3
Implant Surgery
INTRODUCTION
It is fair to say that the discovery and universal application of osseointegration has revolutionized the prosthodontic, surgical, and, increasingly, orthodontic rehabilitation of partially or fully edentulous patients, and in some cases, fully dentate patients. Although integration failure of implant devices occurs at very low rates, an implant that has not achieved osseointegration can certainly be considered a failure from a restorative or functional perspective. Fortunately, many complications that are associated with implant placement are considered reparable, even if it means removing the implant and starting over. However, failures sometimes can have devastating consequences on a patient’s (or surgeon’s) physical, psychosocial and financial well-being. This chapter will focus on the more commonly reported complications associated with dental implant surgery. Consideration will be given to (1) preoperative planning and the avoidance of complications during the treatment planning phase; (2) intraoperative contributions to integration failure and acute intraoperative complications; (3) early postoperative failures; and (4) late postoperative failures including peri-implantitis.
PREOPERATIVE PLANNING
Patient Assessment
There are many factors that are important to assess when evaluating a patient for implant reconstruction. Even before the actual clinical assessment is performed, the clinician should have a reasonable idea whether the patient is a good candidate for a successful outcome.
The patient’s ability to cooperate with treatment and subsequent hygiene and maintenance should be a primary concern when evaluating the patient for implant reconstruction. The immediate surgical outcome, although a concern, does not mean much if the patient does not possess the skills or understanding important to the long-term success of implant rehabilitation. Additionally, the patient’s expectations are key in determining whether or not the patient will consider his/her own treatment as a success.
There have been several systemic conditions cited in the literature that traditionally have been accepted as risk factors for integration failure. A number of articles cite specific conditions that are considered absolute or relative contraindications to implant placement. Typically these have included diabetes, osteoporosis, corticosteroid therapy, chemotherapy, and head and neck radiation.1 Recently, several outcomes studies have alluded to the fact that each of these indeed may not be contraindications, and that other factors, not normally included on that list, may be bigger contributors to failure. A study by Klokkevold and Han2 analyzed data from 35 articles that included failure rates in diabetic patients and smokers. The findings suggest that smoking significantly contributed to failure, but there was no difference for the diabetic patient. In a study reviewing 4,680 implants, Moy et al.,1 however, found that there was a significant increase in implant failure for the diabetic patient and the smoker. Also, additional conditions related to increased risk for failure included patients age greater than 60 years of age, head and neck radiation, and postmenopausal estrogen therapy. Conversely, gender, hypertension, coronary heart disease, pulmonary disease, steroid therapy, chemotherapy, and not being on hormone replacement therapy (in postmenopausal women) were all not associated with increased incidence of implant failure.
Although the literature supports the fact that there may not be any absolute contraindications to implant placement, the clinician needs to understand how certain systemic conditions may affect the integration of implants. This will help direct proper judgment with respect to treatment planning in patients with systemic diseases or disorders. For example, in the diabetic patient, decreased vascularity and circulation of the recipient bed due to microvascular abnormalities such as thickening of capillary basement membranes contribute to impaired wound healing, and abnormalities in neutrophil chemotaxis and phagocytic activity may make the diabetic more susceptible to infections.3 In the case of metabolic bone diseases (osteoporosis, hyperparathyroidism, Paget’s disease, etc.), one must consider the potential for proper mineralization that is important to integration.
In most instances, the literature does not distinguish the difference between implant failure and medical complications associated with implant placement.4 However, the clinician should differentiate the possible conditions that simply may cause implant failure versus conditions that may directly cause harm to the patient. For example, a patient who has had radiation to the jaws or has been treated with a potent bisphosphonate may be at risk for osteoradionecrosis or bisphosphonate-related osteonecrosis, respectfully, as well as implant failure. In these patients, “The option of implant therapy should be chosen restrictively, and the patient should be informed specifically, taking into account the current level of uncertainty with regard to the consequences.”4
In general, if a patient has the proper physical and mental attributes to maintain implants after restoration, has reasonable expectations, and can safely undergo the surgical procedure without putting undue risk on their physical well-being, they are a candidate for implant reconstruction. The informed consent discussion should be tailored to each patient, taking care to identify issues that may cause increased risk of failure or medical/physical risk to the patient.
Clinical Assessment of the Patient
Thorough clinical examination prior to implant treatment planning is imperative to assess not only the recipient site itself, but also to evaluate the patient’s current dentition and dental/gingival health, signs of parafunctional habits, malocclusion, or other factors that may be of importance with respect to implant failure. The clinician must keep in mind that the recipient site may be optimal for implant integration, but if the implant cannot be restored to proper function and aesthetics, then it may be deemed a failure.
The idea of placing implants in a patient with a history of periodontal disease has been a topic of controversy in the literature. Behind these studies, there exist several factors that make it difficult to compare outcomes. For example, each study may have different parameters with respect to the definition of periodontitis, the severity and treatment of periodontitis, the outcomes measures, the periodontal status at the time of placement, etc. Because of this variability, one cannot say for certain that a patient who experiences tooth loss due to periodontitis has a higher risk of developing peri-implantitis or integration complications.
Bruxism has been implicated in implant component fractures (implant platforms, abutment screws, implant bodies, etc.). Although no actual causal relationship exists, the general consensus in the literature recognizes an association between implant fracture and parafunctional habits. When developing an implant treatment plan for a patient with bruxism, the clinician should plan to minimize eccentric forces, eliminate cantilevers and potentially place additional implants to share the occlusal load (Fig. 3.1). When considering implant fracture, two other main causes have been implicated: manufacturing error and poor prosthetic fit.5 Although these factors also may contribute to implant fracture, they are much less cited when compared with parafunction. Implant fractures are commonly preceded by multiple incidents of broken abutment screws and bone loss, and may give the clinician an indication that there is an underlying problem. Balshi et al.5 performed an analysis of 4,045 implants placed in function for 5 years. He found eight fractured implants (0.2%). Six were supporting posterior prostheses, and all patients were diagnosed with parafunctional habits. Most of these patients also had preceding problems with loosening or fractured prosthetic or abutment screws prior to fracture.
Fig. 3.1. Implant platform fracture caused by over-torquing the final abutment. This implant required removal and replacement.

When examining the soft tissues surrounding the areas of interest, traditionally it was thought that there must be a proper amount of keratinized gingiva present for proper maintenance of implants. Recent studies, however, show that the amount of keratinized gingiva may only be a matter of cosmesis. There are no studies that show an increased loss of implants in areas of inadequate (<2 mm) keratinized mucosa. Kim et al.6 suggest that there may be an increased risk of gingival recession and marginal bone loss in areas of deficient keratinized mucosa, but this does not necessarily cause adverse effects unless it is in the aesthetic zone and aesthetics are affected. Schrott et al.7 reported similar findings as part of a prospective 5-year follow-up study of patients who underwent edentulous reconstruction with a fixed, mandibular implant prosthesis. They found that plaque accumulation and bleeding upon probing on the lingual surfaces were greater in patients with less than 2 mm of keratinized mucosa surrounding the implants. Buccal soft tissue recession was also reported to be greater over a 5-year period in patients with inadequate keratinized gingiva. These studies may suggest that patients with inadequate keratinized mucosa around implants may have greater challenges with hygiene leading to subsequent periodontal issues that may or may not impact the overall success of the reconstruction.
Bone quality has been implicated as one of the most important factors for initial implant osseointegration, but is unfortunately difficult to evaluate preoperatively and it is a factor that cannot be changed prior to surgery. It is widely accepted that Misch type 2 and 3 bone is the most favorable for initial osseointegration,3 but many times, the surgeon may be faced with type 1 or 4 bone at the time of surgery, even if the patient has a fairly normal anatomic and radiographic examination. Sometimes it is not difficult to predict based on the patient’s presentation. For instance, a patient with a severely atrophic mandible will most likely have nearly all cortical bone in the anterior mandible. Surgeons need to familiarize themselves with these presentations to make adjustments for bone quality. For instance, a tapered implant may be preferred, healing time may be extended, or a two- versus one-staged procedure may be indicated.
Prosthodontic and Surgical Treatment Planning
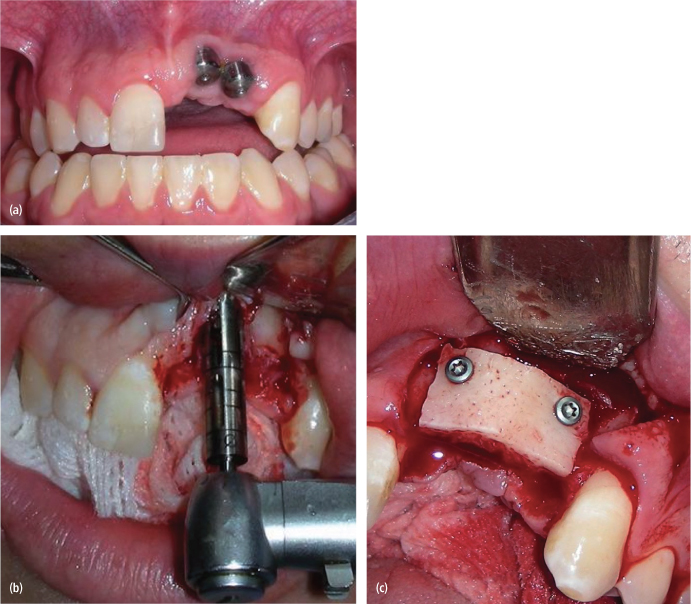
Implant reconstruction treatment planning is a team concept. The restorative dentist and surgeon must both provide input for a successful outcome. Failure to include the restorative dentist in the treatment planning phase could lead to prosthodontic failures because of unrestorability of the implant due to location, angulation problems, or aesthetic failures. Both parties should communicate their preferences with respect to implant location. Many times it is helpful when the restorative dentist provides a surgical guide to assist with implant location and angulation [Figs. 3.2(a)–(c)]. Surgical guides are not always necessary depending on the location of the implants and the skill of the surgeon but can be very helpful for complex cases and aesthetic zone cases, especially those involving multiple implants. Recently, there has been great attention paid to computer-aided treatment planning, surgical guide fabrication, and computer-guided surgery. Currently, there exist no clinical trials indicating the superiority of such techniques. There may be some benefit of obtaining CT imaging when treatment planning sites that may have significant anatomic limitations, but in general, most of the information provided on the CT scan can be obtained by a good clinical examination, mounted models, and plane radiography.
Fig. 3.2. (a) Immediate implant placed too facial and too apical. These implants are integrated, but are esthetically nonrestorable. (b) Implant removal with a trephine. (c) An onlay/veneer graft was placed to facilitate proper placement of the implants.
(Courtesy of James Q. Swift, DDS)
Treatment planning not only addresses location of implants but also time between extraction and implant placement, time to implant loading, and time to final restoration. All of these factors may play a role in the initial integration and implant stability. The alveolar ridge undergoes hard and soft tissue dimensional change after tooth extraction. Several studies have looked at the amount of bone loss that occurs over time after extraction. These studies show a loss of horizontal width between 30 and 50% at 3 to 12 months after extraction.8–11 Immediate and early implant placement has become an accepted technique to attempt to offset this anatomical change. However, Boticelli et al.,12 placed 21 immediate implants in 18 patients, and upon re-entry at 4 months found resorption of the bone around the implants: approximately 50% on the buccal plate and 30% on the lingual. Covani13 found similar outcomes and concluded that immediate implant placement cannot prevent resorption in the alveolar process. Although these studies suggest that bony resorption continues to take place regardless of when the implant is placed after extraction, there is no evidence to suggest that early or immediate placement techniques have a significantly lower rate (or higher rate) of integration success as those placed in a more delayed fashion. The author acknowledges, however, that more clinical studies need to be done in a randomized fashion with clearly defined long-term outcomes to help guide treatment strategies.
Timing to loading of implants is also well debated in the literature, and presumably has an effect on the overall success of implant integration. Jokestad and Carr14 performed a systematic review of the literature examining timing to loading of implants. Only 22 papers were thought to be adequate for inclusion in the study. Due to the heterogeneity, variable clinical applications, variable outcomes, and lack of quality of evidence, the authors could not make a definitive conclusion. They stated that the average outcome was in favor of delayed loading, but there are no indications that immediate or early loading cannot be a safe procedure. With so many variables to consider (bone quality, type of implant, timing of implant placement relative to extraction, patient factors, prosthetic plan, stability of implant at time of insertion, etc.), one cannot, at this point, prove any superiority to any one loading plan.
Another factor to consider with respect to timing of implant placement and loading includes the augmented ridge or sinus. Aghaloo and Moy15 performed a systematic review of the literature to determine which hard tissue augmentation procedures are the most successful in furnishing support for implant placement. The study included 90 articles that were acceptable for data extraction and analysis. Regarding sinus augmentation, the authors found that sinus augmentation with allogeneic/nonautogenous composite grafts had the best retention for implants (93%). Autogenous grafts were a close second at 92%, followed by alloplastic />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


