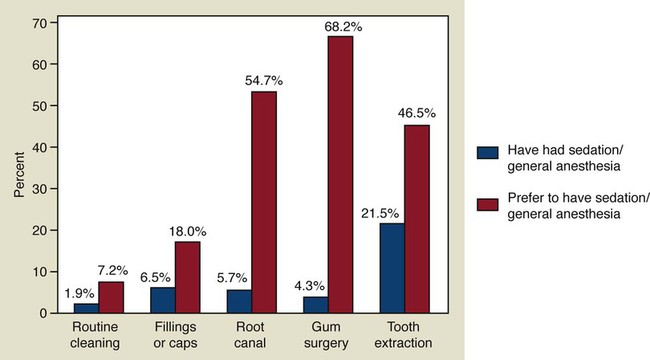
Many patients delay or avoid having needed dental treatment because of fear and anxiety. This avoidance behavior often results in compromised health and quality of life. Anxiety toward dental therapy has not changed significantly over the past 50 years; publications report that about 30% to 50% of patients are at least somewhat fearful of dental procedures.1–4 New evidence suggests that genetic variations are associated with anxiety related to dental care, which could help to explain the consistent avoidance patterns despite improved treatment methods.5 According to a national survey of the Canadian population, more than 68% of patients would prefer to have sedation or general anesthesia for periodontal surgery6 (Figure 36-1). Anxiety reduction is an important part of delivering advanced periodontal services.7 Furthermore, since dental anxiety results in avoidance behavior and is associated with more dental and periodontal problems,8,9 it is likely that a disproportionate number of patients referred to periodontal specialists will have dental anxiety. Interestingly, there appears to be a close relationship between anxiety and postoperative pain. In fact, preoperative anxiety may be considered a predictor of postoperative pain.10,11 In addition, high levels of anxiety (stress) can affect wound healing after periodontal treatment12–14 (see Chapter 11). Sedation techniques have been shown to be effective in reducing physiologic markers of stress.15 For these reasons, it is important for clinicians who provide advanced periodontal and implant therapy to be knowledgeable and skilled in providing sedation in order to reduce anxiety in their patients.
ADA Policy Statement and Guidelines for Conscious Sedation
In 2007, the American Dental Association (ADA) released three documents related to the use of sedation and general anesthesia in dentistry, including (1) the ADA Policy Statement: The Use of Sedation and General Anesthesia by Dentists,16 (2) the ADA Guidelines for the Use of Sedation and General Anesthesia by Dentists,17 and (3) ADA Guidelines for Teaching Pain Control and Sedation to Dentists and Dental Students.18 The ADA Policy Statement and the ADA Guidelines provide educational and practice standards for anxiety control in dental practice. The ADA Committee on Anesthesiology, consisting of representatives from dental organizations involved with sedation and anesthesia (Table 36-1), produced these documents after review of the relevant scientific evidence, expert opinion, and comment by all communities of interest. The following paragraphs describe the important elements of these documents as they relate to treating anxious periodontal patients.
TABLE 36-1
American Dental Association Committee on Anesthesiology: 2007 Policy and Guidelines
| Dr. Guy Shampaine, Chairperson | Dr. David Moyer |
| American Dental Association Oral and Maxillofacial Surgeon |
American Association of Oral and Maxillofacial Surgeons |
| Annapolis, MD | Oral and Maxillofacial Surgeon |
| Dr. Michael Edwards | South Portland, ME |
| American Dental Association | Dr. Mort Rosenberg |
| General Dentist Wedowee, AL |
American Dental Society of Anesthesia |
| Dr. Dee Isackson American Society of Anesthesiologists |
Dental Anesthesiologist, Tufts University School of Dental Medicine |
| M.D. Anesthesiologist | Boston, MA |
| Bothell, WA | Dr. David Rothman |
| Dr. Michael Mashni American Association of Dental Anesthesiologists |
American Association of Pediatric Dentists Pediatric Dentist |
| Dental Anesthesiologist | San Francisco, CA |
| Fullerton, CA | |
| Dr. Robert Merin | |
| American Academy of Periodontology | |
| Periodontist | |
| Woodland Hills, CA |
ADA Policy Statement: The Use of Sedation and General Anesthesia by Dentists
The dental profession’s continued ability to control anxiety and pain effectively depends on a strong educational foundation in the discipline. Training to competency in minimal and moderate sedation techniques may be acquired at the predoctoral, postgraduate, graduate, or continuing education level. Dentists who wish to utilize minimal or moderate sedation are expected to successfully complete formal training, which is structured in accordance with the ADA Guidelines for Teaching Pain Control and Sedation for Dentists and Dental Students.18 The knowledge and skills required for administration of deep sedation and general anesthesia are beyond the scope of predoctoral and continuing education. Only dentists who have completed an advanced education program accredited by the Commission on Dental Accreditation (CODA) that provides training in deep sedation and general anesthesia are considered educationally qualified to use these modalities in practice.
ADA Guidelines for the Use of Sedation and General Anesthesia by Dentists
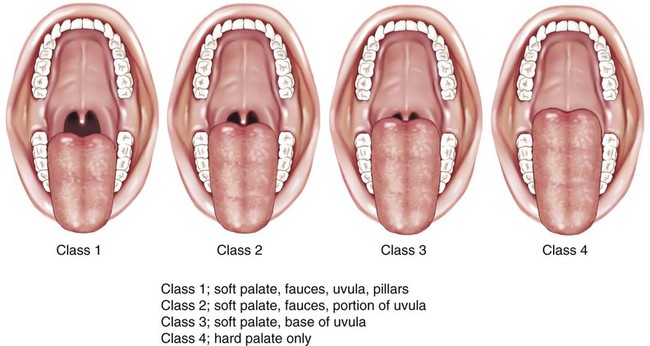
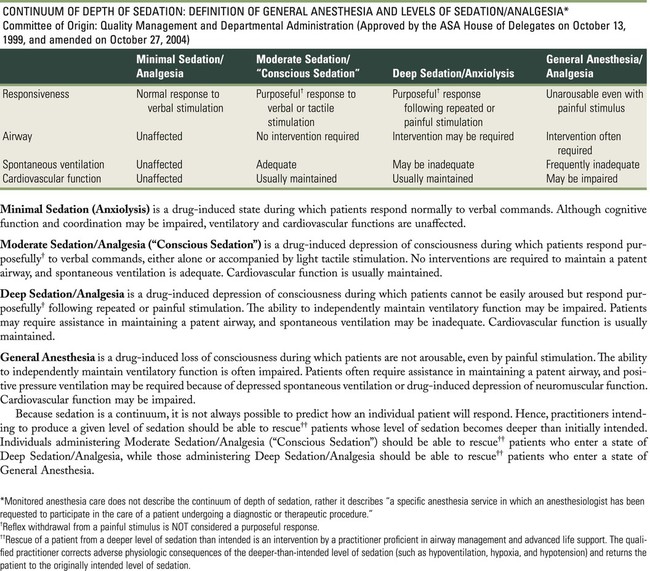
Unlike previous ADA documents, the 2007 ADA Guidelines refer to the effects of sedation on the central nervous system and are not dependent on the route of administration. The ADA adopted the American Society of Anesthesiologists (ASA) definitions for levels of sedation (Figure 36-2) and expanded and commented on them specifically as they relate to treating dental patients.19
Definitions and Levels of Sedation
Pediatric Sedation
Children (aged 12 and younger) can become moderately sedated despite an intended level of minimal sedation. The use of preoperative sedatives for children (ages 12 and younger) except in extraordinary situations must be avoided because of the risk of unobserved respiratory obstruction during transport by untrained individuals. The management of children with conscious sedation is beyond the scope of this chapter and is not covered. For children 12 years of age and younger, the reader is referred to the American Academy of Pediatrics/American Academy of Pediatric Dentists Guidelines for Monitoring and Management of Pediatric Patients During and After Sedation for Diagnostic and Therapeutic Procedures.20
Clinical Guidelines for Minimal and Moderate Sedation
The following clinical guidelines apply to both minimal and moderate sedation.17 These guidelines include (1) patient evaluation, (2) preoperative preparation, (3) personnel and equipment, (4) monitoring and documentation, and (5) recovery and discharge. Differences between guidelines for minimal and moderate sedation are indicated as appropriate.
Patient Evaluation.
Patients must be evaluated to assess their current health status before any sedation procedure. This should include a determination of their ASA physical status (ASA PS) (Table 36-2). In healthy or medically stable individuals (ASA PS 1 or 2), a review of their medical history and medication use may be adequate. However, for patients with significant medical considerations (ASA PS 3 or 4), a consultation with their primary care physician or consulting medical specialist is indicated. The evaluation should also include baseline vital signs and a focused physical examination of alertness, respiratory function, airway, and appearance, as well as a specific evaluation of any identified medical conditions (Box 36-1 and Figure 36-3).
TABLE 36-2
ASA Physical Status Classification System
| ASA 1 | A normal healthy patient |
| ASA 2 | A patient with mild systemic disease |
| ASA 3 | A patient with severe systemic disease |
| ASA 4 | A patient with severe systemic disease that is a constant threat to life |
| ASA 5 | A moribund patient who is not expected to survive without the operation |
| ASA 6 | A declared brain-dead patient whose organs are being removed for donor purposes |
From American Society of Anesthesiologists: ASA physical status classification system: www.asahq.org, 2009.
Preoperative Preparation.
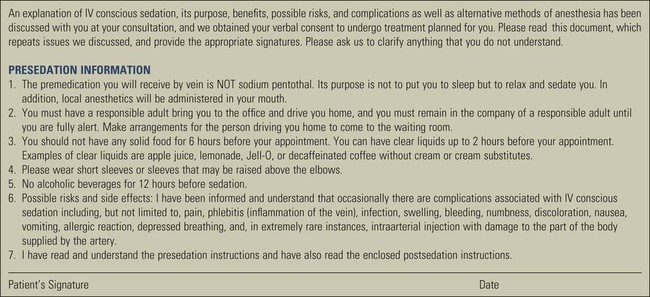
The patient (parent, guardian, or caregiver, if patient is a minor) must be informed about the planned procedure under sedation, including benefits, risks, and instructions for sedation (Figure 36-4). An informed consent for the proposed procedure and sedation must be obtained.
Preoperative dietary restrictions must be considered based on the sedative technique prescribed (Boxes 36-2 and 36-3; see also Figure 36-4).
Personnel and Equipment.
For moderate sedation, the equipment necessary to establish IV access must be available. This includes a catheter or butterfly needle, an IV drip line, a solution bag (saline or dextrose), tourniquet, and appropriate antiseptic/dermal disinfectant (Figure 36-5).

Monitoring.
The dentist or an appropriately trained individual, directed by the dentist, must remain in the operatory during active dental treatment with sedation to monitor the patient continuously until the criteria for discharge is met (Box 36-4). The appropriately trained individual must be familiar with monitoring techniques and equipment.
In the case of moderate sedation, a qualified dentist administering moderate sedation must remain in the operatory room to monitor the patient continuously until the patient meets the criteria for recovery. When active treatment concludes and the patient recovers to a minimally sedated level, a qualified auxiliary may be directed by the dentist to remain with the patient and continue to monitor him or her as explained in the guidelines until discharged from the facility. The dentist must not leave the facility until the patient meets the criteria for discharge and is discharged to go home with a responsible adult (see Box 36-4).
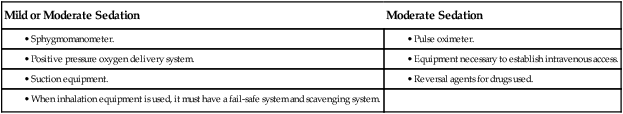
Monitoring equipment must include a sphygmomanometer, positive pressure oxygen delivery system, suction, and if inhalation sedation is used, a fail-safe and scavenging system. In the case of moderate sedation, a pulse oximeter, equipment for IV access, and reversal agents for drugs used must also be available (Table 36-3).
TABLE 36-3
Equipment Required for Mild or Moderate Sedation
| Mild or Moderate Sedation | Moderate Sedation |
In the case of moderate sedation, the level of consciousness (e.g., responsiveness to verbal command) must be continually assessed (Table 36-4).
TABLE 36-4
The Observer’s Assessment of Alertness/Sedation Scale
| Category | Observation | Score |
| Responsiveness | Responds readily to name spoken in normal tone | 5 |
| Lethargic response to name spoken in normal tone | 4 | |
| Responds only after name is called loudly and/or repeatedly | 3 | |
| Responds only after mild prodding or shaking | 2 | |
| Does not respond to mild prodding or shaking | 1 | |
| Speech | Normal | 5 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses