Trauma
Ernest W.N. Lam
Radiologic examination is essential for evaluating trauma to the teeth and jaws. The presence, location, and orientation of fracture planes and fragments can be determined, and the involvement of nearby vital anatomic structures can be assessed. Foreign objects that have become embedded within the soft tissues as a result of trauma can be detected. Follow-up images are useful in evaluating the extent of healing after an injury and long-term changes resulting from the trauma.
Applied Radiology
The ideal imaging study may be difficult to perform after trauma because of the nature of the injury and patient discomfort. Although the prescription of the appropriate images should be ordered only after a careful clinical examination, in some cases this is not always possible.
Dentoalveolar Fractures
Although a panoramic image may be useful for localizing injuries to the teeth and supporting structures, it may not have the image resolution to reveal injuries involving the anterior mandible or maxillae or the teeth. Dentoalveolar trauma always requires intraoral images to obtain adequate anatomic detail. A minimum of two intraoral periapical images should be made at different horizontal x-ray beam angulations to identify tooth fractures. Additionally, it is important to image the teeth of the opposing arch. Occlusal views may also be particularly useful depending on the severity of the trauma and the ability of the patient to open the mouth. More recently, small field of view cone-beam computed tomographic (CBCT) imaging has been used to identify tooth fractures, although the results have been variable. The high resolution of the small field systems may be beneficial to imaging such fractures.
If a tooth or a large fragment of a tooth is missing, a chest or abdominal image may be considered to locate the tooth. If there are lacerations in the lips or cheek, a soft tissue image of the area may be obtained by placing an intraoral film or receptor in the mouth adjacent to the traumatized soft tissue and then exposing it. If the laceration is in the tongue, a standard mandibular occlusal image may be exposed, or the tongue can be protruded and then imaged.
Mandibular Fractures
Panoramic imaging may be useful as an initial investigation for assessing mandibular fractures. Should a fracture be suspected to involve the body or alveolar process of the mandible, the addition of an intraoral cross-sectional occlusal view of the mandible may be useful, if this is possible. The open mouth Towne view may be useful in cases of suspected trauma to the mandibular condylar head and neck areas. This view may supplement panoramic imaging, especially in cases of nondisplaced greenstick fractures of the condylar neck. For suspected multiple and complex fractures of the mandible, either CBCT or multidetector computed tomographic imaging (MDCT) is the modality of choice for imaging mandibular trauma, although magnetic resonance imaging (MRI) may be useful to assess soft tissue injury to the temporomandibular joint capsule or articular disk.
Maxillofacial Fractures
Computed tomographic (CT) imaging is the method of choice for imaging fractures of the maxillofacial skeleton, particularly fractures that involve multiple bones.
Radiologic Signs of Fracture
Fractures are often erroneously referred to as “lines” despite their three-dimensional nature. Fractures represent planes of cleavage through a tooth or bone, and these planes extend deep into the tissues. A fracture may be missed if the plane of the fracture is not aligned with the direction of the incident x-ray beam on a single plane image.
The following are general signs that may indicate the presence of a fracture of a tooth or bone:
Traumatic Injuries of the Teeth
Concussion
Definition
The term concussion refers to a crush injury to the vascular structures at the tooth apex and the periodontal ligament resulting in inflammatory edema. There is no displacement, and only minimal loosening of the tooth occurs. The injury may result in mild avulsion of the tooth from its socket, causing its occlusal surface to make premature contact with an opposing tooth during mandibular closing.
Clinical Features
The patient usually complains that the traumatized tooth is tender to touch, which can be confirmed by gentle horizontal or vertical percussion of the tooth. The tooth may also be sensitive to biting forces, although patients usually try to modify their occlusion to avoid contacting the traumatized tooth.
Imaging Features
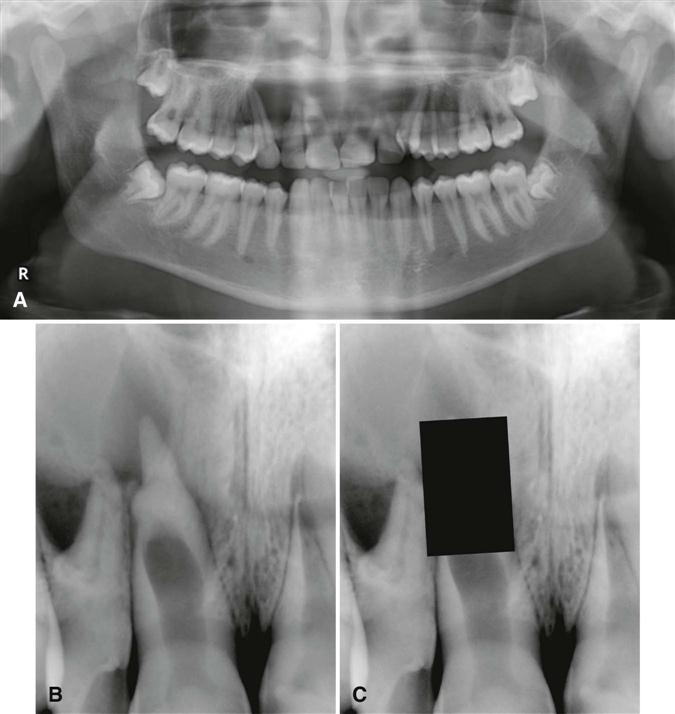
The imaging appearance of a dental concussion may be subtle. No changes may be visible, or there may be localized widening of the apical periodontal ligament space (Fig. 30-1). Changes to the size of the pulp chamber and root canals may develop in the months and years after traumatic injury to the teeth, and this may be particularly evident in teeth that are still developing. Should pulpal necrosis occur after trauma, there may be no further deposition of (secondary) dentin as the odontoblasts and the pulpal and pulpal stem cell populations die.
Teeth that have undergone trauma before apical closure may develop a morphologically abnormal apex, the osteodentin cap. As the pulpal necrosis process begins incisally and progresses apically, vital odontoblasts may remain at the developing root apex, and tertiary dentin (osteodentin) may be deposited ahead of the advancing front of pulpal necrosis. The disorganized and sparse matrix of mineralized material that does develop may resemble bone in structure and a root apex morphologically; as such, it “caps” the end of the root. The osteodentin cap in some instances may appear to be contiguous with the developing root apex or appear separate from it. In contrast to internal resorption where the root canal is focally widened (Fig. 30-2), the root canal seen in association with an osteodentin cap appears uniformly widened from pulp chamber to apex (Fig. 30-3). The development of the canal and deposition of dentin is “frozen in time” at the developmental stage at which pulpal necrosis occurred. When the cap is covered or “hidden” from view, the apex of the root resembles that of a developing tooth (see Fig. 30-3, C).
Management
Because significant displacement of the tooth or teeth does not occur, the appropriate treatment is conservative and may include slight adjustment of the opposing teeth (if necessary) or the application of a flexible splint. Periodic monitoring in the first year with repeated vitality testing and radiographs are indicated. Should rarefying osteitis develop, endodontic treatment is appropriate.
Luxation
Definition
Luxation is a dislocation of the tooth from its socket after severing of the periodontal attachment. Such teeth are abnormally mobile and displaced. Subluxation of the tooth denotes an injury to the supporting structures of the tooth that results in abnormal loosening of the tooth without frank dislocation.
Depending on their magnitude and direction, traumatic forces can cause intrusive luxation (displacement of a tooth into the alveolar process), extrusive luxation (partial displacement of a tooth out of its socket), or lateral luxation (movement of a tooth in a direction other than intrusive or extrusive displacement). In intrusive and lateral luxation, comminution or crushing of the alveolar process may accompany tooth dislocation.
The movement of the apex and disruption of the circulation to the traumatized tooth that accompanies luxation can produce either temporary or permanent changes to the dental pulp, and these changes may result in pulpal necrosis. If the pulp survives the traumatic incident, the rate of dentin formation may accelerate and continue until it obliterates the pulp chamber and root canal. This process may occur in permanent and deciduous teeth.
Clinical Features
An adequate clinical history is helpful in identifying luxation and ordering the appropriate radiographs. Subluxated teeth are in their normal location but are abnormally mobile. There may be extravasated blood emanating from the gingival crevice, indicating periodontal ligament damage, and there may be extreme sensitivity to percussion and masticatory forces.
The clinical crowns of intruded teeth may appear reduced in height. Maxillary incisors may be intruded so deeply into the alveolar process that they appear to be completely avulsed or lost. The displaced tooth may cause some damage to adjacent teeth, particularly if any developing permanent teeth are present in the underlying bone.
Depending on the orientation and magnitude of the force and the shape of the root, it may be pushed through the buccal or, less commonly, the lingual cortex of the alveolar process where it may be seen and palpated. On repeated vitality testing, the sensitivity of a luxated tooth may be temporarily decreased or undetectable, especially shortly after the injury. Vitality may return weeks or several months later.
Usually two or more teeth are involved in luxation injuries, and the teeth most frequently affected are the deciduous and permanent maxillary incisors. The mandibular teeth are seldom affected. The type of luxation appears to vary with age, and this may reflect changes to the nature of maturing bone. Intrusions and extrusions are often found in the deciduous dentition. In the permanent dentition, the intrusive type of luxation is seen less frequently.
Imaging Features
Radiographic examinations of luxated teeth may demonstrate the extent of injury to the root, periodontal ligament, and alveolar process. An image made at the time of injury serves as a valuable reference point for comparison with subsequent radiographs. As with dental concussion, the minor damage associated with subluxation may be subtle and limited to elevation of the tooth from its socket. The sole radiographic finding may be a widening of the apical portion of the periodontal ligament space. Elevation of the tooth may not be apparent on the image.
The depressed position of the crown of an intruded tooth is often apparent on an image (Fig. 30-4), although a minimally intruded tooth may be difficult to demonstrate. Intrusion may result in partial or total obliteration of the apical periodontal ligament space. Multiple radiologic projections, including occlusal views, may be necessary to show the direction of tooth displacement and the relationship of the displaced tooth to adjacent teeth and the outer cortex of bone.

A tooth that has been extruded may demonstrate varying degrees of apical widening of the periodontal ligament space, depending on the magnitude of the extrusive force (Fig. 30-5). A laterally luxated tooth with some degree of extrusion may show a widened periodontal ligament space, with greater width on the side of impact.
Management
A subluxated permanent tooth may be restored to its normal position by digital pressure shortly after the accident. If inflammation precludes repositioning, minimal reduction of opposing teeth may be necessary to minimize any discomfort. The use of a flexible splint may provide additional stability and prevent further damage to the pulp and periodontal ligament. A subluxed deciduous tooth may potentially damage its underlying successor. Consequently, extraction may be considered. If the alveolar bone over the root of a luxated tooth has been fragmented and displaced, the fragments should be repositioned by digital pressure. A subluxated primary tooth should be periodically examined after the injury. If it causes discomfort because of extrusion, it can be removed without undue concern for occlusal problems. Subluxed permanent teeth should be monitored in the same manner as teeth that have been concussed.
Avulsion
Definition
The term avulsion is used to describe the complete displacement of a tooth from the alveolar process. Teeth may be avulsed by direct trauma when the force is applied directly to the tooth or by indirect trauma (i.e., when indirect force is applied to teeth as a result of the jaws striking together). Avulsion occurs in about 15% of traumatic injuries to the teeth, with fights being responsible for the avulsion of most permanent teeth and accidental falls accounting for the traumatic loss of most deciduous teeth.
Clinical Features
Maxillary central incisors are the most commonly avulsed teeth from both dentitions. Most often only a single tooth is lost. This injury typically occurs in a relatively young age group when the permanent central incisors are just erupting. Fractures of the alveolar process and lip lacerations may be seen with an avulsed tooth.
Imaging Features
In a recent avulsion, the lamina dura of the empty socket is apparent and usually persists for several months. The missing tooth may be displaced into the adjacent soft tissue, and its image may project over the image of the alveolar process, giving the false impression that it lies within the bone. To differentiate between an intruded tooth and an avulsed tooth lying within the adjacent soft tissues, a soft tissue image of the lacerated lip or tongue should be made. In some instances, new bone within the healing socket may be very dense and simulate a retained root tip (Fig. 30-6).
Management
If the avulsed tooth is not found by clinical or radiologic examination, a chest or abdominal image may be considered to locate it within the airway or gastrointestinal tract. Reimplanting permanent teeth after avulsion is possible; however, the prognosis of the reimplantation depends on the condition of the tooth while it is outside the mouth, the time it is out of its socket, and the viability of the residual periodontal ligament fibers. Endodontic therapy may be necessary after reimplantation, and there may be external root resorption in the months and years after reimplantation. Reimplanting an avulsed deciduous tooth carries the danger of interfering with the underlying developing permanent tooth.
Fractures of the Teeth
Dental Crown Fractures
Definition
Fractures of the dental crown account for about 25% of traumatic injuries to the permanent teeth and 40% of injuries to the deciduous teeth. The most common event responsible for the fracture of permanent teeth is a fall, followed by accidents involving vehicles (e.g., bicycles, automobiles) and blows from foreign objects striking the teeth. Fractures involving only the crown normally fall into three categories:
Clinical Features
Fractures of the dental crowns most frequently involve anterior teeth. Infractions or cracks in the enamel are common, although frequently they may not be readily detectable unless by illumination. Histologic studies show that such cracks pass through the enamel but not into the dentin.
Uncomplicated fractures that involve both the enamel and the dentin of permanent teeth are more common than complicated fractures that include the pulp. In contrast, complicated and uncomplicated fractures occur with near-equal proportions in the deciduous teeth. Uncomplicated crown fractures that involve dentin can be recognized by the contrast in color between dentin and the peripheral layer of enamel. The exposed dentin is usually sensitive to chemical, thermal, and mechanical stimulation. In deep fractures, the pink blush of the pulp may be appreciated through the thin remaining dentin wall. Complicated crown fractures are distinguishable by bleeding from the exposed pulp or by droplets of blood forming from pinpoint exposures. The pulp is visible and may extrude from the open pulp chamber if the fracture is old. The exposed pulp is sensitive to most forms of stimulation.
Imaging Features
Imaging provides information regarding the location and extent of the fracture and the relationship of the fracture plane and fragment to the pulp chamber. The stage of root development of the involved tooth also can be assessed (Fig. 30-7). This initial image also provides a means of comparison for follow-up examinations of the involved teeth.
Management
Although crown infractions do not require treatment, the vitality of the tooth should be evaluated. The sharp edges of enamel that result from an uncomplicated fracture should be smoothed and may require restoration for cosmetic reasons. It is reasonable to delay this procedure for a number of weeks until the pulp has recovered and secondary dentin is laid down. The prognosis for teeth with fractures limited to the enamel is quite good, and pulpal necrosis develops in less than 2% of such cases. If a fracture involves both dentin and enamel, the frequency of pulpal necrosis is about 3%. Oblique fractures have a worse prognosis than horizontal fractures because potentially a greater amount of dentin is exposed. The frequency of pulpal necrosis increases greatly with concussion and mobility of the tooth.
Treatment of complicated crown fractures of permanent teeth may involve pulp capping, pulpotomy, or pulpectomy, depending on the stage of root formation. If a coronal fracture of a deciduous tooth involves the pulp, it is usually best treated by extraction.
Dental Root Fractures
Definition
For horizontal root fractures, the plane of cleavage may extend across the long axis of the root either perpendicularly or obliquely. In contrast, vertical root fractures represent fracture planes that run lengthwise from the crown toward the apex of the tooth, usually through the facial and lingual root surfaces.
Clinical Features
Horizontal root fractures occur more commonly in maxillary central incisors and result from the direct application of traumatic force to the face, alveolar processes, or teeth. In contrast, vertical fractures usually involve the molar teeth in adults. Vertical fractures may be iatrogenic, following the insertion of retention screws or pins into teeth, or the result of high occlusal forces, particularly in restored teeth. Endodontically treated posterior teeth that have not been restored with a full coverage restoration are also at risk.
The mobility of the fractured tooth crown relates to the level of the fracture. That is, the closer the fracture plane is located to the apex, the more stable the tooth is. When testing the mobility of a traumatized tooth, the clinician places a finger over the alveolar process. If movement of only the crown is detected, a root fracture is likely. Fractures of the root may occur with fractures of the alveolar process and are often not detected. This situation is most commonly observed in the anterior region of the mandible where root fractures are infrequent. Although root fracture is usually associated with temporary loss of sensitivity (by all usual criteria), the sensitivity of most teeth returns to normal within about 6 months.
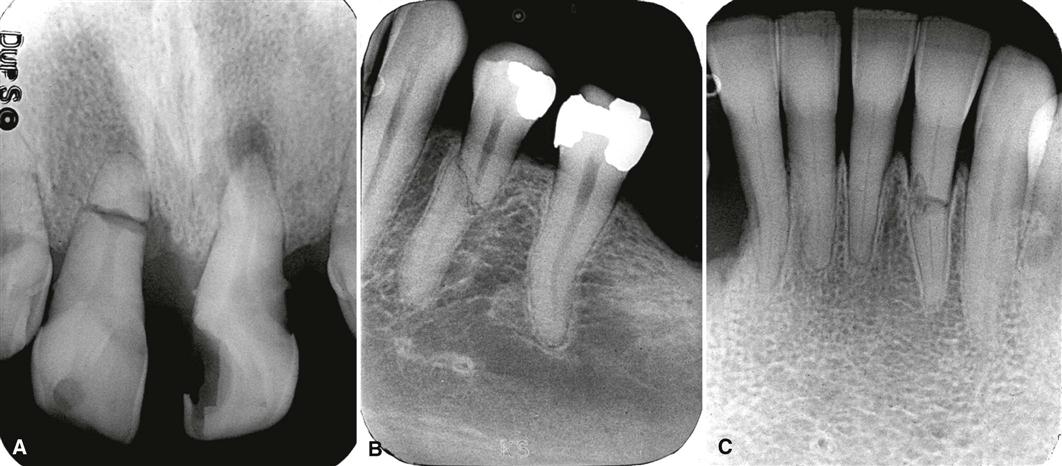
Imaging Features
Horizontal fractures of the dental root may occur at any level and involve one (Fig. 30-8) or all of the roots of multirooted teeth. Most of the fractures confined to the root occur in the middle third of the root. The ability of an image to reveal the presence of a root fracture depends on the relative angulation of the incident x-ray beam to the fracture plane and the degree of separation of the fragments. If the x-ray beam is aligned along the fracture plane, a single sharply defined radiolucent line confined to the anatomic limits of the root may be seen. However, if the orientation of the x-ray beam meets the fracture plane in a more oblique manner, the fracture plane may appear as a more poorly defined single line or as two lines that converge at the mesial and distal surfaces of the root. The appearance of a comminuted root fracture may also be less well defined. Most nondisplaced root fractures are usually difficult to detect, and several views at differing angles may be necessary. In some instances when the fracture line is not visible, the only evidence of a fracture may be a localized increase in the width of the periodontal ligament space adjacent to the fracture site (Fig. 30-9).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses