Substance dependence
Dependence or addiction is characterized by impaired control over drug use, compulsive use, continued use despite harm, and/or craving. Substance or chemical dependence or abuse (misuse) covers a range of mind-altering substances and is present when at least three of the conditions listed in Box 34.1 apply. Most addictive substances directly or indirectly stimulate the brain’s reward centre by increasing release of dopamine – the neurotransmitter involved in the regulation of emotion, cognition, movement, motivation and pleasure. Brain stimulation with dopamine produces intense euphoria, a pleasurable sensation reinforced by continued drug use.
Drug abuse causes central nervous system (CNS) effects that produce changes in the mind, behaviour, thoughts and mood, levels of awareness or perceptions and sensations. It is defined as self-administration without any medical indication and despite adverse medical and social consequences, in a manner that deviates from the cultural norm and is harmful. Social, mental and physical sequelae are common and discussed below.
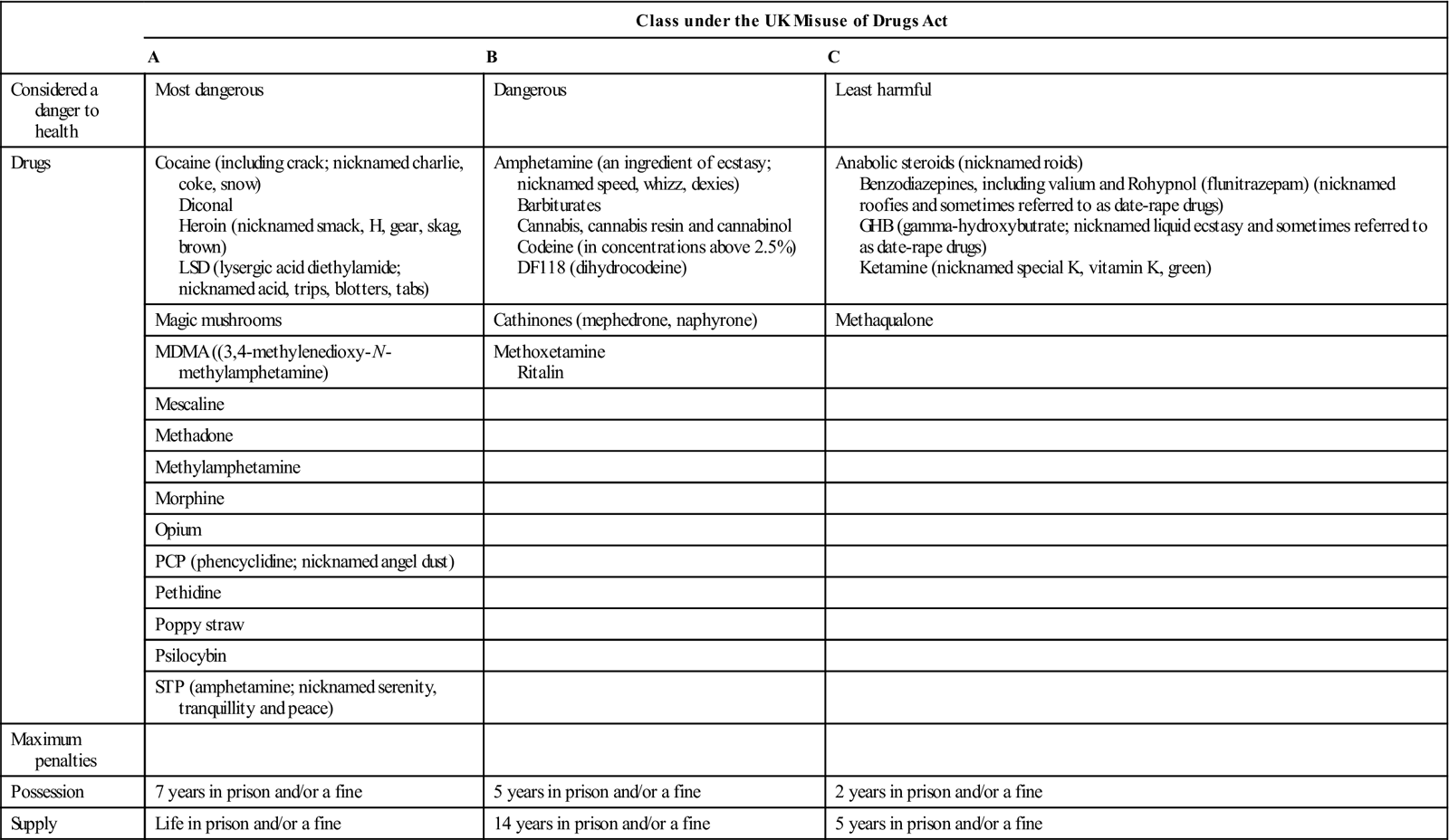
Use of some of these drugs is illegal, and being found in possession of them can lead to criminal charges, particularly, if there is any intention of dealing (supplying; Table 34.1). In the UK, illegal drugs are classified under the Misuse of Drugs Act 1971 as A, B and C, depending on how dangerous they are to health; this classification can only be changed and added to by the Home Secretary. In some countries, use or possession may result in more serious punishments – even execution.
Table 34.1
Main drug classes and penalties for possession and supply
< ?comst?>
| Class under the UK Misuse of Drugs Act | |||
| A | B | C | |
| Considered a danger to health | Most dangerous | Dangerous | Least harmful |
| Drugs | Cocaine (including crack; nicknamed charlie, coke, snow) Diconal Heroin (nicknamed smack, H, gear, skag, brown) LSD (lysergic acid diethylamide; nicknamed acid, trips, blotters, tabs) |
Amphetamine (an ingredient of ecstasy; nicknamed speed, whizz, dexies) Barbiturates Cannabis, cannabis resin and cannabinol Codeine (in concentrations above 2.5%) DF118 (dihydrocodeine) |
Anabolic steroids (nicknamed roids) Benzodiazepines, including valium and Rohypnol (flunitrazepam) (nicknamed roofies and sometimes referred to as date-rape drugs) GHB (gamma-hydroxybutrate; nicknamed liquid ecstasy and sometimes referred to as date-rape drugs) Ketamine (nicknamed special K, vitamin K, green) |
| Magic mushrooms | Cathinones (mephedrone, naphyrone) | Methaqualone | |
| MDMA ((3,4-methylenedioxy-N-methylamphetamine) | Methoxetamine Ritalin |
||
| Mescaline | |||
| Methadone | |||
| Methylamphetamine | |||
| Morphine | |||
| Opium | |||
| PCP (phencyclidine; nicknamed angel dust) | |||
| Pethidine | |||
| Poppy straw | |||
| Psilocybin | |||
| STP (amphetamine; nicknamed serenity, tranquillity and peace) | |||
| Maximum penalties | |||
| Possession | 7 years in prison and/or a fine | 5 years in prison and/or a fine | 2 years in prison and/or a fine |
| Supply | Life in prison and/or a fine | 14 years in prison and/or a fine | 5 years in prison and/or a fine |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Risk Factors for Drug Abuse
Addiction is a primary, chronic, neurobiological condition, influenced by genetic, psychosocial and environmental factors. Men are twice as likely as women to experience drug problems. Factors that may contribute to drug use include:
Persons Who Use Drugs (PWUD)
Substance abuse is increasingly common in many parts of the world. The pattern of drug use in the British Crime Survey by 2012 is shown in Box 34.2.
The 2012/13 Crime Survey for England and Wales showed that in the past year:
■ Cannabis was the most commonly used drug
■ The next most commonly used were powder cocaine and ecstasy.
■ Young adults (aged 16 to 24) were more likely to use drugs.
In the USA, the highest rates of illicit drug use are: in males – in entertainment, food preparation and service, cleaning services and construction; and in females – in food preparation and service, social work and legal professions, including lawyers and legal assistants. Abuse of alcohol is highest among construction workers, car mechanics, food preparation workers, light truck drivers and labourers. Unmarried workers or those having three or more jobs in the previous 5 years report about twice the rate of illicit drug and heavy alcohol use as married workers or those who had two or fewer jobs.
The lowest rates of illicit drug use are in workers in occupations that require public trust, such as health-care professions (HCPs), police officers, teachers and child-care workers. Between 10 and 15% of HCPs misuse drugs or alcohol at some time during their life – rates similar to those seen in the general population. Alcohol abuse is relatively common among doctors and dentists, and one study of USA medical personnel found that over half had tried marijuana or cocaine recreationally, or opioids or tranquillizers for self-treatment. HCPs have higher rates of abuse with benzodiazepines and opiates, and abuse drugs for performance enhancement and as self-treatment for various reasons, such as pain, anxiety or depression. Those in anaesthesia, emergency medicine and psychiatry have the highest rates of drug abuse.
Drugs and alcohol used by medical and dental students are mostly for ‘recreational’ purposes. More than a half of UK dental students in 2003 had used cannabis and over one-third admitted other illicit drug use. Some 6–10% of dentists may abuse drugs, but there is limited evidence to suggest that they are at a greater risk for abusing alcohol or other drugs than the public. Alcohol and tobacco are the substances abused most frequently by dentists, followed by opiates (mainly hydrocodone and oxycodone) and nitrous oxide. Other substances abused include marijuana; opiates (e.g. morphine, fentanyl, pethidine (meperidine), hydromorphone and oxycodone); minor opiates (e.g. hydrocodone and codeine); and anxiolytics (e.g. alprazolam and diazepam). Interpersonal and life circumstances that contribute to dentists misusing drugs and alcohol include career choice dissatisfaction, domestic breakdown, low professional or self-esteem, obsessive–compulsive and perfectionist behaviour, interpersonal relationship difficulties, and stress at work.
Dentists who become aware and are sure of a colleague’s chemical dependency have professional and ethical responsibilities to intervene in a constructive manner. All dentists have an ethical obligation to urge chemically impaired colleagues to seek treatment. Interventions involve discussing the issue with the addicted dentist, offering help if possible, and reporting the dentist to a wellness committee. Once a person with an addiction accepts the presence of the issue and expresses a desire to change, treatment can begin, but it should be individually designed by professionals experienced in treating drug and alcohol abuse. Clinicians in the UK who have such issues can receive support from the Practitioner Health Programme, initiated by the National Clinical Assessment Service (NCAS; http://www.php.nhs.uk/, accessed 30 September 2013).
Recognizing and Detecting Substance Abuse
Behavioural traits that should increase the level of concern include loss of reliability, mood changes, impaired driving, and the self-prescribing of mood-altering medications. Care should be taken with any patient who has subjective symptoms with no objective evidence of the disorder; makes a self-diagnosis and requests a specific drug, especially a psychoactive agent; appears to have a dramatic but unexpected complaint, such as trigeminal neuralgia, requiring potent analgesics; firmly rejects treatments that exclude psychoactive drugs; and has no interest in the diagnosis or investigations, or refuses a second opinion.
To help a friend/colleague address such problems, it is important to document the dates and times when people have expressed concern and when the signs of substance abuse were noted. These may include the smell of alcohol, tremor, slurred speech, ataxic gait and sloppy appearance. It is important to monitor and document incidents so that this information will be available when discussing concerns with a friend or colleague. The user’s first response is typically denial – and a person in denial will often try to convince others that their assessments are wrong or misguided. Recognition of abuse in an HCP may include, in addition to the above, patient and staff complaints about deteriorating attitude and behaviour, worsening personal and professional isolation, excessive amounts of time spent near a drug supply, heavy ‘wastage’ of drugs, sloppy record-keeping, suspect ledger entries and drug shortages, inappropriate prescriptions, or insistence on the personal administration of injected narcotics to patients.
Medical and Social Complications of Drug Abuse
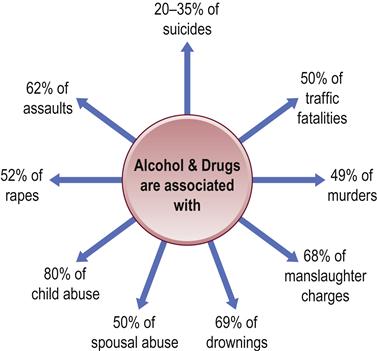
There may be intense drug dependence (or psychological addiction; Table 34.2) and physical effects (physical addiction) in people who use drugs (PWUD) or if a drug of abuse is stopped (withdrawal syndrome) (Fig. 34.1).
Table 34.2
| Drug | Psychological dependence | Physical dependence |
| Heroin | ++++++ | ++++++ |
| Cocaine | +++++ | +++ |
| Alcohol | ++++ | +++ |
| Tobacco | +++++ | ++++ |
| Barbiturates | ++++ | ++++ |
| Benzodiazepines | ++++ | ++++ |
| Amphetamine | +++ | ++ |
| LSD | ++ | + |
| Cannabis | +++ | + |
| Ecstasy | ++ | + |
aAdapted from: Nutt D, et al. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet 2007; 369 (9566): 1047.
Use of illicit drugs is associated with increased rates of infections (e.g. tuberculosis and sexually shared infections [SSIs]), and health and social issues related to alcohol, tobacco and other drugs. Injection drug use is an important route of transmission of blood-borne infections, particularly HIV and viral hepatitis B and C.
Drugs bought on the street are especially hazardous, as they are not necessarily pure and are frequently adulterated or falsely labelled, often with unknown ingredients that may be dangerous in their own right. For example, PWUD who think they are purchasing a drug such as MDMA (ecstasy; 3,4-methylenedioxy-N-methylamphetamine) may be in danger of receiving synthetic cathinones instead; mephedrone has been found as a substitute for MDMA in pills sold as ecstasy in some countries. Intravenous use and the mixing of drugs (polydrug use) are particularly hazardous; those who misuse drugs not uncommonly misuse several substances, including alcohol and tobacco, and may well neglect their health – general and oral. Heroin and cocaine are especially dangerous. Tobacco and alcohol also cause significant harm, but cannabis appears to be less harmful in general.
Almost every month, new synthetic drugs, opiate painkillers and other substances emerge as popular among partygoers and drug addicts. Recently appearing new drugs include:
See also “LEGAL HIGHS” and “EMERGING DRUGS”.
Clinical Features
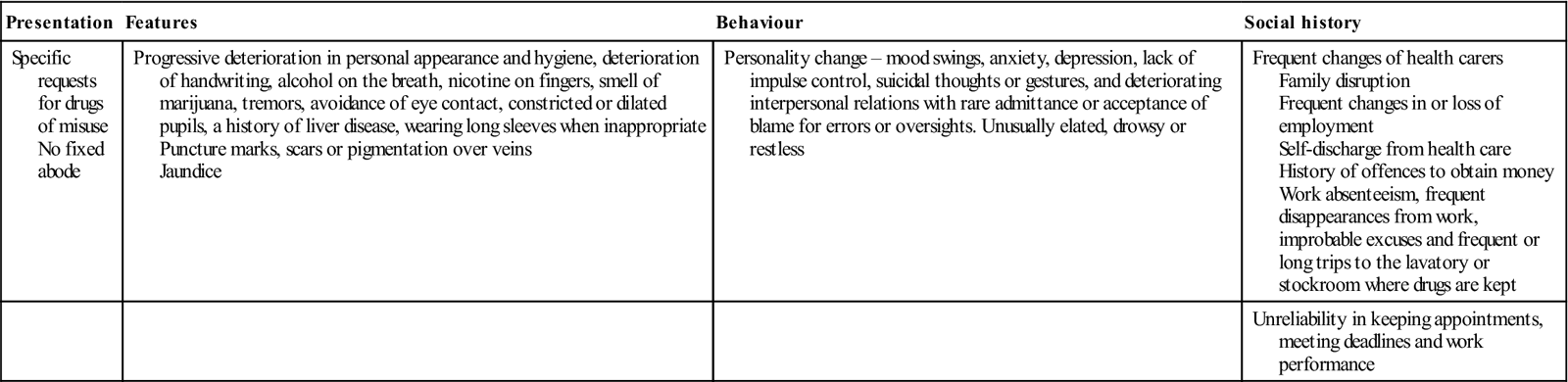
Signs and symptoms that may indicate drug addiction include behavioural and social features, as well as health aspects (Table 34.3). There can be serious medical and behavioural consequences affecting both user (and any fetus) and others in the community, not least because of assaults, theft and prostitution used to fund the drug habit. Maxillofacial injuries and sexually shared and other infectious diseases are thus common consequences. Intravenous injection is common in drug misuse, often with filthy injection technique, sharing of needles or syringes (with the risk of blood-borne infections) and even use of water from a lavatory pan to dissolve the drug. Viral hepatitis (particularly B, C, D and others), chronic liver disease, human immunodeficiency virus (HIV) and other blood-borne agents are common consequences of intravenous drug abuse or drug ‘snorting’. Infective endocarditis and consequent cardiac lesions may stem from infected injections. Venous thromboses are common, making intravenous injection difficult.
Table 34.3
Features possibly suggesting drug misuse (recognition of persons who use drugs)
< ?comst?>
| Presentation | Features | Behaviour | Social history |
| Specific requests for drugs of misuse No fixed abode |
Progressive deterioration in personal appearance and hygiene, deterioration of handwriting, alcohol on the breath, nicotine on fingers, smell of marijuana, tremors, avoidance of eye contact, constricted or dilated pupils, a history of liver disease, wearing long sleeves when inappropriate Puncture marks, scars or pigmentation over veins Jaundice |
Personality change – mood swings, anxiety, depression, lack of impulse control, suicidal thoughts or gestures, and deteriorating interpersonal relations with rare admittance or acceptance of blame for errors or oversights. Unusually elated, drowsy or restless | Frequent changes of health carers Family disruption Frequent changes in or loss of employment Self-discharge from health care History of offences to obtain money Work absenteeism, frequent disappearances from work, improbable excuses and frequent or long trips to the lavatory or stockroom where drugs are kept |
| Unreliability in keeping appointments, meeting deadlines and work performance |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
General Management
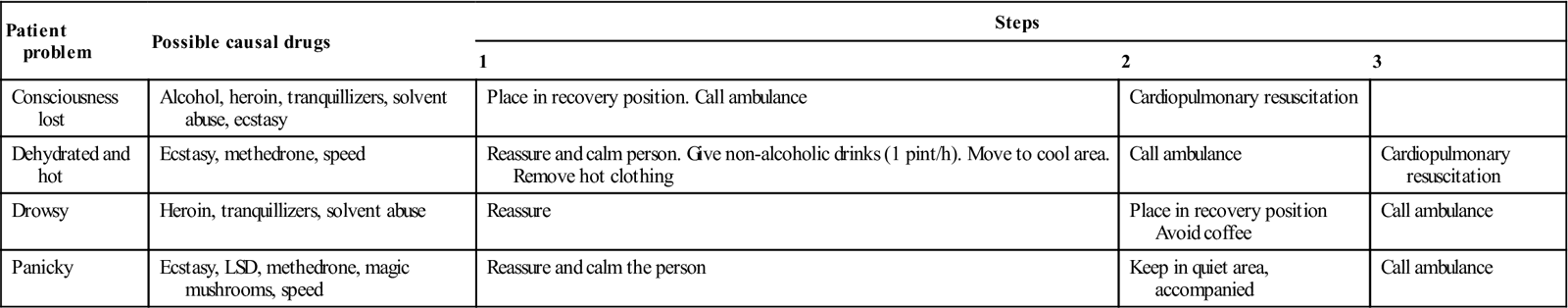
Common management difficulties are behavioural problems, including irregular health care, poor attendance and compliance, effects of trauma and the frequent risk of maxillofacial and other injuries during assaults or fights, and hazards of cross-infection with hepatitis viruses, HIV and, increasingly, tuberculosis. PWUDs who collapse or become hyperthermic, drowsy or panicky may well need emergency care (Table 34.4). Many drugs of abuse can alter behaviour or interact with drugs used for medical or dental purposes (Ch. 29). There can therefore be substantial difficulties in interactions between HCPs and drug users. However, it is unethical to withhold treatment from any patient on the basis of a moral judgment that the patient’s activities or lifestyle might have contributed to the condition for which treatment was being sought.
Table 34.4
Emergency care of people who use drugs
< ?comst?>
| Patient problem | Possible causal drugs | Steps | ||
| 1 | 2 | 3 | ||
| Consciousness lost | Alcohol, heroin, tranquillizers, solvent abuse, ecstasy | Place in recovery position. Call ambulance | Cardiopulmonary resuscitation | |
| Dehydrated and hot | Ecstasy, methedrone, speed | Reassure and calm person. Give non-alcoholic drinks (1 pint/h). Move to cool area. Remove hot clothing | Call ambulance | Cardiopulmonary resuscitation |
| Drowsy | Heroin, tranquillizers, solvent abuse | Reassure | Place in recovery position Avoid coffee | Call ambulance |
| Panicky | Ecstasy, LSD, methedrone, magic mushrooms, speed | Reassure and calm the person | Keep in quiet area, accompanied | Call ambulance |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Main Groups of Drugs Abused
Patterns of drug misuse change rapidly, depending on fashion and cultural factors, availability and cost. New agents are constantly appearing, often in an attempt to circumnavigate the law and frequently under a variety of names, and may have adverse effects. For example, benzylpiperazine (BZP; A2, legal E, legal XTC, legal high, Jax, London Underground, Pep twisted or Pep love) appeared as an alternative to ecstasy but caused serious adverse effects (see http://www.justice.gov/dea/druginfo/factsheets.shtml and http://www.talktofrank.com/home_html.aspx; accessed 30 September 2013).
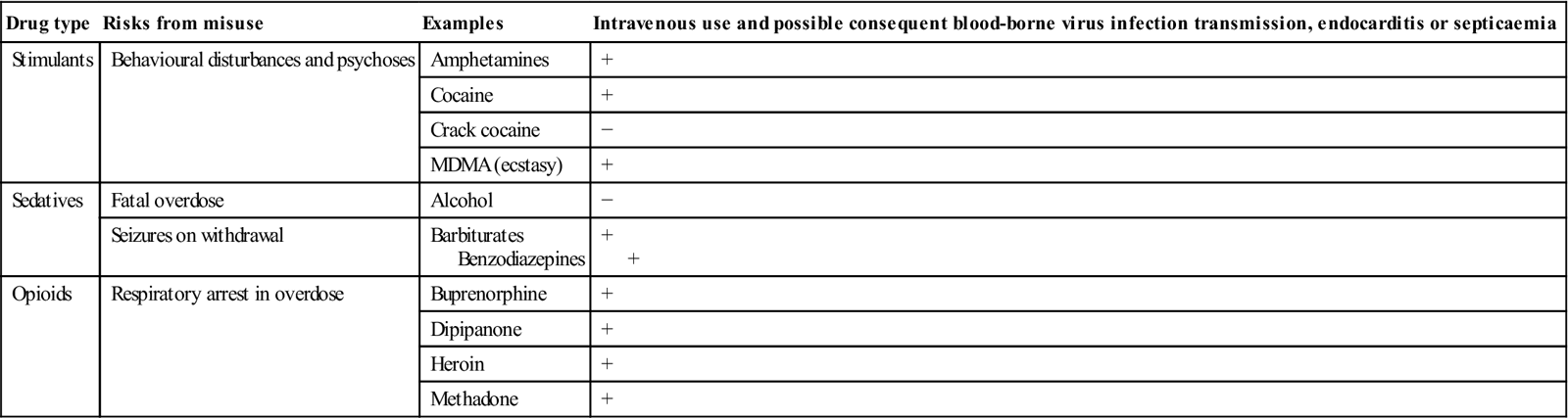
The main groups of drugs abused are stimulants (uppers), depressants (hypnotics/sedatives/downers), hallucinogens (psychedelics) and anabolic steroids (Table 34.5). Alcohol, tobacco, solvents, cannabis and ecstasy have been popular for many years; apart from these, heroin is the main drug of misuse, followed closely by mephedrone, methadone and cocaine (Tables 34.5 and 34.6). Other drugs commonly abused include amphetamines, barbiturates, benzodiazepines, methaqualone and opium alkaloids. Drugs abused may be obtained legally from a doctor or chemist, or may be illicitly obtained. They may be taken orally, inhaled, or injected into the skin, muscle or a vein.
Table 34.5
Common drugs of misuse and the possible consequences
< ?comst?>
| Drug type | Risks from misuse | Examples | Intravenous use and possible consequent blood-borne virus infection transmission, endocarditis or septicaemia |
| Stimulants | Behavioural disturbances and psychoses | Amphetamines | + |
| Cocaine | + | ||
| Crack cocaine | − | ||
| MDMA (ecstasy) | + | ||
| Sedatives | Fatal overdose | Alcohol | − |
| Seizures on withdrawal | Barbiturates Benzodiazepines |
+ + |
|
| Opioids | Respiratory arrest in overdose | Buprenorphine | + |
| Dipipanone | + | ||
| Heroin | + | ||
| Methadone | + |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Table 34.6
Main groups of substances abused
< ?comst?>
| Stimulants (uppers) | Depressants (hypnotic/sedatives/downers) | Hallucinogens (psychedelics) | Analgesics | Anabolic steroids |
| Actions | ||||
| Speed brain activity | Slow brain activity | Distort brain activity | Decrease pain | Promote growth and muscle |
| Examples | ||||
| Amphetamine, caffeine, cocaine, crack, dextroamphetamine, diethylpropion, mephedrone, methylphenidate, naphyrone, nicotine, phenmetrazine, tobacco | Anxiolytics: alprazolam, benzodiazepines, clorazepate, meprobamate Barbiturate Ethanol (alcohol) Inhalants: amyl nitrite, butyl nitrite, enflurane, ether, halothane, isoflurane, nitrous oxide, petrol, solvents (various) |
Lysergic acid diethylamide (LSD), mephedrone, mescaline (peyote), methyl-dimethoxy amphetamine (STP; DOM), methylene dioxyamphetamine (MDA), 3,4-methylenedioxy-methamphetamine (MDMA; ecstasy), phencyclidine (PCP), psilocybin Cannabinoids: marijuana |
Opioids: codeine, fentanyl, heroin, hydrocodone, lomotil, pethidine (meperidine), methyl-phenyl-tetra-hydropyridine (MPTP), morphine, oxycodone, propoxyphene | Nandrolone (Deca-Durabolin), Sustanon 250, Dianabol, Anavar, stanozolol |
| Main CNS and adverse effects | ||||
| Exhilaration, energy, reduced appetite, weight loss, alertness; rapid or irregular heart beat; raised heart rate, blood pressure, metabolism | Feeling of well-being; lowered inhibitions; slowed pulse and breathing; lowered blood pressure; poor concentration, confusion, fatigue; impaired coordination, memory, judgment; respiratory depression and arrest | Altered states of perception and feeling; nausea, psychoses, persisting perception disorder (flashbacks) | Pain relief, euphoria, drowsiness, nausea, confusion, constipation, sedation, respiratory depression and arrest, unconsciousness, coma | No intoxication effects |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Prescription drugs are commonly abused – notably stimulants, CNS depressants, analgesics and opioids.
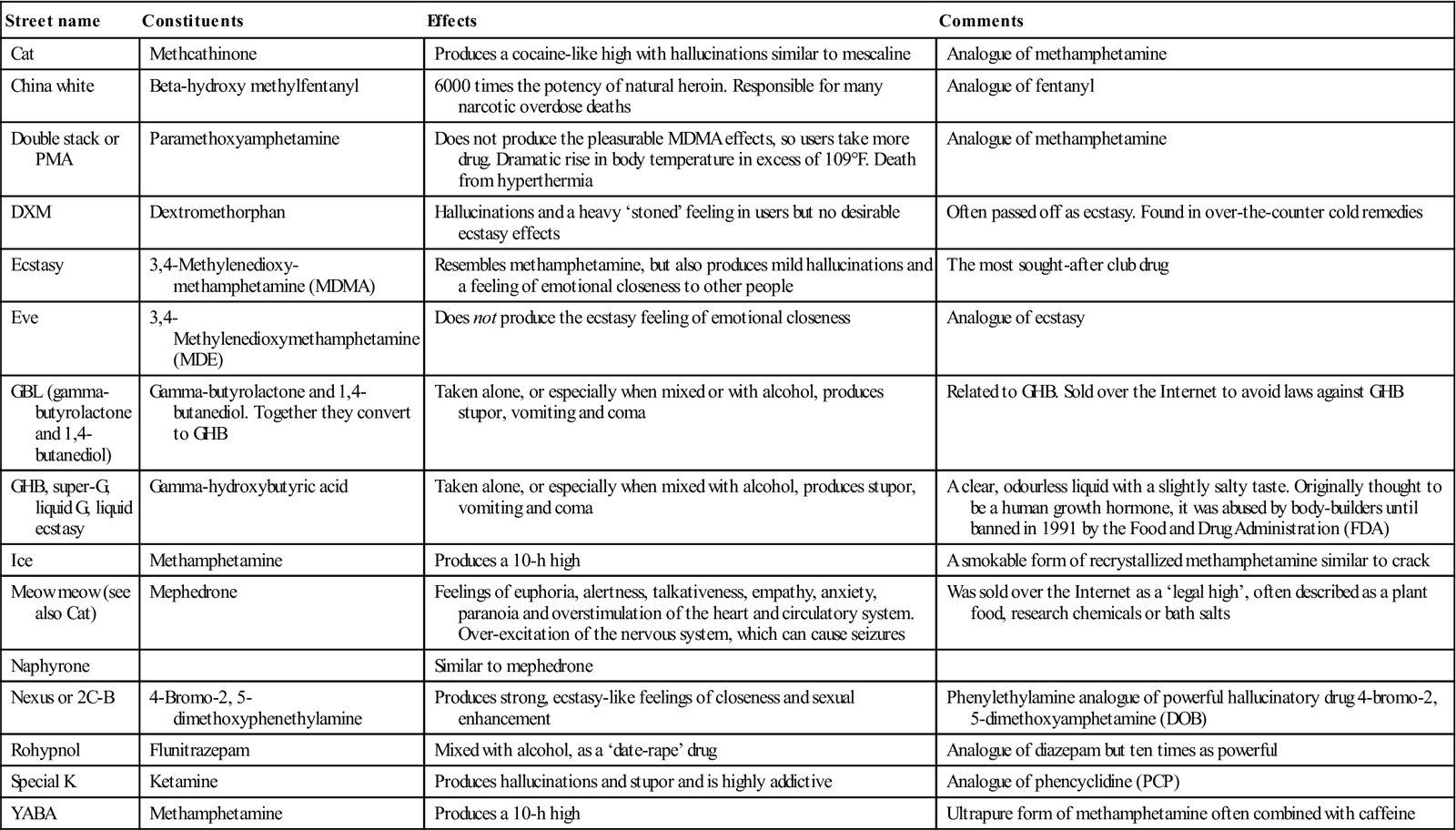
Club drugs are those used by teenagers and young adults who are part of a nightclub, bar, trance or rave scene – night-long dances, often held in warehouses (Table 34.7). In high doses, club drugs can cause a sharp rise in body temperature (malignant hyperthermia) leading to muscle breakdown and renal and cardiovascular system failure.
Table 34.7
< ?comst?>
| Street name | Constituents | Effects | Comments |
| Cat | Methcathinone | Produces a cocaine-like high with hallucinations similar to mescaline | Analogue of methamphetamine |
| China white | Beta-hydroxy methylfentanyl | 6000 times the potency of natural heroin. Responsible for many narcotic overdose deaths | Analogue of fentanyl |
| Double stack or PMA | Paramethoxyamphetamine | Does not produce the pleasurable MDMA effects, so users take more drug. Dramatic rise in body temperature in excess of 109°F. Death from hyperthermia | Analogue of methamphetamine |
| DXM | Dextromethorphan | Hallucinations and a heavy ‘stoned’ feeling in users but no desirable ecstasy effects | Often passed off as ecstasy. Found in over-the-counter cold remedies |
| Ecstasy | 3,4-Methylenedioxy-methamphetamine (MDMA) | Resembles methamphetamine, but also produces mild hallucinations and a feeling of emotional closeness to other people | The most sought-after club drug |
| Eve | 3,4-Methylenedioxymethamphetamine (MDE) | Does not produce the ecstasy feeling of emotional closeness | Analogue of ecstasy |
| GBL (gamma-butyrolactone and 1,4-butanediol) | Gamma-butyrolactone and 1,4-butanediol. Together they convert to GHB | Taken alone, or especially when mixed or with alcohol, produces stupor, vomiting and coma | Related to GHB. Sold over the Internet to avoid laws against GHB |
| GHB, super-G, liquid G, liquid ecstasy | Gamma-hydroxybutyric acid | Taken alone, or especially when mixed with alcohol, produces stupor, vomiting and coma | A clear, odourless liquid with a slightly salty taste. Originally thought to be a human growth hormone, it was abused by body-builders until banned in 1991 by the Food and Drug Administration (FDA) |
| Ice | Methamphetamine | Produces a 10-h high | A smokable form of recrystallized methamphetamine similar to crack |
| Meow meow (see also Cat) | Mephedrone | Feelings of euphoria, alertness, talkativeness, empathy, anxiety, paranoia and overstimulation of the heart and circulatory system. Over-excitation of the nervous system, which can cause seizures | Was sold over the Internet as a ‘legal high’, often described as a plant food, research chemicals or bath salts |
| Naphyrone | Similar to mephedrone | ||
| Nexus or 2C-B | 4-Bromo-2, 5-dimethoxyphenethylamine | Produces strong, ecstasy-like feelings of closeness and sexual enhancement | Phenylethylamine analogue of powerful hallucinatory drug 4-bromo-2, 5-dimethoxyamphetamine (DOB) |
| Rohypnol | Flunitrazepam | Mixed with alcohol, as a ‘date-rape’ drug | Analogue of diazepam but ten times as powerful |
| Special K | Ketamine | Produces hallucinations and stupor and is highly addictive | Analogue of phencyclidine (PCP) |
| YABA | Methamphetamine | Produces a 10-h high | Ultrapure form of methamphetamine often combined with caffeine |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Date-rape drugs, such as gamma-hydroxybutyric acid (GHB), Rohypnol (flunitrazepam) and ketamine, are used because they lack colour, taste and odour, and thus can be added to beverages to be ingested unknowingly by the victim. They are CNS depressants that cause loss of inhibitions and memory. They can also readily cause unconsciousness.
Stimulants
Stimulants are substances that cause excitement and euphoria (a ‘high’), which may last several hours. Withdrawal symptoms (restlessness, agitation, sleeplessness and depression) may follow. Heavy use of strong stimulants for weeks may cause paranoia and auditory hallucinations – effects that may be irreversible (Table 34.8).
Table 34.8
| Main stimulant groups | Street namesa | Comments |
| Adrenaline (epinephrine) derivatives ephedrine and pseudoephedrine | Bennies, black beauties, crosses, hearts, LA turnaround, speed, truck drivers, uppers | Raised heart rate, blood pressure, metabolism, feelings of exhilaration, energy, increased mental alertness, rapid or irregular heart beat, reduced appetite, weight loss, heart failure, rapid breathing |
| Phentermine Amphetamine |
Hallucinations/tremor, loss of coordination, irritability, anxiousness, restlessness, delirium, panic, paranoia, impulsive behaviour, aggressiveness, tolerance, addiction | |
| Caffeine | Found in tea and coffee, cola and a number of energy drinks | Energy, increased mental alertness, rapid or irregular heart beat |
| Cocaine Cocaine hydrochloride |
Blow, bump, C, candy, charlie, coke, crack, flake, rock, snow, toot, white | Raised temperature, chest pain, respiratory failure, nausea, abdominal pain, strokes, seizures, headaches, malnutrition |
| Methylenedioxy-methamphetamine (MDMA) | DOB, DOM, MDA, adam, clarity, ecstasy, eve, lover’s speed, peace, STP, X, XTC, E, pills, XTC, disco biscuits, Mitsubishis, Rolexs, dolphins | Mild hallucinogenic effects, increased tactile sensitivity, empathic feelings, hyperthermia, impaired memory and learning |
| Methamphetamine | Chalk, crank, crystal, fire, glass, go fast, ice, meth, speed | Aggression, violence, psychotic behaviour, memory loss, cardiac and neurological damage, impaired memory and learning, tolerance, addiction |
| Mephedrone | White magic, miaow, meph, meow meow, MC, M-CAT, drone, charge, bubble, bounce, 4-MMC | Feelings of euphoria, alertness, talkativeness, empathy, anxiety, paranoia and overstimulation of the heart and circulatory system. Over-excitation of the nervous system, which can cause seizures |
| Methylphenidate | Ritalin, JIF, MPH, R-ball, skippy, the smart drug, vitamin R | Increase or decrease in blood pressure, psychotic episodes, digestive problems, loss of appetite, weight loss |
| Naphyrone | NRG, O-2482 or naphthylpyrovalerone | Similar to mephedrone. Was sold over the Internet as a ‘legal high’, often described as a plant food, research chemicals or bath salts. Feelings of euphoria, alertness, talkativeness, empathy, anxiety, paranoia and overstimulation of the heart and circulatory system. Over-excitation of the nervous system, which can cause seizures |
| Nicotine | Bidis, chew, cigars, cigarettes, smokeless tobacco, snuff, spit tobacco | Tolerance, addiction, additional effects attributable to tobacco exposure – adverse pregnancy outcomes, chronic lung disease, cardiovascular disease, stroke, cancer |
Stimulants cause moderate to severe psychological addiction. Withdrawal is purely psychological and psychosomatic. They include:
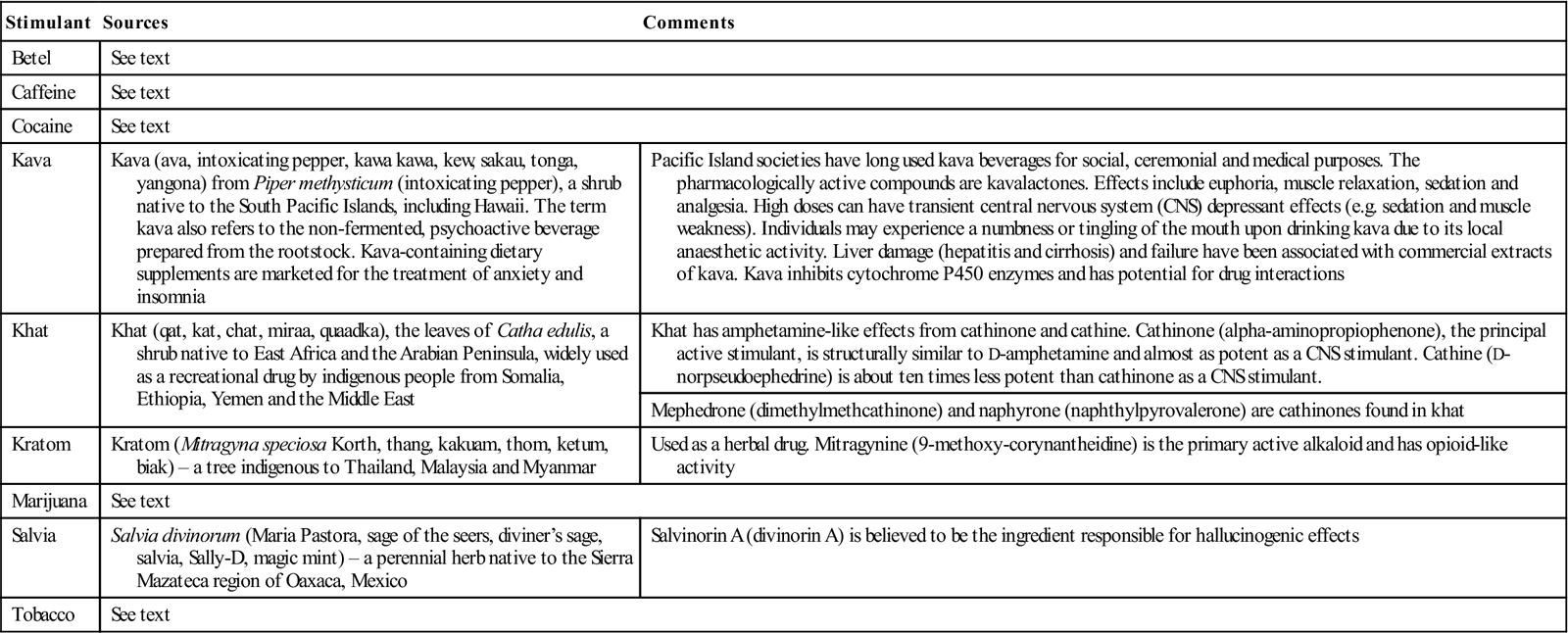
Stimulants used in various cultures include betel, caffeine, cocaine, kava, khat, kratom, marijuana, salvia and tobacco (Table 34.9). Common herbal sources of psychedelics include Psilocybe mushrooms (‘magic mushrooms’), seeds of morning glory (from the Convolvulus family), peyote (from a cactus in the south-west USA), various ayahuasca preparations (from the Banisteriopsis species of vine from Amazonia), San Pedro cactus (from a cactus found in Peru, Bolivia, Chile and Ecuador) and Hawaiian baby woodrose (a vine from India, the Caribbean, Hawaii and Africa).
Table 34.9
Stimulants used in various cultures
< ?comst?>
| Stimulant | Sources | Comments |
| Betel | See text | |
| Caffeine | See text | |
| Cocaine | See text | |
| Kava | Kava (ava, intoxicating pepper, kawa kawa, kew, sakau, tonga, yangona) from Piper methysticum (intoxicating pepper), a shrub native to the South Pacific Islands, including Hawaii. The term kava also refers to the non-fermented, psychoactive beverage prepared from the rootstock. Kava-containing dietary supplements are marketed for the treatment of anxiety and insomnia | Pacific Island societies have long used kava beverages for social, ceremonial and medical purposes. The pharmacologically active compounds are kavalactones. Effects include euphoria, muscle relaxation, sedation and analgesia. High doses can have transient central nervous system (CNS) depressant effects (e.g. sedation and muscle weakness). Individuals may experience a numbness or tingling of the mouth upon drinking kava due to its local anaesthetic activity. Liver damage (hepatitis and cirrhosis) and failure have been associated with commercial extracts of kava. Kava inhibits cytochrome P450 enzymes and has potential for drug interactions |
| Khat | Khat (qat, kat, chat, miraa, quaadka), the leaves of Catha edulis, a shrub native to East Africa and the Arabian Peninsula, widely used as a recreational drug by indigenous people from Somalia, Ethiopia, Yemen and the Middle East | Khat has amphetamine-like effects from cathinone and cathine. Cathinone (alpha-aminopropiophenone), the principal active stimulant, is structurally similar to D-amphetamine and almost as potent as a CNS stimulant. Cathine (D-norpseudoephedrine) is about ten times less potent than cathinone as a CNS stimulant. |
| Mephedrone (dimethylmethcathinone) and naphyrone (naphthylpyrovalerone) are cathinones found in khat | ||
| Kratom | Kratom (Mitragyna speciosa Korth, thang, kakuam, thom, ketum, biak) – a tree indigenous to Thailand, Malaysia and Myanmar | Used as a herbal drug. Mitragynine (9-methoxy-corynantheidine) is the primary active alkaloid and has opioid-like activity |
| Marijuana | See text | |
| Salvia | Salvia divinorum (Maria Pastora, sage of the seers, diviner’s sage, salvia, Sally-D, magic mint) – a perennial herb native to the Sierra Mazateca region of Oaxaca, Mexico | Salvinorin A (divinorin A) is believed to be the ingredient responsible for hallucinogenic effects |
| Tobacco | See text | |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Inhalants are stimulants that are volatile chemical vapours that produce psychoactive effects. Many are available over the counter, including solvents (paint thinners, gasoline, glues), gases (butane, propane, aerosol propellants, nitrous oxide), nitrites (isoamyl, isobutyl, cyclohexyl – used to enhance sexual arousal) and sprays (e.g. deodorants; Table 34.10). ‘Laughing gas’, ‘poppers’, ‘snappers’ and ‘whippets’ are commonly used terms. Sniffing inhalants produces psychotomimetic effects somewhere between those of alcohol and general anaesthesia (GA), in that initially users may feel slightly stimulated; with successive inhalations, they may feel less inhibited and less in control. Users may appear drunk and giggling with slurred speech and unsteadiness. Adverse effects include headache, nausea or vomiting, wheezing, unconsciousness, cramps, weight loss, muscle weakness, depression, memory impairment, damage to cardiovascular and nervous systems, and unconsciousness. Inhalant misuse is increasingly common in children and young adults, and has led to many deaths. Sniffing highly concentrated chemicals such as fluorocarbons and butane-type gases can damage liver and CNS, or cause delusions, hypoxia, arrhythmias and sometimes sudden death. Deliberately inhaling from an attached paper or plastic bag, or in a closed area, greatly increases the chances of suffocation. Users can also choke on their own vomit. Chronic solvent misuse can impair memory and concentration, and permanent damage to the brain, liver or kidneys has been reported. Respiratory damage, anaemia, lead poisoning and cranial nerve palsies can follow chronic misuse of petrol. A syndrome of learning disability, hypotonia, scaphocephaly and high malar bones has also been reported in children of mothers who inhaled petrol during pregnancy (fetal gasoline syndrome). Specific chemicals may also have additional adverse effects (Table 34.11). Signs of solvent misuse include slurred speech, euphoria, anorexia and a circumoral (glue sniffers’) rash. Jaundice may be seen and the pulse may be irregular.
Table 34.10
| Solvents | Gases |
| Industrial or household solvents Art or office supply solvents |
Butane and propane in household or commercial products |
| Paint thinners or solvents, degreasers (dry-cleaning fluids), petrol and glues Correction fluids, felt-tip-marker fluid and electronic contact cleaners |
Aerosol propellants Anaesthetics Whipping cream aerosols or dispensers (whippets) and refrigerant gases |
| Spray paints, hair or deodorant sprays, and fabric protector sprays | |
| Nitrous oxide, halothane, ether and chloroform |
Table 34.11
Adverse effects from inhalants
| Chemical | Found in | Effects |
| Benzene | Petrol | Bone marrow damage |
| Chlorinated hydrocarbons | Correction fluids, dry-cleaning fluids | Liver and kidney damage |
| Hexane | Glues, petrol | Peripheral neuropathies or limb spasms |
| Methylene chloride | Varnish removers, paint thinners | Blood oxygen depletion |
| Nitrites | ‘Poppers’, ‘bold’ and ‘rush’ | Blood oxygen depletion |
| Nitrous oxide | Whipping cream, gas cylinders | Peripheral neuropathies or limb spasms |
| Toluene | Paint sprays, glues, dewaxers | Liver, kidney and central nervous system damage, hearing loss |
| Trichloroethylene | Cleaning fluids, correction fluids | Hearing loss |
Depressants
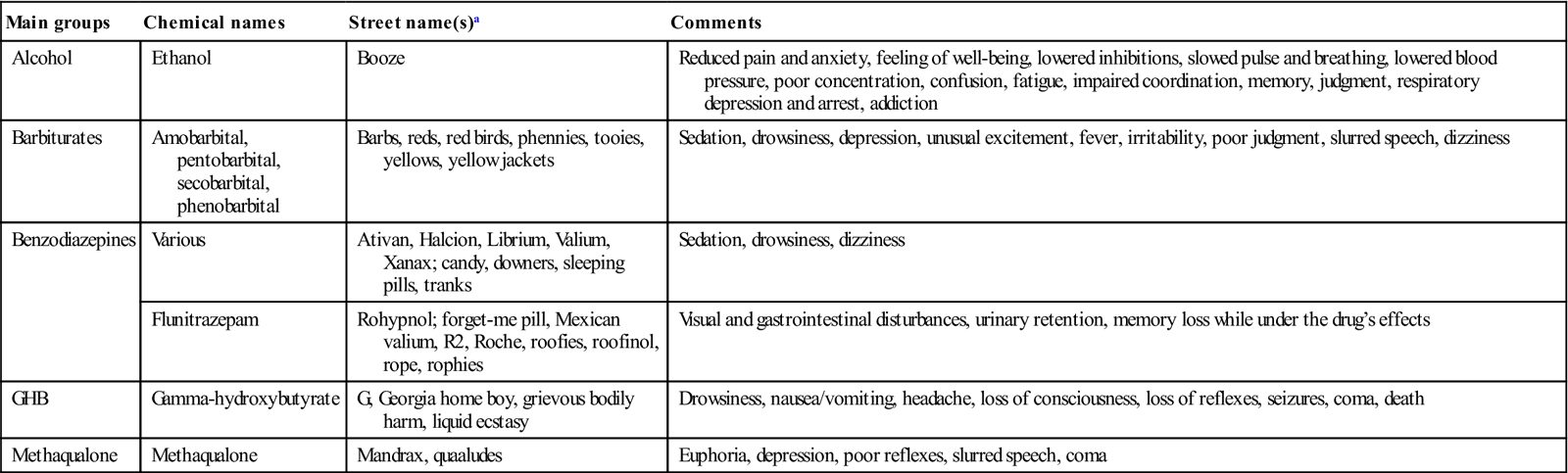
Depressants (including alcohol) depress the CNS, causing drowsiness; poor concentration, judgment and memory; disorientation; ataxia; and, in severe cases, unconsciousness (Table 34.12). Sedatives and hypnotics may cause mild to severe psychological addiction, and severe physiological addiction; abrupt withdrawal may be fatal. They include:
■ alcohol
■ methaqualone and the related quinazolinone sedative-hypnotics
■ opiate and opioid analgesics (mild to severe psychological addiction, mild to severe physiological addiction; abrupt withdrawal is unlikely to be fatal):
morphine and codeine (two naturally occurring opiate analgesics)
synthetic opioids, e.g. fentanyl, pethidine (meperidine) and methadone.
Table 34.12
< ?comst?>
| Main groups | Chemical names | Street name(s)a | Comments |
| Alcohol | Ethanol | Booze | Reduced pain and anxiety, feeling of well-being, lowered inhibitions, slowed pulse and breathing, lowered blood pressure, poor concentration, confusion, fatigue, impaired coordination, memory, judgment, respiratory depression and arrest, addiction |
| Barbiturates | Amobarbital, pentobarbital, secobarbital, phenobarbital | Barbs, reds, red birds, phennies, tooies, yellows, yellow jackets | Sedation, drowsiness, depression, unusual excitement, fever, irritability, poor judgment, slurred speech, dizziness |
| Benzodiazepines | Various | Ativan, Halcion, Librium, Valium, Xanax; candy, downers, sleeping pills, tranks | Sedation, drowsiness, dizziness |
| Flunitrazepam | Rohypnol; forget-me pill, Mexican valium, R2, Roche, roofies, roofinol, rope, rophies | Visual and gastrointestinal disturbances, urinary retention, memory loss while under the drug’s effects | |
| GHB | Gamma-hydroxybutyrate | G, Georgia home boy, grievous bodily harm, liquid ecstasy | Drowsiness, nausea/vomiting, headache, loss of consciousness, loss of reflexes, seizures, coma, death |
| Methaqualone | Methaqualone | Mandrax, quaaludes | Euphoria, depression, poor reflexes, slurred speech, coma |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
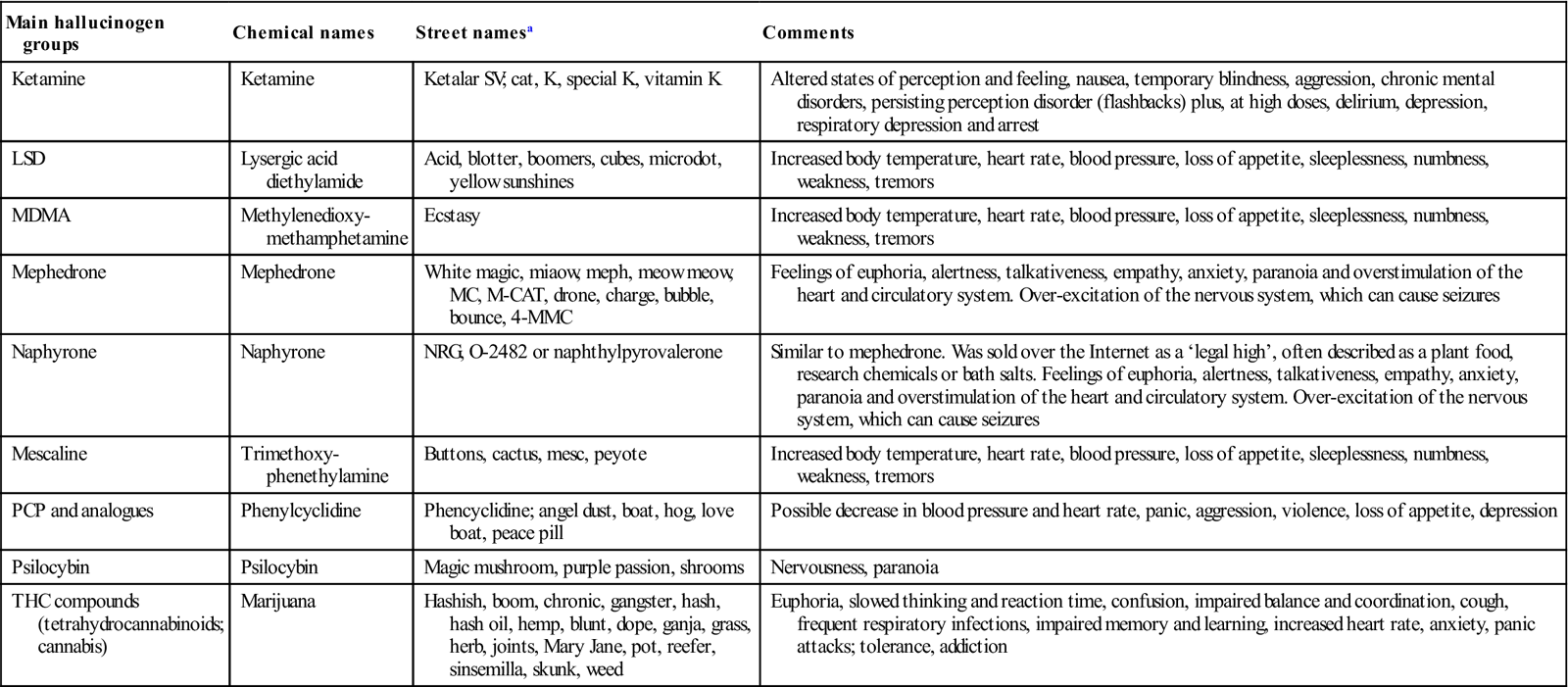
Hallucinogens
Hallucinogenic drugs cause sensory distortions, including mood changes, feelings of disassociation, auditory and visual disturbances, and changes to taste or smell. Hallucinations are quite dangerous, as sufferers may present extreme danger either to themselves or to others (Table 34.13).
Table 34.13
< ?comst?>
| Main hallucinogen groups | Chemical names | Street namesa | Comments |
| Ketamine | Ketamine | Ketalar SV; cat, K, special K, vitamin K | Altered states of perception and feeling, nausea, temporary blindness, aggression, chronic mental disorders, persisting perception disorder (flashbacks) plus, at high doses, delirium, depression, respiratory depression and arrest |
| LSD | Lysergic acid diethylamide | Acid, blotter, boomers, cubes, microdot, yellow sunshines | Increased body temperature, heart rate, blood pressure, loss of appetite, sleeplessness, numbness, weakness, tremors |
| MDMA | Methylenedioxy- methamphetamine | Ecstasy | Increased body temperature, heart rate, blood pressure, loss of appetite, sleeplessness, numbness, weakness, tremors |
| Mephedrone | Mephedrone | White magic, miaow, meph, meow meow, MC, M-CAT, drone, charge, bubble, bounce, 4-MMC | Feelings of euphoria, alertness, talkativeness, empathy, anxiety, paranoia and overstimulation of the heart and circulatory system. Over-excitation of the nervous system, which can cause seizures |
| Naphyrone | Naphyrone | NRG, O-2482 or naphthylpyrovalerone | Similar to mephedrone. Was sold over the Internet as a ‘legal high’, often described as a plant food, research chemicals or bath salts. Feelings of euphoria, alertness, talkativeness, empathy, anxiety, paranoia and overstimulation of the heart and circulatory system. Over-excitation of the nervous system, which can cause seizures |
| Mescaline | Trimethoxy-phenethylamine | Buttons, cactus, mesc, peyote | Increased body temperature, heart rate, blood pressure, loss of appetite, sleeplessness, numbness, weakness, tremors |
| PCP and analogues | Phenylcyclidine | Phencyclidine; angel dust, boat, hog, love boat, peace pill | Possible decrease in blood pressure and heart rate, panic, aggression, violence, loss of appetite, depression |
| Psilocybin | Psilocybin | Magic mushroom, purple passion, shrooms | Nervousness, paranoia |
| THC compounds (tetrahydrocannabinoids; cannabis) | Marijuana | Hashish, boom, chronic, gangster, hash, hash oil, hemp, blunt, dope, ganja, grass, herb, joints, Mary Jane, pot, reefer, sinsemilla, skunk, weed | Euphoria, slowed thinking and reaction time, confusion, impaired balance and coordination, cough, frequent respiratory infections, impaired memory and learning, increased heart rate, anxiety, panic attacks; tolerance, addiction |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Anabolic Steroids
See Chapter 33.
Alphabet of Drugs of Misuse
Appendix 34.1 gives the main street names for the most important drugs of abuse but there are many others (see http://www.drugrehab.co.uk/street-drug-names.htm).
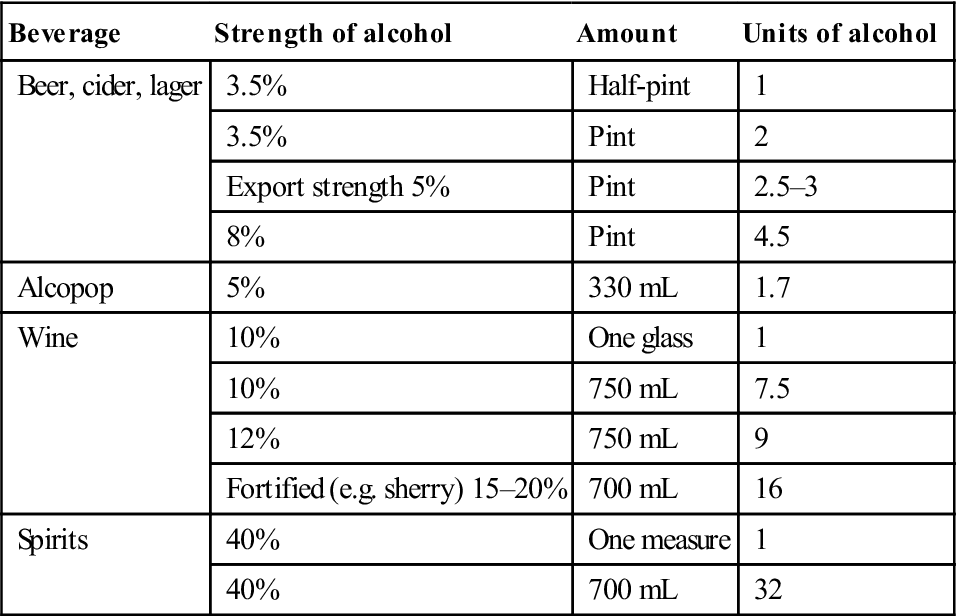
Alcohol
Alcohol (ethanol) is the most common drug of abuse. It accounts for about as much of the burden of world disease as tobacco and hypertension, is exceeded only by the burdens caused by malnutrition and unsafe sex (Fig. 34.2), and consumption is rising across the globe. Alcohol in drinks is generally measured in units (Table 34.14): 1 alcohol unit (AU) equates to 10–12 mL of pure ethanol, contained in a standard bottle or a can of regular beer, a glass of dinner wine (125 mL), a small glass (30 mL) of spirits and a measure (60 mL) of aperitif. Moderate alcohol use is defined as 1 AU daily for women and 2 for men. A safe maximum daily alcohol consumption is generally regarded as 3 units for a man and 2 for a woman. Alcohol misuse, defined as a daily intake in excess of 5 units, is the most common form of drug misuse. The World Health Organization estimates that there are almost 80 million people worldwide with diagnosable alcohol misuse disorders. Over 25% of the UK population appear to drink to excess (44% of men in Scotland also drink to excess). There seems to be a genetic predilection to alcoholism.
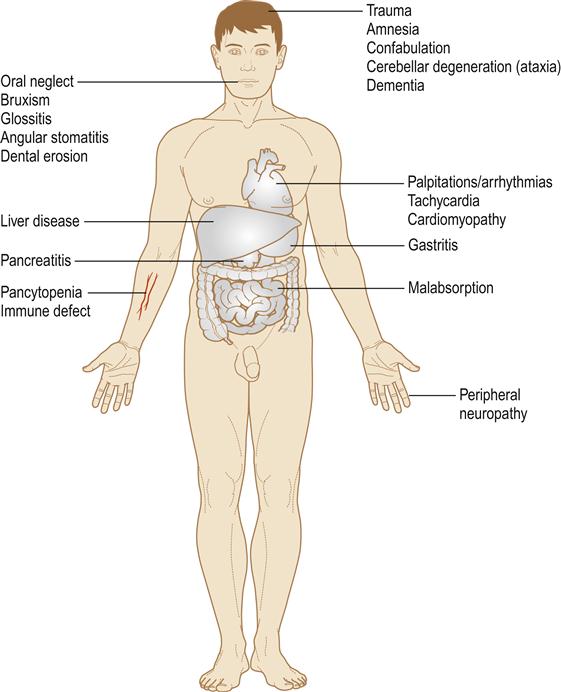
Table 34.14
Alcohol in various alcoholic beverages
< ?comst?>
| Beverage | Strength of alcohol | Amount | Units of alcohol |
| Beer, cider, lager | 3.5% | Half-pint | 1 |
| 3.5% | Pint | 2 | |
| Export strength 5% | Pint | 2.5–3 | |
| 8% | Pint | 4.5 | |
| Alcopop | 5% | 330 mL | 1.7 |
| Wine | 10% | One glass | 1 |
| 10% | 750 mL | 7.5 | |
| 12% | 750 mL | 9 | |
| Fortified (e.g. sherry) 15–20% | 700 mL | 16 | |
| Spirits | 40% | One measure | 1 |
| 40% | 700 mL | 32 |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
The term ‘alcohol’, as used in medicine and by the lay public, typically applies to ethanol (CH3CH2OH), which is produced by yeast fermentation of carbohydrates, such as in fruit and starch. Fermentation is incomplete in beer but complete in wine, with resulting alcohol contents of 3–8% and 7–18% by volume, respectively. Spirits (e.g. whisky, brandy and vodka) are produced by distillation of fermented products, and are 30% or greater alcohol by volume.
A cocktail is a mixed drink usually containing one or more alcoholic beverages, flavourings and one or more fruit juices, sauces, honey, milk, cream or spices, etc. A subgroup of cocktails are pre-mixed and bottled cocktails, generally known as alcopops, RTDs (ready to drink) or FABs (flavoured alcoholic beverages); they are usually made from vodka, beer, whisky or rum, to reach an alcohol concentration of 4–7% by volume, and are sweet and fruit-flavoured because they are mixed with cola, lemonade, ginger ale, etc.
Ethanol is rapidly absorbed through the gastric and duodenal mucosae, and metabolized by the liver, with a small fraction metabolized by oral and upper digestive tract mucosa. Alcohol dehydrogenase catalyses ethanol oxidation to acetaldehyde, which is oxidized into non-toxic acetate by aldehyde dehydrogenase. In turn, acetate is oxidized into fatty acids, carbon dioxide and water. Ethanol blocks nitrosamine metabolism in the liver, thus allowing nitrosamines to circulate to other organs, such as the kidneys and oesophagus, where they can be activated into carcinogens. Alcoholic beverages also contain polyphenols – plant secondary metabolites, which play an important protective role via their potent antioxidant activity; resveratrol in red wine is one example. In contrast, the diet of alcoholics is often B-vitamin–deficient.
Clinical features
Alcohol is a CNS depressant and can have a range of mental effects (



