CHAPTER 3

PLANNING VENEERS
MACIEJ ŻAROW

Planning veneers
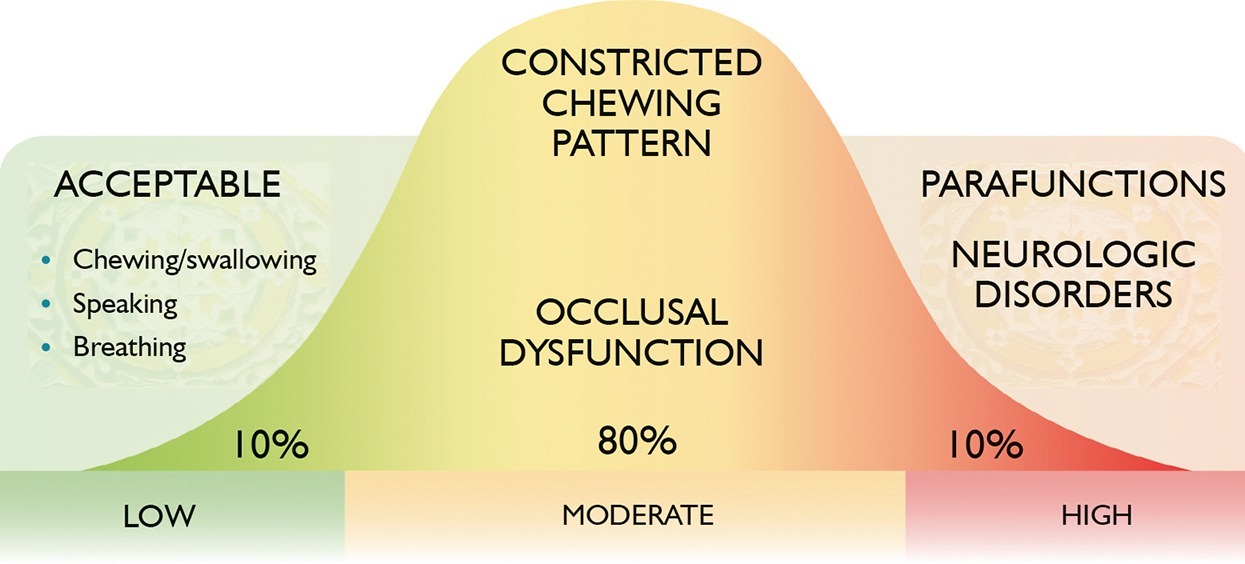
When porcelain veneer preparation is performed, it is important to achieve an “equilibrium” between minimizing the preparation of the tooth structure (which will ensure maximum adhesion through the presence of enamel), achieving the necessary mechanical strength (appropriate thickness), and esthetics. This can be achieved through appropriate treatment planning.
ADHESION, MECHANICAL RESISTANCE, AND ESTHETICS
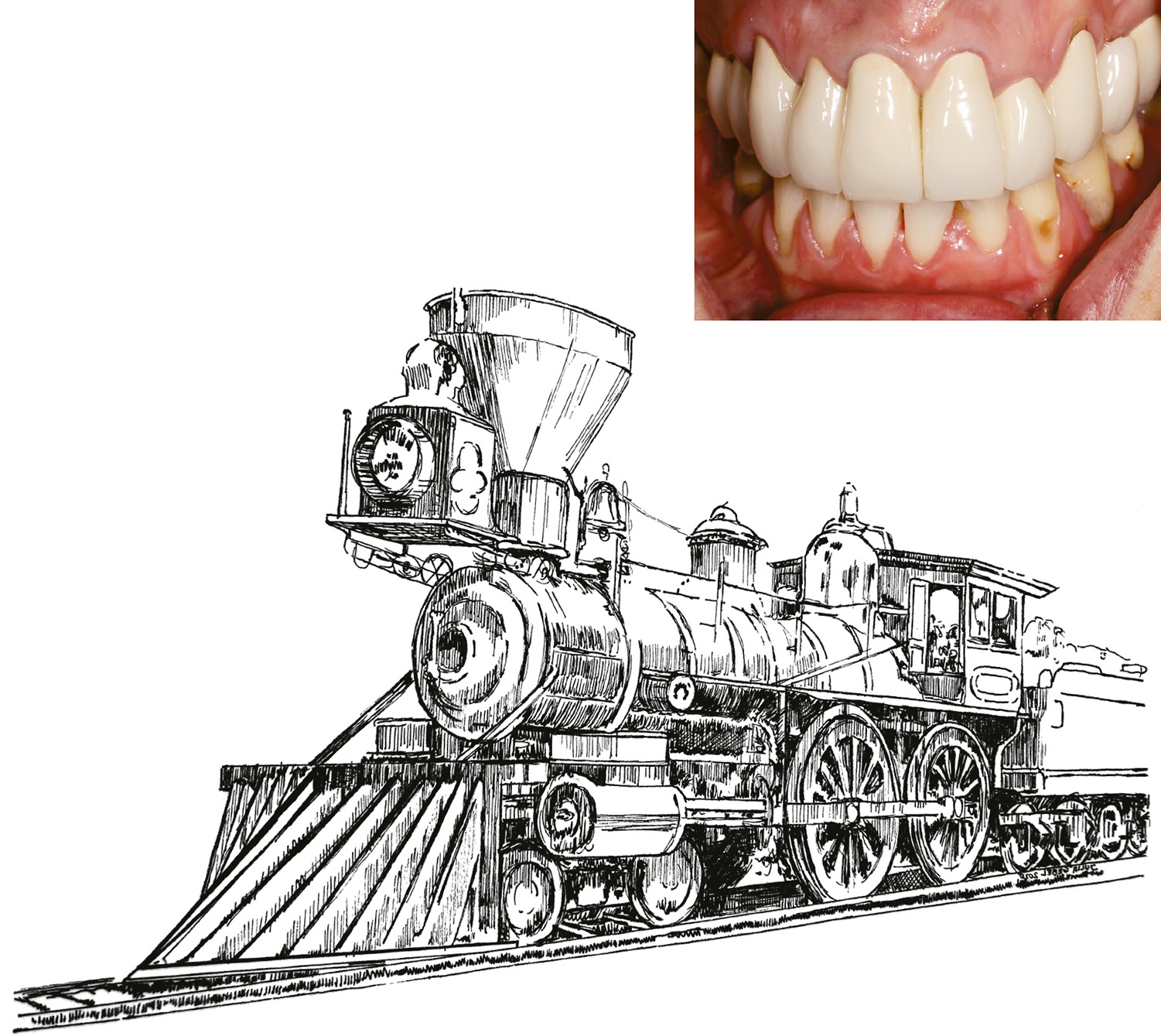
Planning the extension of veneer preparation is very important because their bonding to the tooth is purely adhesive, not retentive (Fig 3-1). If we prepare too little, the dental technicians will not have enough space for the restorative material, making them too convex, and the teeth will look like an off-road bumper or a locomotive from old times (Fig 3-2). To improve the shape, the dental technician would have to reduce the volume of the material from the labial surface, but this could also make the veneer too thin in some places and prone to cracking. However, if we prepare too much of the tooth, we will risk dentin exposure, which will weaken the veneer adhesion.1–4
Fig 3-1
When carrying out veneer preparation, ensure the conditions for maximum adhesion, mechanical resistance, and esthetics.
Fig 3-2
A poorly planned and disastrously performed prosthetic restoration. The teeth are too big, have an unnatural shape and resemble… … a locomotive from old times.
CONSULTATION VISIT
The consultation visit should include:
-
Thorough medical history
-
Clinical examination
-
Photographic documentation
-
Creating diagnostic wax-up
 Determining the needs, expectations, and risks related to the patient
Determining the needs, expectations, and risks related to the patient
First, you need to know the patient’s general health. How did they find the dental office? Who (if anyone) recommended it to them? What is the patient’s profession and their chief complaint? Are they satisfied with previous treatment? If not, why not? What expectations does the patient have of the initial visit? Answering these questions makes it possible to obtain information and create an initial patient profile (Fig 3-3).5–7
Fig 3-3
Favorable conditions for the first consultation: the right amount of time, a calm and quiet place allowing mutual trust to be established … this seems crucial in the extremely intimate path toward creating a patient’s smile. A short, hurried visit, the patient or dentist being late, disturbances, or unprofessional clinical staff members can ruin the first visit irreversibly.
A good solution is to present the patient with a questionnaire to be filled in during the first visit. This allows an assessment of the current condition of the oral cavity. The completed questionnaire is an excellent starting point for a clinical examination and treatment plan. Thanks to the information provided, the dentist does not have to take a scattergun approach to diagnosis that may make the patient uncomfortable. Rather, the dentist’s observations from the clinical examination may relate to the patient’s remarks in the questionnaire, which in turn can give the patient more confidence in the diagnosis.8
 Structural risk related to the loss of hard tooth tissue
Structural risk related to the loss of hard tooth tissue
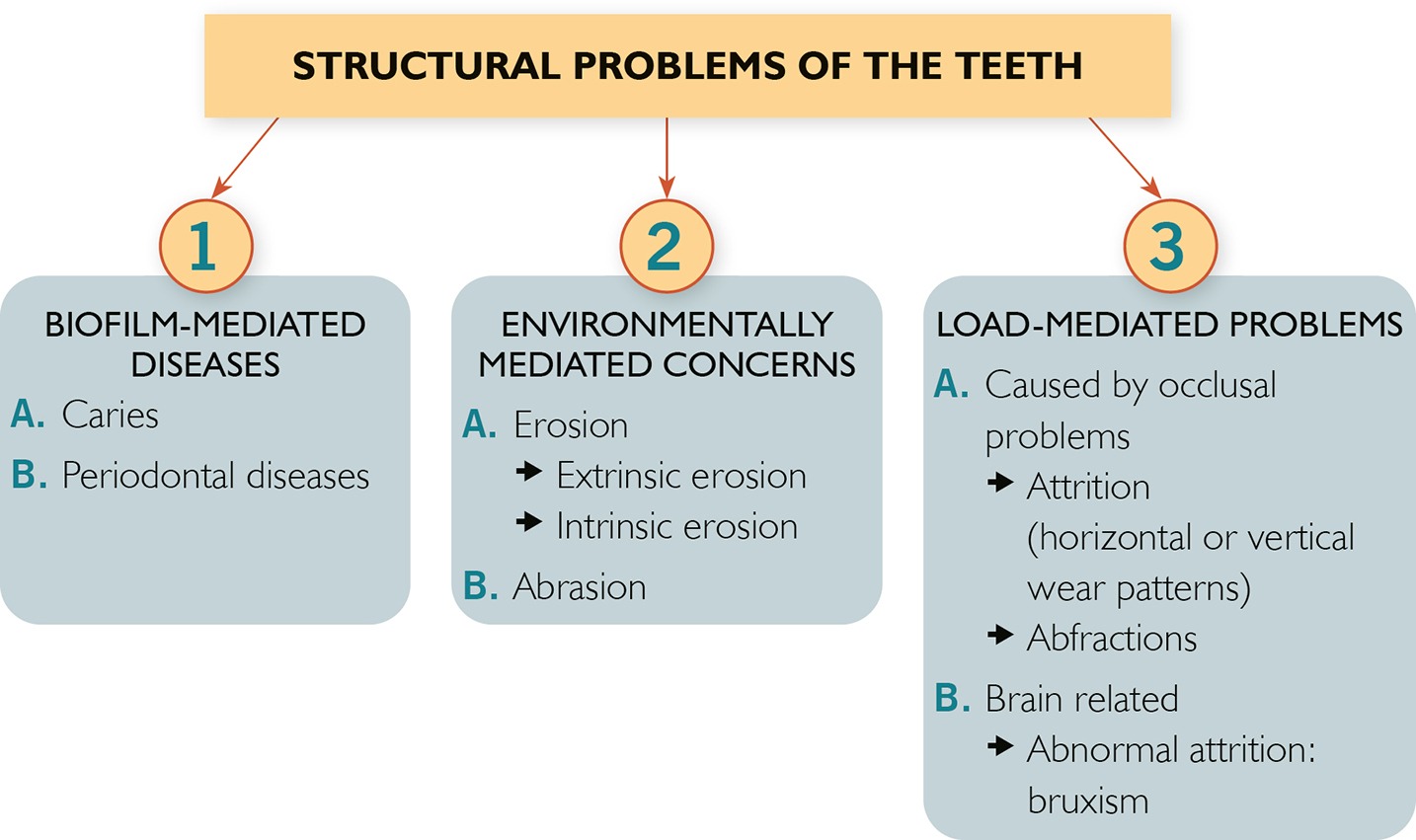
It is important to analyze the loss of tooth structure because the consequence of an unrecognized cause and lack of implementation of the prophylaxis/treatment may be a continuation of further hard tissues loss. This may have a negative impact on the long-term durability of restorative therapy, including veneers. The dentist/dental hygienist performing the dental examination should note any symptoms of tooth structure loss and ascertain their origin (Fig 3-4):
Fig 3-4
Structural risk depending on the cause: bacterial, environmental, or occlusal overload (according to Dr. John Kois).
- Structural loss related to biofilm-mediated diseases: caries result from a complex process of demineralization and remineralization of the enamel due to the exposure of organic acids produced by microorganisms living in the bacterial plaque.9
- Structural loss related to environmentally mediated concerns: erosion (hard tissue lesions caused by chemical processes, without cariogenic bacteria) (Fig 3-5) and abrasion (hard tissue lesions caused by physical wear by extraneous objects, such as hard bristle toothbrushes or excessively abrasive toothpaste; Fig 3-6).10–12
Fig 3-5a
Extrinsic erosion: a patient had a habit of consuming sauerkraut and pickled cucumbers every day. She was also fond of grapefruits and lemons. With a pH of around 2, these fruits represent a very high erosion risk factor.Fig 3-5b
Intrinsic erosion: a patient suffered from an eating disorder (bulimia), which caused erosion on the palatal side of the maxillary incisors (typical for intrinsic erosions) and resulted in rapid tooth wear of the incisal edges.Fig 3-6
Abrasion lesions on the buccal and cervical surfaces are related to many factors, such as hard-bristle toothbrushes, abrasive toothpaste, and a diet high in acids. - Structural loss related to environmentally mediated concerns: erosion (hard tissue lesions caused by chemical processes, without cariogenic bacteria) (Fig 3-5) and abrasion (hard tissue lesions caused by physical wear by extraneous objects, such as hard bristle toothbrushes or excessively abrasive toothpaste; Fig 3-6).10–12
If the patient is diagnosed with erosion, the origin must be determined: intrinsic erosion (gastroesophageal reflux disease, bulimia) or extrinsic erosion (diet including lemons, grapefruits, fruit juices, energy drinks, etc.).
 REMEMBER
REMEMBER
The dental hygienist has a specific scope of procedures, such as recording and documenting (with photographs) the presence of cavities and identifying their origin – bacterial, chemical, or mechanical. The desire for white teeth makes patients buy toothpaste recommended in supermarkets or TV advertisements. These often have unfavorable abrasive properties, especially when the dentin is already exposed. The dental hygienist should monitor what kind of toothpaste is used by each patient.13,14
The toothpaste abrasiveness ranked by recommended daily allowance (RDA) value:
- Low abrasive: RDA below 70
- Medium abrasive: RDA 70–100
- Highly abrasive: RDA 100–150
When extrinsic erosion is diagnosed, the focus should be on raising the patient’s awareness of their diet and its impact on the loss of tooth substance (Tables 3-1 to 3-4).15
Table 3-1 Acidity of common beverages and foods
| Beverage | pH range |
| Gatorade Orange | 2.99 |
| Clear American Tropical Fruit | 3.07 |
| Vitamin Water Zero Mega-C | 3.05 |
| S. Pellegrino Sparkling Natural Mineral Water | 4.96 |
| Perrier Carbonated Mineral Water | 5.25 |
| 24:7 Energy Cherry Berry | 2.61 |
| 180 Blue with Acai | 2.82 |
| Red Bull | 3.43 |
| Wine | 2.3–3.8 |
| Vinegar | 2.4–3.4 |
| Apples | 2.9–3.5 |
| Plums | 2.8–4.6 |
| Orange juice | 2.8–4 |
| Lemon juice | 1.8–2.4 |
| Raspberries | 2.9–3.7 |
| Mayonnaise | 3.8–4 |
| Coca-Cola | 2.48 |
| Pepsi-Cola | 2.60 |
Source: Kois Center (Seattle, USA)
Table 3-2 RDA value of certain products and toothpastes
| Toothpaste | RDA value |
| Water | 4 |
| Sodium bicarbonate | 7 |
| Carifree CTx3 Gel | 18.5 |
| Enamel Plus | 25 |
| Rembrandt | 53 |
| Colgate Cavity Protection | 65 |
| Sensodyne Extra Whitening | 104 |
| Aquafresh Triple Protection | 105 |
| Amway Glister | 110 |
| Aquafresh All Tartar Control | 110 |
| Crest Pro-Health Whitening | 168 |
| Colgate 2-in-1 Whitening | 200 |
Table 3-3 Enamel dissolution in mg/cm2
| Beverage | pH | 14-day weight loss (mg/cm2) |
| Coca-Cola | 2.48 | 2.78 |
| Pepsi-Cola | 2.60 | 3.07 |
| Sprite | 3.27 | 8.60 |
| Canada Dry Ginger Ale | 2.94 | 6.31 |
| Mountain Dew | 3.14 | 14.31 |
| Diet Mountain Dew | 3.17 | 14.82 |
Source: Kois Center (Seattle, USA)
Table 3-4 Main acids in common food products and beverages and their source
| Acid | Food product and beverages |
| Acetic acid | Products containing wine vinegar, pickled cucumbers |
| Ascorbic acid | Vitamin C lozenges, some beverages |
| Carbonic acid | Fizzy drinks |
| Citric acid | Lemon and fruit juices |
| Malic acid | Apples and apple juices |
| Tartaric acid | Grapes, grape juices, wine |
| Phosphoric acid | Soft drinks (such as Coca-Cola) |
Source: Kois Center (Seattle, USA)
When intrinsic erosion is diagnosed, we usually refer the patient for gastroenterological consultation or multi-specialized behavioral therapy (in the case of bulimia nervosa).
When diagnosing abrasion, we think about the harmful effect of hard bristle toothbrushes or abrasive toothpastes, which wear away the tooth substance, especially exposed dentin (see Table 3-2), and we recommend those that are appropriate for this clinical situation.
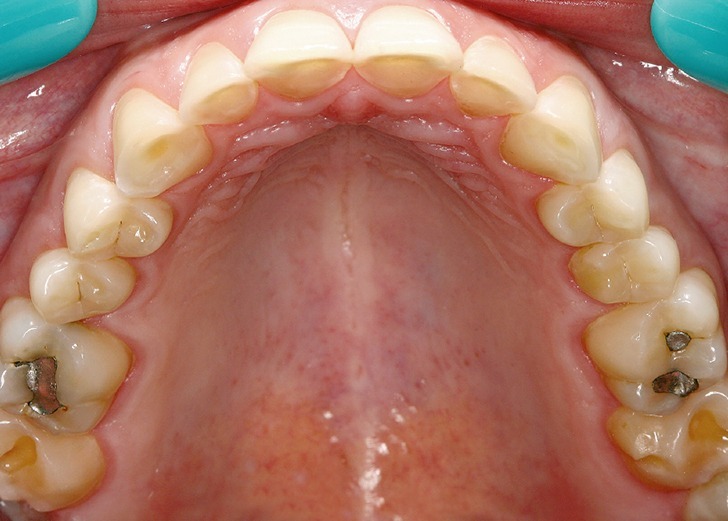
- Attrition: Mechanical wear resulting from mastication limited to contacting surfaces of opposing teeth (Fig 3-7).
Fig 3-7
Attrition: clear horizontal wear pattern is characteristic of occlusal dysfunction. The cause is usually the lack of bilateral simultaneous posterior occlusal support and a widened envelope of function leading to horizontal wear of the incisors. In this case, factors accelerating wear can include diet, too abrasive toothpaste with abrasive agents, or a hard-bristle toothbrush.
In the patient’s record, note the type of wear: whether it is horizontal or more vertical (typical “shelves of wear” are visible on the palatal surface of the maxillary incisors) and draw appropriate conclusions about this type of wear.16,17 It is also crucial to diagnose whether tooth wear is due to occlusal or neurological problems (such as bruxism; Fig 3-8). Suppose the patient has used an occlusal splint. In that case, it can be a useful tool to diagnose bruxism (patients diagnosed with bruxism usually leave characteristic transverse scratches on the splint, indicating nocturnal activity of the masticatory system).
Fig 3-8
Bruxism: a 22-year-old patient, despite his young age, has worn out a large part of the enamel of the posterior teeth. This was caused by clenching his teeth at night combined with an acidic diet.
- Abfractions: The pathologic loss of tooth substance in the cervical area can indicate premature contact on given teeth or other types of biomechanical loading forces, leading to cavities at the cementoenamel junction (Fig 3-9). An acidic diet, incorrect toothbrush movement while brushing teeth, too hard bristle toothbrushes, or abrasive toothpaste may deepen the abfraction.
Fig 3-9
Abfractions: a 21-year-old patient, predisposed to clenching his teeth during the day, presented to the dental office with numerous non-carious cervical lesions in the premolars and anterior teeth. Many abfractions were rapidly deepened due to an acidic diet and improper tooth brushing.
- Cracked tooth syndrome: The lines of the fracture in the posterior teeth usually run between the marginal ridges of the contact surfaces, with pain while biting down or temperature change; this may indicate pathological occlusal activity that led to the cracked tooth (Fig 3-10). The remaining teeth should be inspected, the cause should be found, and a plan for preventive (occlusal splint) or therapeutic measures developed (for example, physiotherapy or changing occlusal conditions – analysis of premature contacts, etc.).
Fig 3-10
Cracked tooth syndrome: a patient who worked in a highly stressful profession (stockbroker) ground his teeth during the day and night. The results are numerous initial cracks in the enamel of the posterior teeth. Cracked tooth syndrome was detected in tooth 17. The patient presented with pain upon temperature change and while biting down. A lithium disilicate overlay and an occlusal splint therapy were proposed.
Recent studies define the following risk groups for non-carious cervical lesions:18,19
- Group 1: Post-orthodontic patients (65% of patients under the age of 30)
- Group 2: Clenching habits – psychological effects of anxiety
- Group 3: Athletes – amateurs and professionals attending fitness clubs, gyms
- Group 4: GERD – gastroesophageal reflux disease and post-bariatric surgery patients
- Group 5: Drug users and/or illicit substances
 The risk of periodontal disease
The risk of periodontal disease
The examination of the current periodontal condition, measurement of the depth of the sulcus or the periodontal pocket, and radiological evaluation of the alveolar ridge level are crucial for maintaining the teeth.20,21
If there is periodontal disease, we start periodontal treatment or refer the patient to a periodontist. Even the presence of one gingival pocket with a depth greater than 5.5 mm places the patient in a high-risk group.22
Regular visits combined with removal and plaque control and the patient’s motivation are mandatory to prevent gum disease.21 Scientific research has confirmed that regular periodontal debridement carried out on patients between 20 and 30 years old reduces tooth loss after the age of 40.21
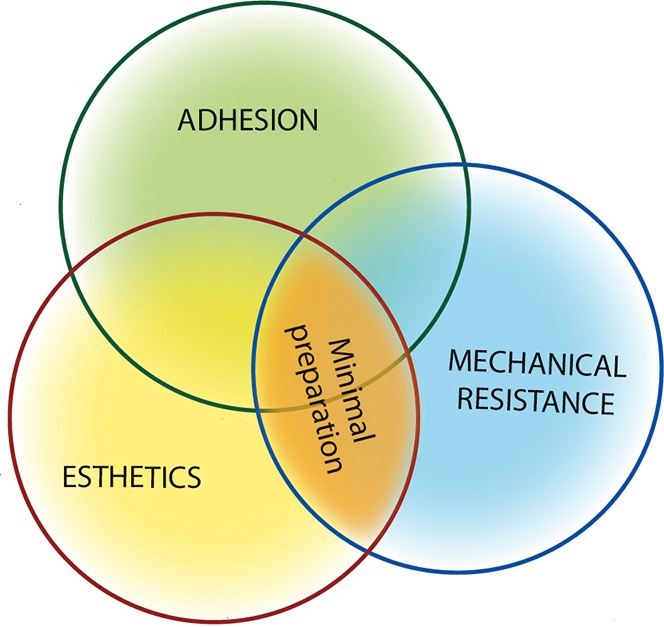
Functional risk assessment is an important step in the patient diagnosis before qualification for veneers, and inaccurate qualification may cause the rapid destruction of new reconstructions.23–28
Porcelain veneers can be planned when:
- There is no occlusal overload in the anterior teeth (when the palpation test is done, the fingertips placed on the anterior teeth do not detect vibration, symptomatic of fremitus) (Fig 3-11)
Fig 3-11
Fremitus is a symptom of occlusal overloading of a given tooth or group of teeth while closing in the centric relation or maximum intercuspation. The tooth vibration is felt when the index finger touches the tooth while closing the teeth. - There are no symptoms of tooth wear, or wear symptoms do not indicate an active, progressive process: according to Dr. John Kois, significant progress has been made in this respect in the last five years, unlike the situation that once led to tooth wear but has now stopped – ie, adapted patient
- There are no clear premature contacts that would change the path of closure of mandible, leading to destruction/overloading/tooth wear
- The patient does not report any pain or discomfort in the temporomandibular joints (TMJs). Basic examination of the joints includes:
- Examination of the vertical movement of the mandible – maximum opening (range of 35–60 mm)
- Examination of the horizontal movement of the mandible (average range of motion 8–10 mm, ie, slightly more than the width of the maxillary central incisor)
- Deviation during mandibular closure. The path of closure should be in a straight line. Use the facial midline as a reference to observe the course of deviation; the direction of the deviation goes toward the joint with the disorder
- Muscle pain during palpation
- Immobilization test: with the teeth held together, the patient tries to move the mandible in the horizontal direction (Fig 3-12a)
Fig 3-12a
Mandibular immobilization test: with the teeth held together, the patient tries to move the mandible in the horizontal direction against the hand of the dentist. - TMJ sounds evaluation during mandibular opening
- TMJ loading test in centric and eccentric relation (Figs 3-12b and 3-12c)
Fig 3-12b
The temporomandibular joint load test with lateral direction of force: the load force is directed on one of the TMJs, first the right and then the left (eccentric load test).Fig 3-12c
The temporomandibular joint loading test is used to identify if we are dealing with a healthy TMJ. Place cotton rolls between the teeth in the posterior region, and then press the chin toward the TMJs (centric load test). - TMJ loading test in centric and eccentric relation (Figs 3-12b and 3-12c)
Tenderness and pain during the test may also indicate disc displacement. The feeling of tension may suggest that the muscle contraction is persisting, which prevents the correct position of the condylar process in the mandibular fossa.27–29 In the case of a negative test, the pain symptoms are probably related to muscle problems – a Kois Deprogrammer is a good diagnostic and therapeutic tool.30 When the tests are positive, the appropriate initial treatment is occlusal splint therapy with support on all teeth (Michigan splint), and the patient’s TMJ should be monitored. If the symptoms persist, another therapeutic solution is a consultation with a physiotherapist or gnathologist. In the case of high functional risk, we will discuss the diagnosed problem with the patient and create a treatment plan that would allow veneers to be performed with reduced functional risk (Fig 3-13).
Fig 3-13
Functional risk assessment according to Dr. John Kois.
 TIP
TIP
The TMJs should be capable of transferring heavy loads without tenderness, tension, or pain in centric relation.
If the reaction in this case is positive, it means that the disc and complex process are not correctly aligned in the centric relation, and the joint should be examined more closely.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses









 TIP
TIP