3 TREATMENT PLANNING
IDENTIFICATION OF PATIENT NEEDS
Correction of Existing Disease
Existing disease is revealed during the clinical examination. The disease process can usually be arrested by identification and reduction of the initiating factors, identification and improvement of the resistive factors, or both (Fig. 3-1). For example, oral hygiene instruction helps reduce the amount of residual plaque, an initiating factor, and thus helps reduce the likelihood of further dental caries. It also helps improve gingival health, and the resulting healthy tissue is more resistant to disease.
AVAILABLE MATERIALS AND TECHNIQUES
Plastic Materials
Plastic materials (e.g., silver amalgam or composite resin) are the most commonly used dental restoratives. They allow simple and conservative restoration of damaged teeth. However, their mechanical properties are inferior to those of cast metal or metal-ceramic restorations. Their continued service depends on the strength and integrity of the remaining tooth structure. When the remaining tooth substance needs reinforcement, a cast metal restoration should be fabricated, usually with amalgam as the foundation or core (see Chapter 6).
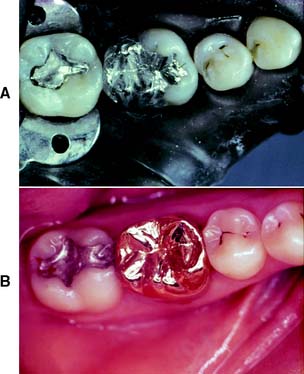
Large amalgam restorations (Fig. 3-2A) are shaped or carved directly in the mouth. The great degree of difficulty associated with this direct approach often results in defective contours and poor occlusion. The indirect procedure, used in making cast metal crowns (Fig. 3-2B), facili-tates the fabrication of more accurately shaped restorations.
Cast Metal
Cast metal crowns are fabricated outside the mouth and are cemented with a luting agent. To minimize exposure of the luting agent to oral fluids, a long-lasting restoration must have good marginal adaptation. The highly refined techniques for overcoming the problem of marginal fit also permit the manufacture of cast metal crowns with precisely shaped axial and occlusal surfaces. This ensures continued periodontal health and good occlusal function. The internal dimensions of a casting must seat without binding against the walls while remaining stable and not becoming displaced during function. Preparation design for cast metal restorations is crucial and is discussed in detail in Chapter 7, Chapter 8, Chapter 9 and Chapter 10.
Intracoronal restorations
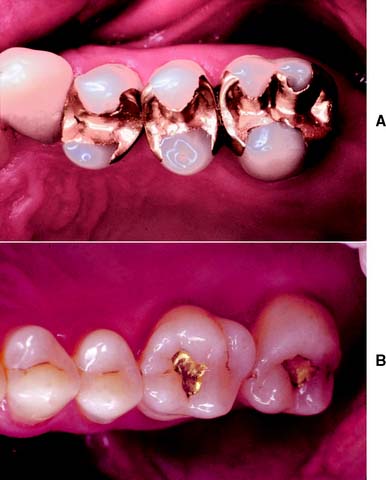
An intracoronal cast metal restoration (Fig. 3-3), or inlay, relies on the strength of the remaining tooth structure for support and retention, just as a plastic restoration does. However, greater tooth bulk is needed to resist any wedging effect on the preparation walls. Therefore, this restoration is contraindicated in a significantly weakened tooth. When fabricated correctly, it is extremely durable because of the strength and corrosion resistance of the gold casting alloy; in a tooth with a minimal proximal carious lesion, however, it usually requires greater removal of tooth structure than does an amalgam preparation. Inlays do not have sufficient resistance or retention to be used as abutment retainers for FDPs.
Extracoronal restorations
An extracoronal cast metal restoration (Fig. 3-4), or crown, encircles all or part of the remaining tooth structure. As such, it can strengthen and protect a tooth weakened by caries or trauma. To provide the necessary bulk of material for strength, considerably more tooth structure must be removed than for an intracoronal restoration. The margins of an extracoronal restoration often must be near the free gingiva, which can make maintenance of tissue health difficult. Tooth preparation for an extracoronal restoration may be combined with intracoronal features (e.g., grooves and pinholes) to gain resistance and retention.
Metal-Ceramic
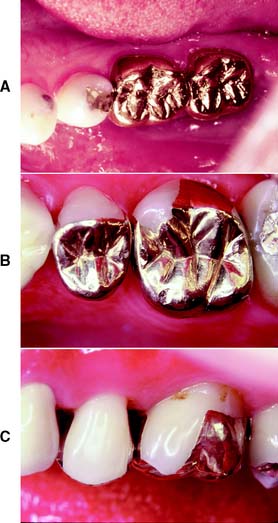
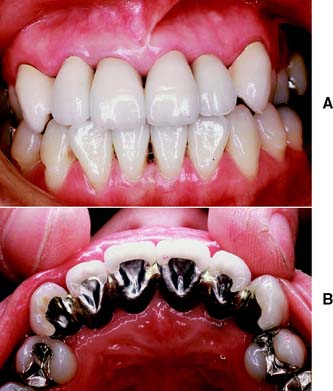
Metal-ceramic restorations (Fig. 3-5) consist of a tooth-colored layer of porcelain bonded to a cast metal substructure. They are used when a complete crown is needed to restore appearance as well as function. Sufficient reduction of tooth structure is necessary to provide space for the bulk of porcelain needed for a natural appearance. Thus, the preparation design for a metal-ceramic crown is among the least conservative, although tooth structure can be conserved if only the most visible part of the restoration is veneered.
The labial margins of a metal-ceramic restoration are often discernible and may detract from its appearance. They can be hidden by subgingival placement, although they then have the potential for increasing gingival inflammation; this should be avoided when possible.1 Appearance can be improved by omitting the metal shoulder and making the labial margin in porcelain. As discussed in Chapter 24, this is a more demanding laboratory procedure.
Resin-Veneered
Resin-veneered restorations were popular before the metal-ceramic technique was fully developed, but problems with wear and discoloration of the polymethyl methacrylate veneer (Fig. 3-6) limited their use to long-term interim restorations. Current resin-veneer techniques2 incorporate bis-GMA–based materials (bisphenol-A glycidyl dimethacrylates), which have better physical properties than do the earlier acrylic resins, and adhesive techniques to improve the bond to the supporting metal.3,4
Fiber-Reinforced Resin
Advances in composite resin technology, especially the introduction of glass and polyethylene fibers,5–7 have prompted the use of indirect composite resin restorations for inlays, crowns, and FDPs. Excellent marginal adaptation and esthetic results are achievable (Fig. 3-7), but because these are newer technologies, little is known about their longer-term performance (see Chapter 27).
Complete Ceramic
Crowns, inlays, and laminate veneers made entirely of dental porcelain can be the most esthetically pleasing of all fixed restorations (Fig. 3-8). Drawbacks include a comparative lack of strength and the difficulties associated with achieving an acceptable marginal fit. The current focus in improving strength lies with either veneering a high-strength alumina, zirconia, spinel, or lithium disilicate core8–10 with a more translucent porcelain or using a leucite-reinforced translucent material11–13 (see Chapter 25). Complete ceramic restorations are fabricated by an indirect technique and generally retained with composite resin. Acid etching is used to provide retention “keys.”
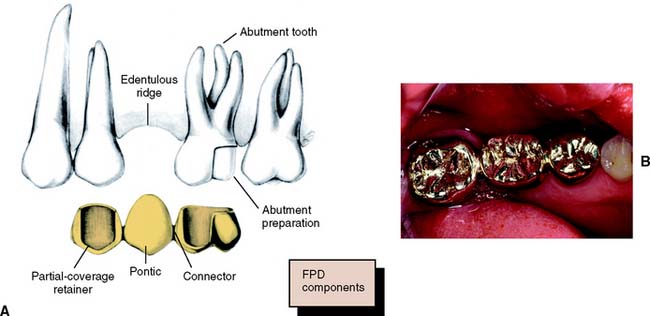
Fixed Dental Prostheses
An FDP (Fig. 3-9) is often indicated when one or more teeth require removal or are missing. Such teeth are replaced by pontics that are designed to fulfill the functional and often the esthetic requirements of the missing teeth (see Chapter 20). Pontics are connected to retainers, which are the restorations on prepared abutment teeth.
All the components of an FDP are fabricated and assembled in the laboratory before cementation in the mouth. This requires precise alignment of tooth preparations. Because unseating forces on individual retainers can be considerable, highly retentive restorations are essential. FDPs have been demonstrated to have exceptional long-term success,14 which is ensured by controlling the magnitude and direction of forces and by making sure the patient practices appropriate oral hygiene measures.
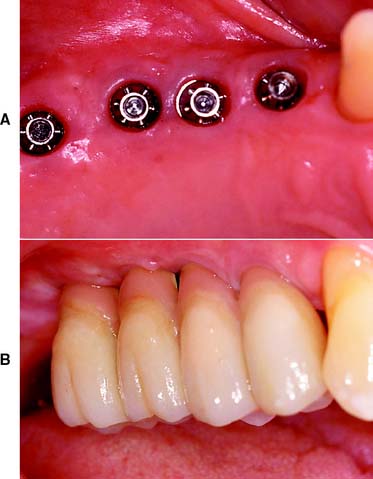
Implant-Supported Prostheses
Single or multiple missing teeth can be replaced with an implant-supported prosthesis (Fig. 3-10). For the successful “osseointegrated” technique, the bone is atraumatically drilled to receive precisely fitting titanium cylinders.15 These are left in place without loading for some months until they are invested with bone. Only then are function and esthetics restored with a prosthesis (see Chapter 13).
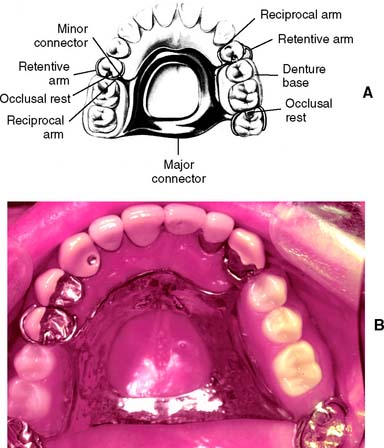
Partial Removable Dental Prosthesis
A partial removable dental prosthesis (RDP) (Fig. 3-11) is designed to replace missing teeth and their supporting structures. Forces applied to a well-designed prosthesis are distributed to the remaining teeth and the residual alveolar ridges. These forces are most accurately controlled if the abutment teeth are provided with fixed cast restorations that have carefully contoured guide planes and rest seats (see Chapter 21).
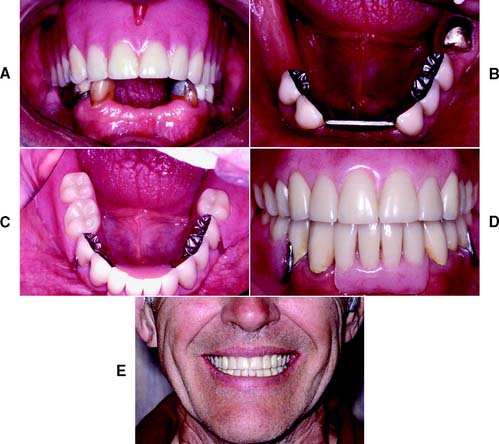
Complete Dentures
Some of the difficulties encountered with complete dentures relate to the lack of denture stability and a gradual loss of supporting bone. Stability is enhanced if the denture has a carefully designed occlusion. Problems with stability can be especially severe when the mandibular incisors are the only teeth retained, with ensuing damage to the opposing premaxilla,16 although any treatment plan that involves a complete denture opposing fixed restorations requires careful planning of the occlusion (Fig. 3-12). For selected patients, providing an overdenture that rests on endodontically treated roots may help preserve the residual ridge and enhance the stability of the complete denture.17
TREATMENT OF TOOTH LOSS
A treatment plan involving fixed prosthodontics generally includes the replacement of missing teeth. Most teeth are lost as a result of dental caries or periodontal disease. In rare cases, they may be congenitally absent or lost as a result of trauma or neoplastic disease.
Decision to Remove a Tooth
The decision to remove a tooth is part of the treatment-planning process and is made after assessing the advantages and disadvantages associated with retention of the tooth. Sometimes it is possible to retain a tooth with an apparently hopeless prognosis by using highly specialized and complex techniques. In other cases, removing the tooth is the treatment of choice (Fig. 3-13). A decision about replacing a missing tooth is best made at the time its removal is recommended, rather than months or years after the fact.
Consequences of Removal without Replacement
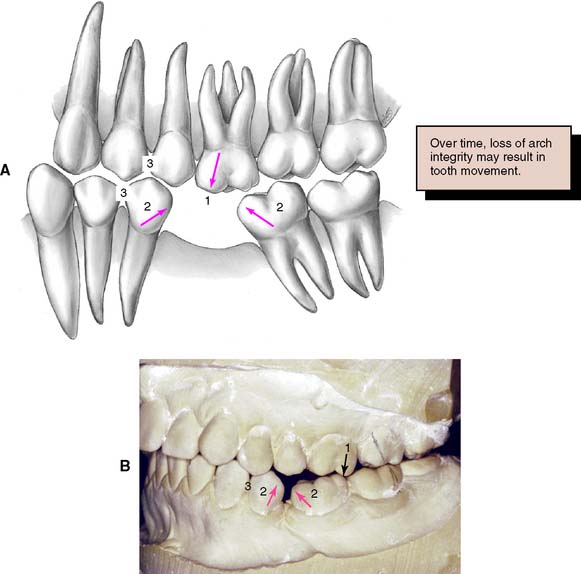
The decision to replace or not replace missing teeth requires a careful analysis of the costs and benefits of the action. The loss of posterior occlusion may lead to excessive forces on the remaining dentition with consequent damage and poor function. However, studies have demonstrated that adequate function is possible with reduced posterior occlusion.18 Deciding not to replace a tooth may lead to a situation in which the balance of the forces exerted on that tooth by the adjacent and opposing teeth and supporting tissues and by the soft tissues of the cheeks, lips, and tongue is upset (Fig. 3-14). The consequences may be supraclusion of the opposing tooth or teeth, tilting of the adjacent teeth, and loss of proximal contact (with resulting disturbances in the health of the supporting structures and the occlusion). However, the teeth adjacent to an edentulous space have not been shown to be at greater risk of damage,19 and the rate of change of teeth adjacent to an edentulous space is usually slow.20
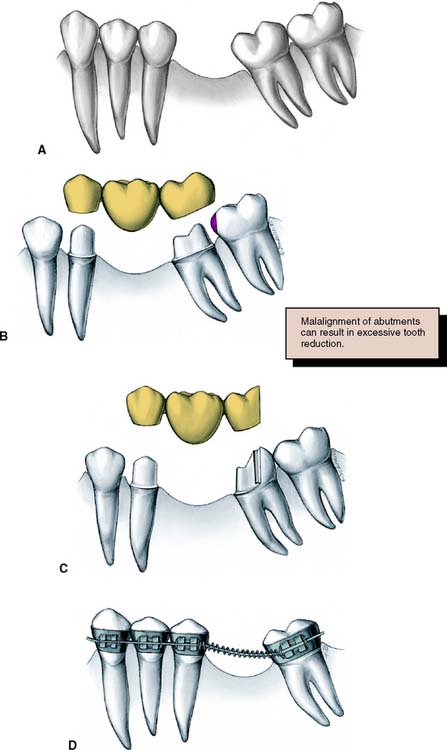
SELECTION OF ABUTMENT TEETH
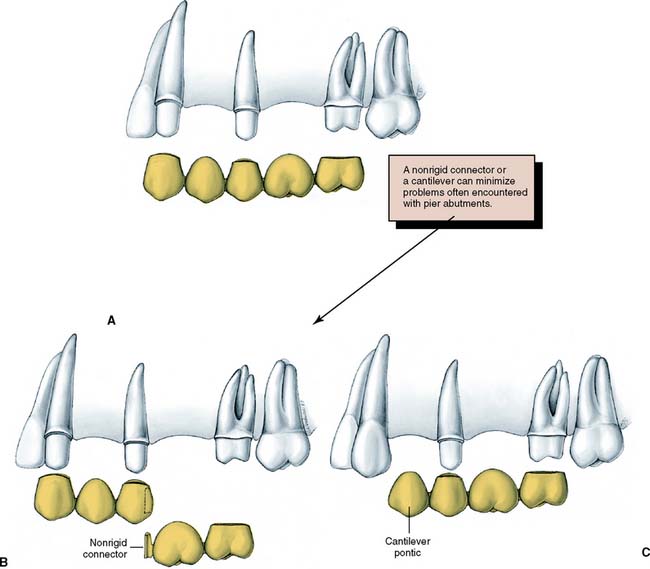
Whenever possible, FDPs should be designed as simply as possible, with a single well-anchored retainer fixed rigidly at each end of the pontic. The use of multiple splinted abutment teeth, nonrigid connectors, or intermediate abutments makes the procedure much more difficult, and often the result compromises the long-term prognosis (Fig. 3-15).
Replacement of a Single Missing Tooth
Unless bone support has been weakened by advanced periodontal disease, a single missing tooth can almost always be replaced by a three-unit FDP that includes one mesial and one distal abutment tooth. An exception is when the FDP is replacing a maxillary or mandibular canine. Under these circumstances, the small anterior abutment tooth needs to be splinted to the central incisor to prevent lateral drift of the FDP.
Cantilever fixed dental prostheses
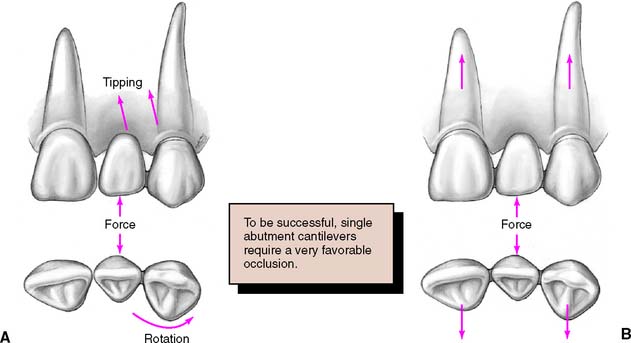
However, the long-term prognosis of the single-abutment cantilever is poor.21 Forces are best tolerated by the periodontal supporting structures when directed in the long axes of the teeth.22 This is the case when a simple three-unit FDP is used. A cantilever induces lateral forces on the supporting tissues, which may be harmful and lead to tipping, rotation, or drifting of the abutment (Fig. 3-16). Laboratory analysis23,24 has confirmed the potential harmful nature of such FDPs. However, clinical experience with resin-retained FDPs has suggested that cantilever designs may be preferred, especially because re-adhesion after failure is greatly facilitated25 (see Chapter 26).
When multiple missing teeth are replaced, cantilever FDPs have considerable application (see Fig. 3-20). The harmful tipping forces are resisted by multiple abutment teeth, and movement of the abutments is unlikely. Cantilevers are also successfully used with implant-supported prostheses (see Chapter 13).
Assessment of abutment teeth
Considerable time and expense are spared, and loss of a patient’s confidence can be avoided, by thoroughly investigating each abutment tooth before proceeding with tooth preparation. Radiographs are made, and pulpal health is assessed by evaluating the response to thermal and electrical stimulation. Existing restorations, cavity liners, and residual caries are removed26 (preferably under a rubber dam), and a careful check is made for possible pulpal exposure. Teeth in which pulpal health is doubtful should be endodontically treated before the initiation of fixed prosthodontics. Although a direct pulp cap may be an acceptable risk for a simple amalgam or composite resin, conventional endodontic treatment is normally preferred for cast restorations, especially when the later need for endodontic treatment would jeopardize the overall success of treatment.
Endodontically treated abutments
If a tooth is properly treated endodontically, it can serve well as an abutment with a post and core foundation for retention and strength (see Chapter 12). Failures occur, however, particularly on teeth with short roots or little remaining coronal tooth structure. Care is needed to obtain maximum retention for the post and core. Sometimes it is better to recommend removal of a badly damaged tooth rather than to attempt endodontic treatment.
Unrestored abutments
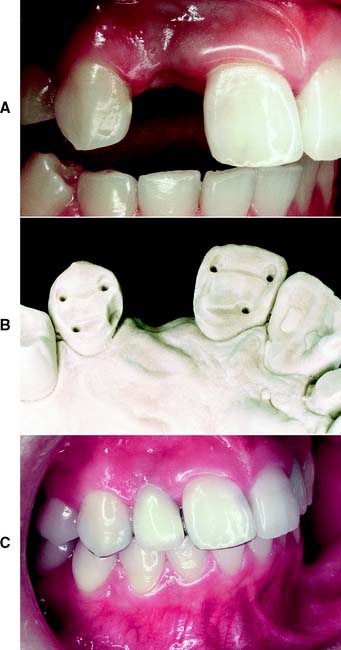
An unrestored, caries-free tooth is an ideal abutment. It can be prepared conservatively for a strong retentive restoration with optimum esthetics (Fig. 3-17). The margin of the retainer can be placed without modifications to accommodate existing restorations or caries. In an adult patient, an unrestored tooth can be safely prepared without jeopardizing the pulp as long as the design and technique of tooth preparation are wisely chosen. Certain patients are reluctant to have a perfectly sound tooth cut down to provide anchorage for an FDP. In these cases, the overall dental health of the patient, rather than the condition of each individual tooth, should be emphasized.
Mesially tilted second molar
Loss of a permanent mandibular first molar to caries early in life is still relatively common (Fig. 3-18). If the space is ignored, the second molar may tilt mesially, especially with eruption of the third molar. It then becomes difficult or impossible to make a satisfactory FDP, because the positional relationship no longer allows for parallel paths of insertion without interference from the adjacent teeth.
In such circumstances, an FDP is sometimes made with modified preparation designs or with a nonrigid connector, or a straightforward solution27 may be considered: uprighting the tilted abutment orthodontically with a simple fixed appliance. However, the problem can be avoided altogether if a space-maintainer appliance (Fig. 3-19) is fabricated when the first molar is removed. This device may be as simple as a square section of orthodontic wire bent to follow the edentulous ridge and anchored with small restorations in adjacent teeth.
Replacement of Several Missing Teeth
Fixed prosthodontics becomes more difficult when several teeth must be replaced. Problems are encountered in restoring a single long, uninterrupted edentulous area or multiple edentulous areas with intermediate abutment teeth (Fig. 3-20), especially when anterior and posterior teeth are to be replaced with a single fixed prosthesis. Underestimation of the problems involved in extensive prosthodontics can lead to failure. One key to ensuring a successful result is to plan the prostheses by waxing the intended restorations on articulated diagnostic casts. This is essential for complex fixed prosthodontic treatments, particularly when an irregular occlusal plane is to be corrected, the occlusal vertical dimension is to be altered, an implant-supported prosthesis is recommended, or a combination of fixed and removable prostheses are to be used. The precise end point of such complicated treatments can be far from evident, even to an experienced prosthodontist (see Fig. 2-39).
Overloading of abutment teeth
The ability of the abutment teeth to accept applied forces without drifting or becoming mobile must be estimated and has a direct influence on the prosthodontic treatment plan. These forces can be particularly severe during parafunctional grinding and clenching (see Chapter 4), and the need to eliminate them becomes obvious during the restoration of such a damaged dentition. Although it is hoped that a well-reconstructed occlusion will reduce the duration and strength of any parafunctional activity, there is little scientific evidence to support this. It is unwise to initiate treatment on the assumption that new restorations will reduce parafunctional activity, unless this has been demonstrated with treatment appliances over a significant period.28
Direction of forces
Whereas the magnitude of any applied force is difficult to regulate, a well-fabricated FDP can distribute these forces in the most favorable way, directing them in the long axis of the abutment teeth. Potentially damaging lateral forces can be confined to the anterior teeth, where they are reduced by the longer lever arm (see Chapter 4).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses