35
Aggressive periodontitis
Figure 35.1 For Aggregatibacter actinomycetemcomitans (A.a.) to initiate periodontal destruction, it needs to undergo the following stages. (1) Attach to buccal cells, move to the tooth surface and progress from a supragingival to subgingival location. Adhesins and autotransporter proteins like Aae and EmaA have a role in attachment to epithelial cells and collagen; fimbriae are involved in autoaggregation, attachment and biofilm formation; and PGA (poly-N-acetyl-glucosamine) polysaccharide may be involved in autoaggregation and is resistant to phagocytosis and antimicrobial peptides. (2) Multiply. Bacteriocins inhibit beneficial species, thereby allowing pathogens to multiply. (3) Evade host defences. A.a.’s leukotoxin is a powerful virulence factor that destroys neutrophils and macrophages; A.a. also produces factors that inhibit neutrophil chemotaxis and are immunosuppressive to immunoglobulin G (IgG) and IgM. (4) Penetrate (invade) tissues (only a few bacteria have this property) – possibly via cytolethal distending toxins and ApiA (an outer membrane protein produced by A.a.). (5) Destroy tissue. A.a. activates T-helper cells and B-cells to incite bone loss and produces collagenases that degrade collagen and periodontal ligament; lipopolysaccharide (endotoxin) activates the host to secrete mediators that lead to bone resorption.
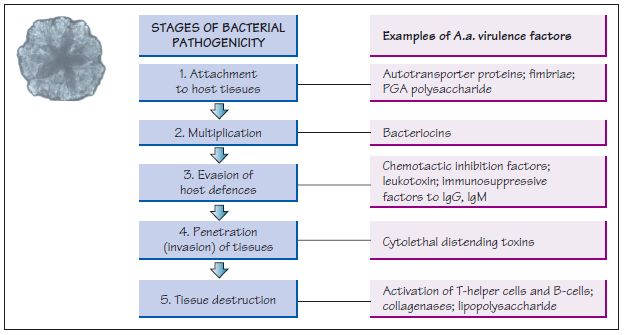
Figure 35.2 A black African girl, aged 12 years, with localised aggressive periodontitis. (a, b) Right and left clinical views. (c) Labial and (d) lingual of the lower incisors showing some plaque, supragingival calculus, subgingival calculus and inflammation. (e) Panoramic radiograph of the patient aged 11 years, when still in the mixed dentition stage, and (f) aged 12 years. The radiographs show characteristic bone loss around the first molars (bilaterally symmetrical, arc-shaped defects with furcation involvement) and angular bone loss around the incisors. Although oral hygiene was unsatisfactory, the levels of plaque are inconsistent with the severe amount of bone loss found in this child.

Figure 35.3 A female (non-smoker) patient aged 32 years with features of localised aggressive periodontitis, with an unknown age of actual onset: (a–d) anterior, right, left and upper arch clinical views, respectively. The periapical radiographs show severe bone loss: (e) UR7 and UR6; (f, g) upper incisors; (h) UL6; (i) LL6 and LL7; and (j) LR6. The patient presented with very deep pockets, clinical attachment loss and visible gingival inflammation especially on UR7, UR6, LR6, LL6 and LL7. Recession was noted on UR1, UL1, UR6 and UL6.
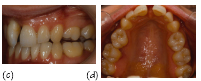
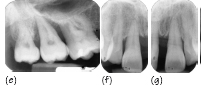
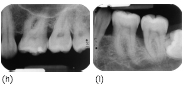

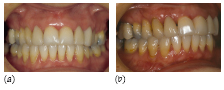
Figure 35.4 A female (non-smoker) patient aged 35 years with generalised aggressive periodontitis: (a–c) anterior, right and left clinical views in occlusion, respectively. (d) A panoramic radiograph showing generalised advanced alveolar bone loss. Generalised mild gingival inflammation is visible, but a relatively small amount of plaque is present which is inconsistent with the severity of destruction, deep pocketing and clinical attachment loss present.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


