Chapter 3. Diagnosis
S. Patel and B.S. Chong
SUMMARY
Diagnosis is the first step in the care and management of any patient. A systematic and organized approach is important in order to avoid misdiagnosis. Special test and additional investigations may be necessary to help confirm a provisional diagnosis. Until and unless a clear diagnosis is possible, invasive and irreversible treatment may have to be delayed. However, once a confirmed diagnosis has emerged, in conjunction with the patient, the various treatment options can then be considered. Depending on patient’s preference, a treatment plan is formulated and then carried out to resolve the patient’s complaint. Referral to a specialist may, sometimes, be necessary to help establish a diagnosis or if complex endodontic treatment is required.
INTRODUCTION
Diagnosis is the process of identifying a disease or an abnormal condition by collecting and evaluating the patient’s presenting signs and symptoms, and the results of further investigations. A clear diagnosis can only be reached when information is collected systematically and interpreted accurately. Without a correct diagnosis, the clinician will not be able to manage and provide appropriate treatment to resolve the patient’s complaint. If a diagnosis cannot be reached, irreversible treatment may have to be delayed. The maxim ‘first do no harm’ is a reminder it may be better to do nothing than something that risks causing more harm than good. If a diagnosis cannot be established, a referral to an appropriate specialist should be considered.
HISTORY
Taking an accurate history from the patient is the first step in diagnosis. The clinician can then decide the direction the diagnostic process should take, for example, the additional investigations or special tests required. Subject to confirmation, a tentative diagnosis may be possible at this stage.
As well as helping to establish the reasons for the patient’s attendance, the history may also reveal the patient’s attitude and motivation towards dental treatment. The clinician may be alerted to potential patient management problems, for example, if the patient mentioned previous difficulties in achieving adequate anaesthesia or an intolerance to having dental instruments in the mouth.
Presenting complaint
Patients should be questioned sympathetically and asked to describe their complaint in their own words; this should then be documented. Their cooperation and ability to describe their complaint accurately will greatly aid diagnosis. The questions asked should be open ended and not leading, for example, ‘What brings you to see me today?’ With endodontic problems, pain and/or swelling are usually the predominant complaints. Typically with pain, a series of follow-up questions is necessary to help establish the character, duration, severity and other features of the pain or discomfort (see Chapter 2, Table 2.1).
History of presenting complaint
Often, the presenting complaint is not new but previous symptoms may have been mild or they may have temporarily abated. The patient may be unaware that treatment is required or may have even chosen to ignore the problem, especially if no longer causing symptoms. However, a historical perspective and the chronology of the presenting complaint are still necessary as it will provide relevant information for arriving at a diagnosis.
Dental history
It is helpful to gain an insight into the patient’s past and present dental history including pattern of attendance. Some patients may only attend when they are in pain, whilst others may see their dentist on a more regular basis. It is also important to determine if the patient has recently had dental treatment in the region of interest because unless it is purely coincidental, it may be related to the presenting complaint. Other relevant snippets of information gleaned from the dental history may provide clues to possible factors contributory to the patient’s complaint. For example, a history of dental trauma may explain symptoms of irreversible pulpitis associated with an otherwise clinically unremarkable tooth.
Medical history
An up-to-date medical history is required. Unless already documented, normally the patient is requested to complete a medical history form beforehand, which the clinician will then go through with the patient. It is imperative to ascertain if there are any medical conditions or medications that the patient may be taking, which may alter their dental management. In addition, patients should be asked if they are allergic to latex (rubber dam and rubber gloves), household bleach (sodium hypochlorite) and iodine; materials they will be in contact with during endodontic treatment. The subject of the patient’s general health and potential impact on endodontic treatment is covered in Chapter 2.
EXAMINATION
Extraoral
The patient’s general well-being and demeanour will be noticeable during consultation. Signs of facial asymmetry, swelling and/or trismus may also be apparent (Fig. 3.1). However, less obvious signs may only be revealed following closer examination. The lymph glands, temporomandibular joint and muscles of mastication are assessed. The degree of mouth opening possible should also be noted because if limited, access for endodontic treatment may be hindered.
 |
| Figure 3.1
An extraoral swelling and associated facial asymmetry that will be obvious upon meeting the patient.
|
Intraoral
Soft tissues
The general state of the soft tissues should be assessed. Scalloping of the lateral borders of the tongue and/or frictional keratosis of the buccal mucosa may indicate a parafunctional habit. The area of interest requires more detailed assessment (see later). Signs, such as a swelling or the presence of a sinus tract should be noted (Fig. 3.2).
 |
 |
| Figure 3.2
(A) Clinical view of the buccal sinus tract associated with a maxillary central incisor. (B) Periapical radiograph of tooth showing an overextended and sub-optimal root canal filling.
|
Hard tissues
The dentition, including the state and quality of existing restorations is assessed; this will provide an overall clinical view of the patient’s dental history (Fig. 3.3). Combined with the oral hygiene status, general periodontal probing profile and caries experience, these are relevant when devising a treatment plan.
 |
| Figure 3.3
The state of the dentition will provide an overall clinical view of the patient’s past dental history.
|
If evident, the severity and distribution of tooth surface loss should be recorded. Localized wear facets and fracture lines may indicate an occlusal component to the patient’s symptoms (Fig. 3.4). If a cracked tooth is suspected it may be necessary to assess individual cusps by occlusal loading (see later). Transillumination, using a light source placed on the side of the tooth may help reveal otherwise hard to detect fracture lines (Fig. 3.5). Special dyes, such as methylene blue (Vista-Blue, Vista Dental Products, Racine, WI, USA) may also be used to highlight a fracture line once its approximate position is known. In general, the use of magnification and enhanced illumination greatly aid visualisation allowing a detailed examination (see Chapter 6).
 |
| Figure 3.4
Excessive generalised tooth surface loss in this mandibular left second molar has resulted in pulpal symptoms.
|
 |
| Figure 3.5
Transillumination using a fibreoptic light.
|
Specific tooth/teeth
The area of interest and specific tooth/teeth are assessed in more detail. The occlusion and the strategic nature of the tooth are considered, for example, if a tooth is unopposed or non-functional. The colour of the tooth, should be compared with adjacent teeth; any darkening of the clinical crown may be related to a history of trauma. 1 The possible causes of pulpal or periapical diseases are noted, for example, the presence of primary or secondary caries (Fig. 3.6), fracture lines (Fig. 3.7) and extensive dentine exposure due to tooth surface loss. The restorability of the tooth must be assessed. The extent of any caries, the size of existing restorations and the amount of original tooth substance left will provide an indication about restorability; there is further discussion on this subject later.
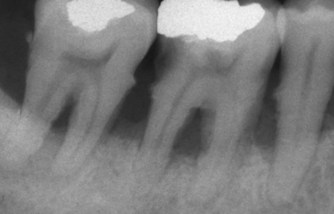
 |
| Figure 3.6
A large carious cavity in a maxillary right first molar. The clinical picture suggested possible pulpal involvement and the need for endodontic treatment.
|
 |
| Figure 3.7
A mandibular right first molar with stained crack lines and an old amalgam restoration that is leaking, with evidence of secondary caries underneath.
|
Palpation
The buccal/labial and palatal/lingual mucosa are palpated. Light finger pressure is applied in a rolling motion on the soft tissues using, normally, an index finger (Fig. 3.8). Signs of tenderness usually indicate inflammation of the underlying tissue.
 |
| Figure 3.8
Light finger pressure is applied in a rolling motion to palpate the soft tissues.
|
Percussion
Teeth are percussed in an axial and buccal direction using a forefinger (Fig. 3.9) or the end of a mirror handle. Tenderness to gentle percussion indicates inflammation of the periodontal ligament surrounding the tooth; this may be of pulpal or periodontal in origin.
 |
| Figure 3.9
Tooth percussion performed using a forefinger.
|
Mobility
With fingers or combined with a mirror handle, any abnormal tooth mobility should be noted. Common causes of increased mobility include periodontal disease, root fracture and acute apical periodontitis.
Periodontal probing
Probing depths should be assessed by ‘walking’ the periodontal probe around the entire circumference of the tooth (Fig. 3.10). The probing profile for root fractures and iatrogenic perforations is, characteristically, an isolated localised loss of attachment. Whereas loss of attachment due to periodontal disease is usually more generalised and not associated with a singular defect. Furcation involvement may indicate advanced periodontal disease (Fig. 3.11) or an iatrogenic root perforation.
 |
| Figure 3.10
The periodontal probe must be walked around the tooth to ensure that any isolated narrow periodontal defects are not missed.
|
 |
| Figure 3.11
Advanced periodontal disease.
|
INVESTIGATIONS
Pulp sensitivity tests
Currently available sensitivity tests assess the neural response, and not the vascular supply of the pulp, the assumption with these tests is that the neural status reflects the blood supply status of the tooth. 2,3 With any sensitivity test, an explanation should be given to the patient about the rationale for the test. Otherwise, particularly with an anxious patient, false positive responses will result. An adjacent tooth, considered healthy, should be tested first; this will act as the control and allow the patient to experience the likely response.
Thermal tests
Cold test
Cold thermal tests work by causing contraction of the dentinal fluid within the dentine tubules; this rapid outward flow of movement results in ‘hydrodynamic forces’ acting on the Aδ nerve fibres. 4,5 There is a sharp sensation, lasting for up to a few seconds after the cold stimulus has been removed from the tooth. 6 Several types of cold tests are available; the main difference between them is the operating temperature.
Ice sticks (0°C) are made by filling discarded, sterilized local anaesthetic needle covers with water and placing them in the freezer. They have the advantage of being inexpensive and easy to prepare. However, false negative responses can occur as a result of water droplets contacting adjacent teeth and gingivae, as the ice melts. Commercially available refrigerant spray containing tetrafluoroethane (−50°C) is convenient and easy to use. It is sprayed onto a small cotton pellet and then applied to the tooth (Fig. 3.12). Carbon dioxide snow (−78.5°C) is also very effective. Carbon dioxide is expressed into a plunger mechanism from a pressurised gas cylinder, and then compressed into a stick of carbon dioxide snow. This is then placed on the tooth to be tested using a special applicator. Being the coldest, carbon dioxide snow is particularly useful for assessing teeth restored with full coverage restorations.
 |
| Figure 3.12
Cold thermal test; a refrigerant is sprayed on a small cotton pellet and applied to the tooth.
|
Teeth may also be isolated individually with rubber dam, and then bathed with cold water. This test is a particularly useful test when a patient is complaining of a poorly localized pain provoked by cold (Fig. 3.13). The colder the applied stimulus the more reliable the test as there is a greater temperature reduction within the dentine-pulp complex. 7,8 This is important in posterior teeth as the thickness of both dentine and enamel is greater than that in anterior teeth. A negative response may be because the applied stimulus is not cold enough. A prolonged and lingering response usually indicates irreversible pulpitis. Cold tests appear to be more effective in assessing nerve status than heat tests. 9,10
 |
| Figure 3.13
A tooth is isolated with rubber dam and bathed with cold water; this is repeated for each tooth in the quadrant to try to reproduce the patient’s symptoms.
|
Heat test
Heat may be applied to a tooth using a heat-softened gutta-percha stick. A thin layer of petroleum jelly should first be applied to the test surface to prevent the gutta-percha sticking to the tooth. Another way of applying heat to a tooth is by running a rubber prophylaxis cup dry, in a slow handpiece, to generate frictional heat on the crown of the tooth11 but this method is seldom used; a false positive response may be obtained because of the vibrations, and particularly if the patient is anxious.
Individual teeth may also be isolated with rubber dam and warm water applied. Again, this test is particularly useful when the patient complained of poorly localized heat sensitivity. Prolonged application of heat to a tooth can result in stimulation of C-fibres, resulting in lingering pain. 12 For testing purposes and for this reason, heat should only be applied to a tooth for a maximum of 5 seconds. 3
Electric pulp test
Electric pulp testers (EPTs) are battery operated units (Fig. 3.14). They produce negative pulses of electricity, with a maximum current of a few milliamperes. The current can be adjusted; it is either controlled by the operator or it increases automatically when the unit is activated. 13 The tooth to be assessed is isolated with cotton wool and dried. Depending on the EPT, the patient is asked to hold the handle of the probe, or a lip hook is placed, to form one loop of the circuit. The tip of the probe is usually coated with a conducting medium (e.g. toothpaste) to improve electrical transmission to the tooth. When the probe is placed onto the tooth (Fig. 3.14), the circuit is complete. If desired, strips of rubber dam or cellulose strips may be used interproximally to reduce the likelihood of electrical conduction to adjacent teeth. 3
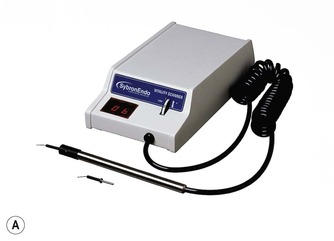 |
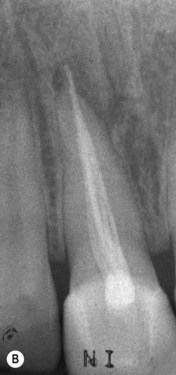
 |
| Figure 3.14
(A) A typical electric pulp tester. (B) The probe is placed on the incisal third of the crown of the tooth; toothpaste is used to help improve conduction.
|
As the test proceeds, the strength of the electrical stimulus will increase and when sensation is elicited, the patient is advised to either let go of the handle of the probe which breaks the circuit, or signal to the clinician so the probe may be removed. The reading on the EPT, either numerical or arbitrary is then recorded. If numerical, the digital readout is relative rather than an accurate quantitative measurement of the health status of the pulp. Apart from a total lack of response suggesting a lack of vitality, EPT readings are merely an indication, a comparative measurement as healthy teeth will respond over a range of values. The threshold for obtaining a positive response depends on the position of the probe on the tooth and the thickness of the enamel and dentine. The probe of the EPT should be placed adjacent to the pulp horn as this is where there is the highest density of nerves. In the case of anterior and posterior teeth this is at the incisal and mid-third region of the tooth respectively14.15. and 16. (Fig. 3.14). The thicker the enamel and dentine, the higher the excitation threshold; for this reason, the probe should be placed where the enamel is thinnest. 17 This explains why for a given test, the excitation threshold increase from incisor to premolar to molar teeth as the thickness of the overlying enamel and dentine increases. 12,18
A tingling or warm sensation indicates a healthy ‘positive’ response. This is a result of Aδ nerve fibres being stimulated, resulting in an ionic shift in the dentinal fluid causing a localized depolarisation and the generation of an action potential from the healthy nerve. 19 A lingering, dull ache following the removal of the EPT probe is a result of stimulation of the C-fibres, which is indicative of irreversible pulpal inflammation. No response from electric pulp testing indicates that the tooth is non-vital, i.e. the pulp is necrotic. Saliva conduction through the periodontal ligament may result in a false positive reading; a negative response may also be due to the failure to complete the electrical circuit. A review on electric pulp testing was published recently; 20 included is the important reminder that electric pulp tests can be unreliable, especially in the case of immature and concussed teeth.
A study to evaluate the ability of thermal and electrical tests to register pulp vitality2 reported that the probability of a non-sensitive reaction representing a necrotic pulp was 89% with the cold test, 88% with the electrical test and 48% with the heat test. It also indicated that the probability of a sensitive reaction representing a vital pulp was 90% with the cold test, 84% with the electrical test and 83% with the heat test. The results of this study would suggest that, in descending order of accuracy: the cold test followed by the electrical test and then the heat test.
Test cavity preparation
Historically, test cavity preparation has been suggested as a technique to assess the pulp status when all other tests are inconclusive. Local anaesthetic is not administered and a small bur is used with copious irrigation to prepare a small cavity down the centre of the tooth into dentine. 21 If the patient feels sensitivity, this may indicate that the tooth is vital; alternatively, it may indicate that the tooth is unhealthy as Aδ fibres may still be viable in necrotic pulp tissue. No response indicates a lack of pulpal vitality. However, if the pulp tissue has receded away from the centre of the tooth and an excessive amo/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


