Pharmacological behaviour management
Eduardo A Alcaino, Jane McDonald, Michael G Cooper and Simrit Malhi

Pain management for children
The proper treatment of pain in children is often inadequate and involves misconceptions that:
• Children experience less pain than adults.
• Neonates do not feel or remember pain.
• Pain is character-building for children.
• Opioids are addictive and too dangerous in terms of respiratory distress.
Development of pain pathways
Even premature neonates have the physiological pathways and mediators to feel pain. The statement that infants and children do not experience pain, either partially or completely, is not physiologically valid.
Measurement of pain in children
There are individual circumstances for each child that affect how they respond to pain and, subsequently, how that pain will be assessed. These include:
Observation of non-verbal cues and behaviour is important. A quiet, withdrawn child may be in severe pain. Simple measures are there to measure pain in children of all ages.
Methods for paediatric pain assessment include
Analgesia prior to procedures (pre-emptive analgesia)
Routes of administration
Analgesics
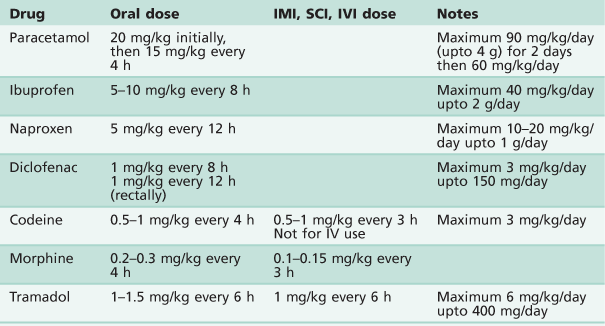
See Table 3.1.
Paracetamol
• Dosage 20 mg/kg orally, then 15 mg/kg every 4 h.
• 30 mg/kg rectally as a single dose.
• Useful as a pre-emptive analgesic.
• Intravenous paracetamol is available (10 mg/mL). The same dose is used and administered over 15 min.
• Take care with dosing, as many different strengths and preparations are available.
Non-steroidal anti-inflammatory drugs (NSAIDs)
• Effective alone after oral and dental procedures.
• May be used in conjunction with paracetamol.
• Have an opioid-sparing effect.
• Increased bleeding time due to inhibition of platelet aggregation.
• Useful analgesic once haemostasis has been achieved.
Contraindications for the use of NSAIDs in children
Aspirin
Ibuprofen
Codeine
Oxycodone
Morphine
Discharge criteria
Many drugs that are used for combination sedation and analgesia in children have a long half-life of several hours. Discharge criteria should be used to assess that the child is well enough prior to discharge from a free-standing facility. Criteria should include:
Local anaesthesia
The use of local anaesthesia in paediatric dentistry varies significantly between countries and there are also individual preferences. Every clinician must be proficient at administering painless local anaesthesia. While it is the mainstay of our pain control for operative treatment, it also represents one of the greatest fears in our patients. Use of many of the non-pharmacological techniques described in the previous chapter may enable the dentist to deliver an injection without the child being aware. There are few patients, old or young, who are not genuinely afraid of injections, and there are obvious disadvantages in the physical size of the dental cartridge syringe.
Techniques and tips
Need for local anaesthesia under sedation and general anaesthesia
Some form of pain control is required when invasive procedures are performed under any form of sedation (including inhalation sedation, oral sedation, etc.). However, the need for local anaesthetic under general anaesthesia is controversial. It is well recognized that a patient’s vital signs may change in response to painful stimuli (e.g. extraction), depending on the depth of anaesthesia. Local anaesthesia is not routinely used for extractions of primary teeth under general anaesthesia. Studies have observed that the child’s postoperative recovery is usually independent of the procedure performed, and preschool children waking after having a general anaesthetic can be more distressed by the sensation of numbness in the mouth. However, the use of local anaesthesia is recommended when removing permanent teeth, especially first permanent molars.
Complications with local anaesthesia
The most significant complication encountered is overdosage. Consequently, maximum doses (Table 3.2) need to be calculated according to weight and preferably written in the notes if more than just a short procedure is being performed. This clinical complication is highlighted in a paper that reviewed significant negative outcomes (death or neurological damage) in children due to local anaesthetic overdose (Goodson & Moore 1983).
Table 3.2
Maximum dosages for local anaesthetic solutions
| Anaesthetic agent | Maximum dose |
| 2% Lidocaine without vasoconstrictor | 3 mg/kg |
| 2% Lidocaine with 1 : 100 000 adrenaline | 7 mg/kg |
| 4% Prilocaine plain | 6 mg/kg |
| 4% Prilocaine with felypressin | 9 mg/kg |
| 0.5% Bupivacaine with 1 : 200 000 adrenaline | 2 mg/kg |
| 4% Articaine with adrenaline 1 : 100 000 (approximately 1.5 cartridge of 2.2 mL in 20 kg child) | 7 mg/kg |
Calculation of local anaesthetic dosage:
2% lidocaine = 20 mg/mL
2.2 mL/carpule = 44 mg/carpule
A 20 kg child (approximately 5 years old) can tolerate a maximum dose of 2% lidocaine with vasoconstrictor of:
7 mg/kg × 20 kg = 140 mg Equivalent of 3 carpules (6.6 mL)
Other complications include:
• Failure to adequately anaesthetize the area.
• Biting of the lower lip or tongue postoperatively.
• Facial nerve paralysis by injecting too far posteriorly into the parotid gland.
Consequently, adequate postoperative instructions to both children and parents are necessary to minimize these complications. In addition, inadequate local anaesthetic technique (inexperienced operator, fast delivery of solution and inadequate behaviour management) may jeopardize a successful outcome in an otherwise cooperative child. Allergic reactions to local anaesthetic solutions and needle breakage are rare in children.
The use of articaine with adrenaline has gained popularity recently. However, its safety and effectiveness in children under the age of 4 years has not been established. Finally, it is worth noting that there is significant evidence that inadequate local anaesthesia for initial procedures in young children may diminish the effect of adequate analgesia in subsequent procedures (Weisman et al. 1998).
Sedation in paediatric dentistry
The decision to sedate a child requires careful consideration by an experienced team. The choice of a particular technique, sedative agent and route of delivery should be made at a prior consultation appointment to determine the suitability of the child (and their parents) to a specific technique.
The use of any form of sedation in children presents added challenges to the clinician. During sedation, a child’s responses are more unpredictable than that of adults. Their proportionally smaller bodies are less tolerant to sedative agents and they may be easily over-sedated. Anatomically differences in the paediatric airways include:
• The vocal cords positioned higher and more anterior.
• Children have relatively larger tongue and epiglottis.
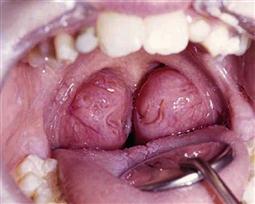
• Possible presence of large tonsillar/adenoid mass (Figure 3.2).
• Larger head to body size ratio in children.
• The mandible is less developed and retrognathic in younger children and infants.
Patient assessment
The preoperative assessment is among the most important factors when choosing a particular form of sedation. This assessment must include:
• Patient medical status (see ASA classification, below).
• History of recent respiratory illness or current infections.
• Fasting requirements and the ability of the carer to comply with instructions.
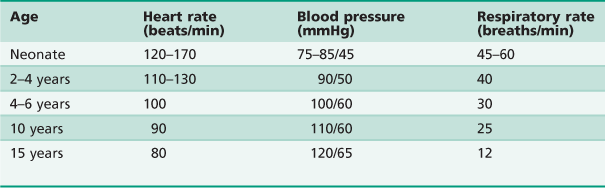
The clinician should be aware that children have resting vital signs that differ according to their age (Table 3.3).
The use of monitoring devices such as pulse oximetry is desirable for lighter sedation techniques and mandatory for moderate and deep sedation. While not currently mandated during relative analgesia, it is suggested that pulse oximetry should be used in all instances when a child is sedated. Sedation and anaesthesia is a continuum and any dentist who sedates children must be capable of resuscitating the patient from any level of sedation deeper than intended (Cote & Wilson 2006). Furthermore, regulations in each country, cultural and socioeconomic factors will determine whi/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses