CHAPTER 30 HYGIENE AND SOFT TISSUE MANAGEMENT
TWO PERSPECTIVES
Postsurgical hygiene and soft tissue management are integral components of any dental implant case. It takes a team of highly skilled dental professionals, along with the patient, to achieve success. Each member of the dental implant team plays a significant role (Table 30-1). This chapter looks at postsurgical hygiene and soft tissue management from the perspectives closest to the patient, the doctor and the dental hygienist.
| Team member | Role |
|---|---|
| Surgeon | Places implant in keratinized tissue with adequate parallelism |
| Restoring Dentist | Provides easily maintainable prosthesis with proper design and high degree of fit |
| Patient | Complies with and commits to long-term care |
| Dental Hygienist | Provides education, motivation, collects assessment data |
| Lab Technician | Delivers highly polished prosthesis with proper design and materials selection |
| Assistant and Other Staff | Motivates and educates |
 The Doctor’s Perspective
The Doctor’s Perspective
Long-term success rates for dental implants are well documented. Growth in the placement and restoration of dental implants has caused an explosion of research and technology to assist clinicians in the quest for implant success. The dynamic nature of implant dentistry offers incredible advances to our knowledge and understanding while challenging our parameters and protocols to undergo constant change and revision in an effort to provide clinicians with a standardized implant health scale. Evaluation and assessment of the presence or lack of health is the first step in treating implant complications. In addition to their legal and ethical necessity, thorough and accurate documentation of baseline data and all maintenance appointments by the dental team is imperative in monitoring implants and their restorations. As the understanding and utilization of dental implants increases, the potential for complications and long-term maintenance challenges also increases. Clinicians are bound to see an increase in problems related to dental implants, especially in complex cases.1 This section outlines factors that the doctor needs to consider throughout the postsurgical implant process.
Evaluation and Assessment
Early changes from baseline data (typically collected by the dental hygienist) are often indicators of a complication that will require further evaluation and possible intervention or correction (Box 30-1). The color, surface texture, size, bleeding, and inflammation of the soft tissue should be assessed.2 Negative findings or changes from baselines should be investigated and appropriate action taken to avoid progression of problems. It is important to remember that implants are not natural teeth and as such may require differences in interpretation of findings.3 Similar to teeth, findings of failing implants include inflammation, pockets, and progressive bone loss.4
Periodontal architecture is well uunderstood,5 and indices to measure changes in the human periodonteum have been used for many years. Adaptation of indices for implants has long been a source of controversy among clinicians. The first step in evaluation should be the understanding of success and failure. Implant quality of health scales have been established by James and further developed by Misch.2,6 In 2007 a Consensus Conference in Pisa, Italy (sponsored by the International Congress of Oral Implantologists, Upper Montclair, NJ) modified the James-Misch health scale and developed categories of implant success, survival, and failure7 (Table 30-2).
| Implant quality scale group | Clinical conditions |
|---|---|
| I. Success (optimum health) |
From ICOI, Pisa, Italy, Consensus Conference, 2007.
Soft Tissue
Assessment of the soft tissue approximating an implant, implant abutment, and restoration is essential to monitor. There has been much controversy about the necessity of keratinized or attached mucosa related to implant success rates. Statistically, we know that attached tissue does help decrease plaque accumulation and gingival inflammation.8 Review of the benefits of keratinized tissue shows that it is preferred at the permucosal site and may be advantageous in avoidance of some long-term implant complications (Box 30-2).
Peri-implant Disease
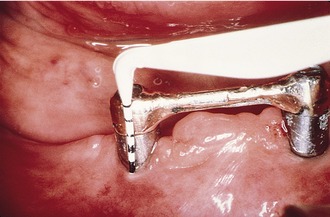
Peri-implantitis is bone loss around an implant that can be caused by bacteria (Figure 30-1). The bacteria responsible for periodontitis and peri-implantitis are the same.9–11 The lack of a connective tissue barrier around implants means bacteria have an easier path of entry to destroy bone. Bone loss and gingival inflammation (a consequence of bacterial plaque) can provide a nidus for anaerobic bacteria, which can be responsible for continued bone loss. Presence of exudate indicates some type of infection. Debridement, treatment with short-term systemic and local antibiotics, and topical chlorhexidine should be employed.3 Continued bone loss and recurrence of exudates may require surgical intervention for correction.
Probing the Dental Implant
Probing the dental implant has been a source of debate for years. It is essential to first note that probing the dental implant leaves you in much closer contact to the bone due to a lack of connective tissue attachment. This proximity to the bone is important to remember because probing force can penetrate the junctional epithelium. Prosthetic design and implant angulation may also inhibit the ability to achieve multiple sites around an implant while trying to maintain correct form (probe parallel to the long axis of the implant [Figure 30-2]). Gingival hyperplasia and hypertrophy can be responsible for increase in pocket depth, and a fixed reference point should be utilized to avoid inaccurate assessment. Probing should be performed in the presence of bone loss (for monitoring purposes) or pathology. Clinicians should use probing not only to measure pockets but also to assess bleeding, exudates, and tissue consistency. Correlation of increased probing depth and bone loss is important.
Bone Loss
The surgical approach and remodeling of the bone after the implant is placed into function may be related to bone loss to the first thread of the implant within the first year of function12 or until the biological width is created and stabilized.13 On average, 0.5 mm of connective tissue will form apical to the abutment/implant junction. Some research has also indicated that the neck of the implant may play a role as to where bone remodels itself and that bone will reposition itself below smooth metal.
Mobility
Implants do not have a periodontal ligament (PDL) and consequently act like ankylosed teeth. Absence of clinical mobility under load is a hallmark for success (Figure 30-3). Prosthetics and their components are often responsible for perceived mobility. However, truly mobile implants represent a failure and should never be restored.
Measuring Success
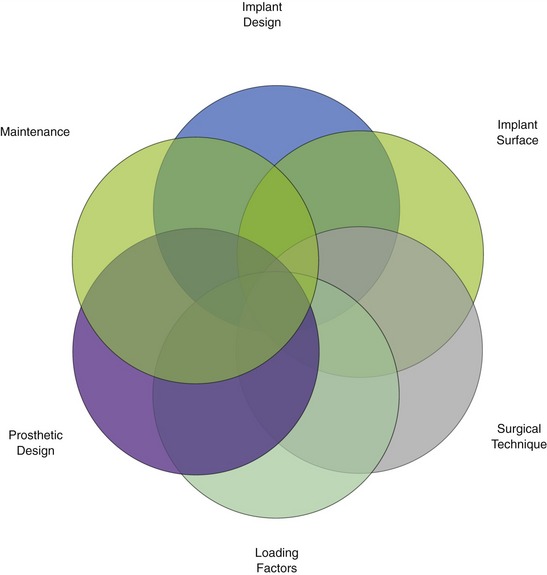
Postsurgical maintenance is essential to a positive outcome in implant surgery. Success in dental implant surgery comes from the interaction of many variables and often of many clinicians (Figure 30-4). The patient’s role is also critical to long-term success (Figure 30-5).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 of implant body)
of implant body) the length of implant
the length of implant