CHAPTER 3 ESSENTIAL SYSTEMS FOR TEAM TRAINING IN THE DENTAL IMPLANT PRACTICE
After the root-form implant was introduced into the United States in 19831 a generalized separation of duties specific to practice type developed. Initially, oral surgeons and then periodontists were the primary sources of surgically placed implants. In most cases, the restorative dentist referred implant candidates to these specialists, who sent them back to the restorative dentist for prosthetic completion after the surgical phase. Unfortunately, the initial lack of prosthetic training made completion of implant cases frustrating for surgical and restorative dentists, as well as for the patients. Although this trend has been significantly remedied with the increasing prevalence of implant prosthetic courses and literature, widespread confusion continues about how the surgical and prosthetic offices can best work together for the seamless completion of implant cases. In other practices, the prosthetic dentist does both surgical and restorative procedures.
Whatever the mechanism for case completion, the office staff must become an integral part of implant education, procedures, and follow-up.2 Without the support of the entire team reinforcing the dentist’s recommendations, developing an implant practice can be very difficult if not impossible.
 Four Presurgical Phases
Four Presurgical Phases
Implant case development usually involves a joint effort between the restorative and surgical offices, facilitated by a protocol for interdisciplinary treatment planning. The following four phases are recommended for analyzing the prospective implant patient’s options for treatment and then delivering them to the patient.3
All dental team members must be cognizant of this presurgical planning system. They must understand why it is important to properly plan the case and how to carry out these phases in a professional and organized manner.4
Diagnostic Work-up
The patient who presents with a need for tooth extraction(s) or is already edentulous in any area qualifies as an implant candidate. This can be determined at an initial appointment with a visual exam and radiographs. The patient is then advised that a diagnostic work-up is needed to properly analyze the case and develop an appropriate treatment plan.5
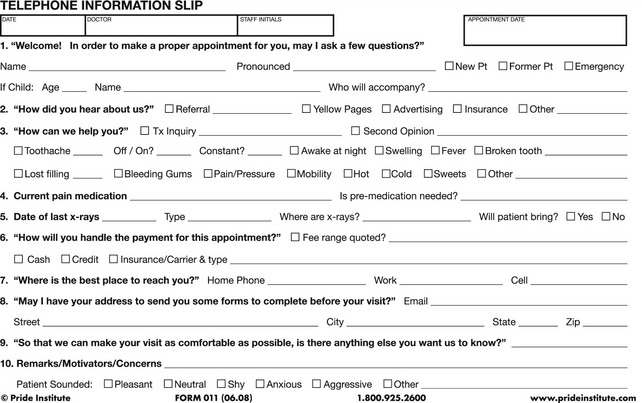
From the first patient contact with the office by phone, email, or other means, each team member should have a working understanding of how the patient is to be guided through an educational process that will allow the patient to make an intelligent decision about treatment. The new patient calling to inquire about dental implants will be scheduled for a limited exam with x-rays, typically one or more periapical radiographs of a specific area and a panoramic radiograph. A preprinted form is used by the scheduler as a guide for gathering pertinent information (Figure 3-1). The appointment coordinator schedules this appointment and sends a health history and other pertinent administrative information to the patient to complete and bring to the appointment. The dentist then examines the area of concern and determines whether the case can be appropriately treated using implants. Additional diagnostic information is recommended, leading into the diagnostic work-up. Once the patient agrees to proceed, the work-up can be completed at the first appointment or scheduled for a later date.
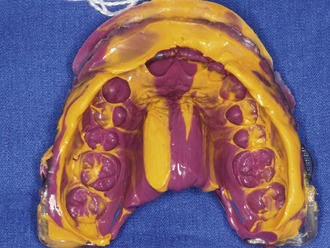
In addition to the necessary and appropriate radiographs, maxillary and mandibular diagnostic impressions are made using vinyl polysiloxane (VPS) impression material. VPS impression material is preferred over alginate impression material because it facilitates pouring of multiple stone casts. Fast setting (2 to 3 minutes) medium-viscosity VPS works very well to capture the detail needed for a diagnostic impression. If significant undercuts exist or if the dentition is periodontally mobile, extra-light-viscosity material is syringed into these areas with medium-viscosity material used in the impression tray. The extra-light material will usually pull out of the undercuts without danger of disrupting the teeth or existing restorations (Figure 3-2). In severe cases of undercuts and/or mobility some form of block-out material should be placed. A bite registration is then made, either in the patient’s acquired maximum interdigitation or in centric relation.
A series of photos are taken to document the patient’s existing condition (Figure 3-3). Additional digital photographic views may be helpful in thoroughly analyzing the case. The dentist or assistant may be aided by taking courses in dental photography or reading the existing literature on the techniques and equipment needed to acquire these images.6,7
The final part of the diagnostic work-up consists of a discussion with the patient regarding goals and expectations. Open-ended questions such as “What would you like to change about your existing smile and teeth?” tend to be the most helpful. In many cases, the patient wants a brighter smile, straighter teeth, closed spaces between teeth, or some other aesthetic improvement. Others may simply want the improved function that implants present by changing from a conventional denture to an over-denture or hybrid appliance. The patient’s responses to these types of questions can provide invaluable information. Because this is a rapport-building period, it is important for the clinician to listen. Let the patient talk as much as is possible to gain insight into exactly what he or she desires; there will be plenty of time later on to go into specifics about the details associated with treatment plan options. Active listening can be used here not only to display genuine interest and concern but also to verify that you understand what the patient is saying.8
Laboratory Procedures
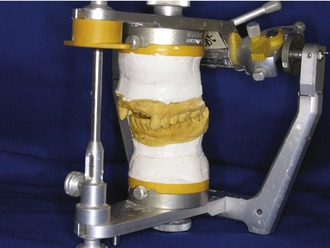
In working up the treatment plan, the restorative dentist will produce diagnostic casts from the preliminary impressions and mount them on a semi-adjustable articulator. Subsequent working models will be mounted on this same articulator for consistency and comparison with the preoperative condition. From the facebow transfer, the maxillary model can be mounted on the upper member of the semi-adjustable articulator (Figure 3-4). The mandibular model is mounted on the lower member of the articulator using the centric bite registration.
The semi-adjustable articulator and facebow transfer procedures facilitate the accuracy of all restorative procedures. In general, this is because the case can be mounted closer to the true arc of closure of the mandibular teeth relative to their interdigitation with the maxillary teeth.9 This principle of restorative dentistry, although always important, is particularly essential when opening the vertical dimension of occlusion (VDO). Having the models track on, or very near to, the arc of closure will reduce the occlusal adjustment needed upon delivery of these types of cases. In many instances, the VDO is opened in patients who have used partial or complete dentures for many years or who exhibit worn dentition. The mounted casts are reviewed along with the radiographs, photos, and chart notes including pertinent periodontal measurements. One of the valuable insights gained from the mounted casts is the determination of how much inter-arch space is available to the proposed implant restoration.
Treatment Planning Conference
The presurgical checklist is used to guide case analysis whether a surgical dentist is involved in the case or both surgical and prosthetic procedures are being performed in-house. When the case involves an interdisciplinary effort with the surgical dentist, duplicate mounted diagnostic casts, radiographs (FMX and/or panoramic), pertinent chartings, and patient-specific notations are sent to the surgical office. A form is useful to deliver a brief description of the purpose for the evaluation (Figure 3-5). The restorative dentist may need to discuss any specific issues or concerns about the case with the surgeon prior to the surgical evaluation appointment. Under this scenario, the two principal clinicians (surgical and restorative) either meet face to face or arrange a scheduled />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses