34
Postoperative management
The role of the anaesthetist is not limited to theatres. There may be a number of postoperative responsibilities to undertake, both in the recovery room and on the surgical ward.
Analgesia
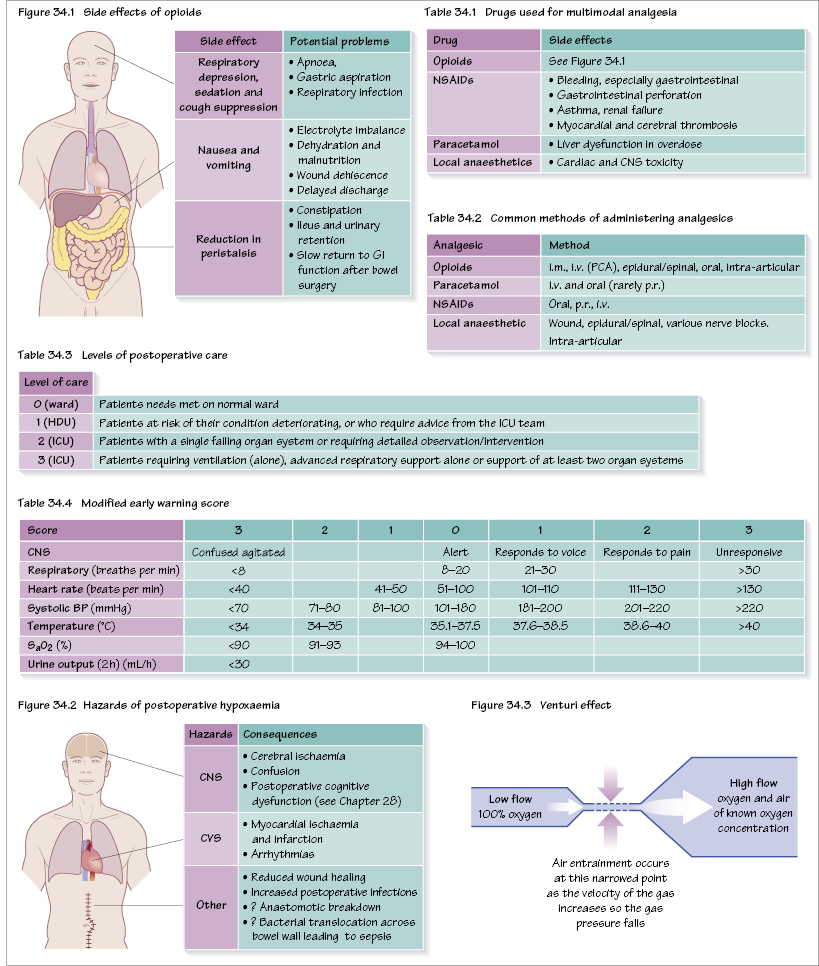
Multimodal analgesia is used, which works on the principle that drugs acting by different mechanisms can result in additive or synergistic analgesia with lowered adverse effects. In particular there is an attempt to minimize opioids (‘opioid sparing’) to reduce their adverse effects (Figure 34.1).
Some of the different drugs that have been used are shown in Table 34.1. The mainstay of analgesia is paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), local anaesthetics and opioids. Safety is paramount in pain management. Most pain is self-limiting, with analgesic requirements falling by 48 hours, even after major surgery.
A practical approach uses the WHO three step analgesic ladder (see Chapter 13). Simple analgesics should be tried (e.g. NSAIDs and paracetamol), then mild opioids (e.g. codeine, tramadol) and finally strong opioids (e.g. morphine). Regular administration affords better pain control than p.r.n. (as required) administration.
Common methods of administering drugs are listed in Table 34.2. For major surgery the use of infusion devices such as PCAs, epidurals or local anaesthetic infusions around major nerves (e.g. paravertebral/brachial plexus) are used.
Fluids
Patients will require i.v. fluids until they are able to drink normally (see Chapter 5). For some patients no i.v. fluids are required, for others i.v. fluids will be required for several days.
Fluid is required for the following:
- maintenance and interoperative fluid losses;
- replacement of pre-existing losses (e.g. dehydration preoperatively);
- replacement of postoperative losses (e.g. nasogastric losses, bleeding).
The types of fluid are:
- isotonic crystalloid (most often used);
- colloids (for maintaining intravascular volume, early bleeding);
- blood and blood products (for significant haemorrha/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


